Last Updated on December 3, 2025 by Bilal Hasdemir

Leukemia is a major concern in pediatric oncology. It’s the top cancer in kids. Every year, about 4,000 kids in the U.S. get it. One in three kids with cancer has leukemia. Examining the statistical peak for the Childhood leukemia age distribution in young children.
Knowing when kids usually get leukemia is key. It helps doctors catch it early and treat it well. Studies on leukemia diagnostic trends and childhood cancer epidemiology have found when most kids get it.
Looking at blood disorder age patterns and youth medical statistics helps us understand more. It shows us how leukemia affects kids worldwide and in the U.S. This knowledge is important for kids’ health.
Key Takeaways
- Leukemia is the most common cancer type among children.
- Approximately 4,000 children are diagnosed with leukemia each year in the U.S.
- One in three children with cancer has leukemia.
- Understanding age patterns is key for early detection.
- Recent studies have found when most kids get leukemia.
Understanding Childhood Leukemia

It’s important to understand childhood leukemia to improve treatment and outcomes. Leukemia is a cancer that affects the white blood cells. These cells are key to our immune system.
What Is Leukemia in Children?
Leukemia in kids happens when the bone marrow makes too many bad white blood cells. This can cause problems like anemia, infections, and bleeding. Acute lymphoblastic leukemia (ALL) is the most common type in kids, making up about 80% of cases.
How Childhood Leukemia Differs from Adult Leukemia
Childhood leukemia is different from adult leukemia in several ways. For instance, ALL is more common in kids, while chronic lymphocytic leukemia (CLL) is more common in adults. Also, childhood leukemia grows faster, needing quick treatment.
- Different types of leukemia are more prevalent in children vs. adults.
- Childhood leukemia often requires more aggressive treatment.
- The impact of leukemia on children’s development and long-term health is a significant concern.
Common Misconceptions About Childhood Cancer
There are many misconceptions about childhood cancer, including leukemia. Some think childhood cancer is always fatal or caused by the environment. But, the truth is that childhood cancer is a complex disease with many causes and risk factors.
Knowing the facts about childhood leukemia helps us support kids and families. It’s important to understand the risk factors and symptoms of leukemia. Also, keeping an eye on pediatric health monitoring and developmental disease tracking is key.
Childhood Leukemia Age Distribution: The Complete Picture
Knowing the age when childhood leukemia strikes is key for treatment. It’s the top cancer in kids and shows different patterns based on the type.
Peak Incidence Ages
Acute Lymphoblastic Leukemia (ALL), the most common type, hits hardest between 2 and 4 years old. Acute Myeloid Leukemia (AML) can happen at any age but is more common in the very young and teens.
Statistical Breakdown by Age Groups
Childhood leukemia falls into different age groups. Here’s a statistical look:
| Age Group | ALL Incidence | AML Incidence |
| 0-2 years | Low | High |
| 2-8 years | High | Low |
| 9-18 years | Moderate | Moderate |
Global vs. U.S. Age Distribution Patterns
Though global patterns vary, U.S. data aligns with international trends. Studies in childhood cancer epidemiology show ALL peaks between 2 and 4 years globally, mirroring U.S. findings. Yet, genetic and environmental factors lead to some differences.
Grasping these leukemia diagnostic trends and oncological age distribution is vital. It helps in creating focused treatments and bettering youth medical statistics.
Types of Childhood Leukemia and Their Age Patterns
Childhood leukemia is not just one disease. It’s a group of blood disorders with different age patterns. Knowing these differences is key for diagnosing, treating, and studying pediatric oncology.
Acute Lymphoblastic Leukemia (ALL) Age Distribution
Acute Lymphoblastic Leukemia (ALL) is the top leukemia in kids, hitting its peak between 2 and 4 years old. It makes up about 80% of all childhood leukemia cases. The age when ALL strikes affects treatment and how well kids do.
Acute Myeloid Leukemia (AML) Age Patterns
Acute Myeloid Leukemia (AML) is less common than ALL but affects different ages. It’s more common in very young kids and teens. AML’s occurrence is spread out, with peaks in infancy and late teens.
Chronic Leukemias in Children
Chronic leukemias, like Chronic Lymphocytic Leukemia (CLL) and Chronic Myeloid Leukemia (CML), are rare in kids. They’re more common in older kids and teens. These leukemias grow slower than acute ones.
Rare Subtypes and Their Age Associations
There are other rare leukemias, like Mixed Phenotype Acute Leukemia (MPAL) and Juvenile Myelomonocytic Leukemia (JMML). These have unique age links and symptoms. They need special treatments.
Knowing the leukemia type and age pattern is vital. It helps manage cancer risk factors and improve childhood disease progression outcomes.
Why Age Matters in Childhood Leukemia
Age is very important in childhood leukemia. It affects how doctors treat the disease and how well the child might do. Knowing a child’s age is key to managing their health.
Impact of Age on Treatment Protocols
How doctors treat childhood leukemia changes with the child’s age. Babies under one and kids over ten often need stronger treatments. This is because their leukemia can be more aggressive. Doctors use the oncological age distribution to make treatment plans that fit each age group.
| Age Group | Typical Treatment Approach |
| Infants (<1 year) | High-intensity chemotherapy |
| Children (1-10 years) | Standard chemotherapy protocols |
| Adolescents (>10 years) | More aggressive treatment, potentially including clinical trials |
Age as a Prognostic Factor
The age a child is when they are diagnosed is very important. Kids between 1 and 9 usually do better than babies or older kids. This shows how important it is to track how a child’s disease is developing.
Developmental Considerations Across Age Groups
Every age group has different needs when it comes to treating childhood leukemia. For example, teenagers might need more help with their feelings and social life because of treatment. This is why developmental considerations are so important.
Watching how a child’s disease progresses means understanding these age-related needs. By recognizing the role of age in treatment and prognosis, doctors can give more tailored care. This helps kids get better and stay healthy.
Risk Factors for Childhood Leukemia Across Different Ages
It’s important to know the risk factors for childhood leukemia. This knowledge helps in early detection and treatment. Factors like genetics, environment, and age play a role in leukemia development.
Genetic Predispositions
Genetic conditions like Down syndrome and Li-Fraumeni syndrome raise leukemia risk. These conditions can make cells more likely to become cancerous.
Key genetic risk factors include:
- Down syndrome
- Li-Fraumeni syndrome
- Neurofibromatosis type 1
Age-Related Risk Variables
Leukemia risk changes with age in children. Acute Lymphoblastic Leukemia (ALL) is common in kids aged 2-5. Acute Myeloid Leukemia (AML) can happen at any age but peaks differently.
Prenatal and Early Life Exposures
Prenatal and early life exposures increase leukemia risk. Maternal infections and ionizing radiation are examples. Knowing these risks helps in prevention.
Examples of prenatal and early life exposures include:
- Maternal infection during pregnancy
- Exposure to ionizing radiation
- Pesticide exposure
Recognizing Leukemia Symptoms at Different Ages
It’s important to know the symptoms of leukemia in kids at different ages. This cancer affects the blood and bone marrow. It shows up in different ways in children of different ages. Knowing this helps find and treat it early.
Infant-Specific Symptoms (0-2 years)
Leukemia in infants is hard to spot because the symptoms are not clear. Babies might have fever, look pale, and bruise easily. Pediatric health monitoring is key here, as these signs can mean many things.
Toddler and Young Child Symptoms (3-6 years)
Kids aged 3 to 6 might show clear signs like being very tired, not wanting to eat, and hurting in their bones. Watch for these signs, as they can mean childhood disease progression.
School-Age Child Symptoms (7-12 years)
Kids in school might get sick a lot, bruise easily, and look pale. These signs can point to leukemia diagnostic trends. It’s important to see a doctor right away.
Adolescent Symptoms (13-18 years)
Teenagers might feel tired, lose weight, and sweat a lot at night. Knowing youth medical statistics helps doctors spot leukemia in teens.
Spotting these age-specific symptoms is key to catching leukemia early in kids. By knowing the signs for each age, parents and doctors can work better together. This helps kids with leukemia get the best care.
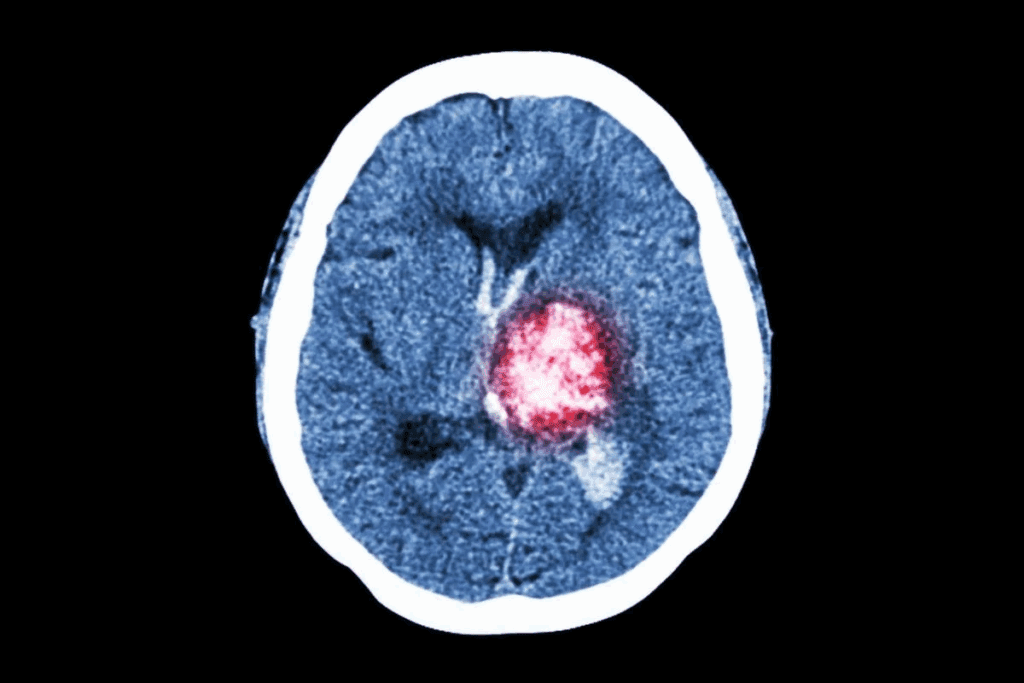
Diagnosis Process for Childhood Leukemia
Diagnosing childhood leukemia is tough. It needs a detailed approach, starting with initial screening and advanced tests. The process has several steps to find out the type and how severe the leukemia is.
Initial Screening and Tests
The first step is a physical check and a complete blood count (CBC). This checks for odd levels of blood cells or platelets. More tests are needed to confirm the diagnosis.
Age-Specific Diagnostic Considerations
Diagnosis changes with age. For example, babies with leukemia might have different genetic signs than older kids. Knowing these age-specific details is key for a correct diagnosis.
Advanced Diagnostic Techniques
Tests like flow cytometry, cytogenetics, and molecular diagnostics help find the exact leukemia type. These tests are vital for planning treatment.
The Role of Genetic Testing
Genetic testing is very important in diagnosing leukemia. It finds specific genetic problems. This info helps in diagnosing, predicting outcomes, and customizing treatments.
In summary, diagnosing childhood leukemia is complex. It involves initial screening, age-specific factors, advanced tests, and genetic testing. These steps help get an accurate diagnosis and guide treatment plans.
Treatment Approaches Based on Age
Age is key in finding the best treatment for kids with leukemia. It’s all about matching the treatment to the child’s age and disease type.
Infant Treatment Protocols
Infants with leukemia need special treatments because of their unique bodies and aggressive disease. They often get strong chemotherapy.
Treatment for Children Ages 1-9
Kids in this age group usually do well and get a mix of chemotherapy and sometimes targeted therapy. The goal is to keep side effects low.
Adolescent Treatment Considerations
Teenagers with leukemia face unique challenges, like more aggressive diseases. Their treatments mix adult and pediatric approaches, using both.
Emerging Therapies for Different Age Groups
New treatments like immunotherapy and precision medicine are being tested. They aim to make treatments safer and more effective for all ages.
The world of pediatric oncology is always growing. Research on oncological age distribution and childhood disease progression leads to better treatments. Advances in leukemia diagnostic trends also help shape these approaches.
Survival Rates and Prognosis by Age Group
Childhood leukemia survival rates have greatly improved over time. But, age is a big factor. Today, survival rates range from 80% to 90%, showing how far treatment has come.
Statistical Outcomes Based on Age at Diagnosis
Survival rates change a lot with age. Kids between 1 and 9 years old usually do best. Some studies say they have a 90% chance of survival.
| Age Group | Survival Rate (%) |
| 0-1 year | 70-80 |
| 1-9 years | 85-90 |
| 10-18 years | 75-85 |
Long-term Outlook Considerations
For kids with leukemia, survival is just the start. Long-term survivors might face treatment side effects. These can include secondary cancers, organ problems, and mental health issues.
“The improvement in survival rates for childhood leukemia is a testament to advancements in medical science and the dedication of healthcare professionals. Yet, the journey doesn’t end with treatment; long-term care is key.”
Quality of Life After Treatment
Survivors of childhood leukemia worry about their quality of life. This depends on their age, type of leukemia, and how intense the treatment was.
Late Effects by Age Group
Late effects differ by age. Younger kids and teens face unique challenges. Knowing these effects helps doctors give better care.
- Increased risk of secondary cancers
- Organ dysfunction (e.g., heart, kidneys)
- Psychological and social challenges
Understanding survival rates, long-term outlook, and late effects by age helps doctors. They can then tailor care to meet each child’s needs. This boosts their chances of a happy, healthy life.
Supporting Children with Leukemia at Different Developmental Stages
When a child is diagnosed with leukemia, their family faces many challenges. These challenges change a lot based on the child’s age and developmental stage. It’s important to support these children in many ways, including their medical, educational, and psychological needs.
Age-Appropriate Communication About Diagnosis
Telling children about their leukemia diagnosis needs to be done in a way that fits their age. Younger kids need simple and reassuring words. Older kids and teens might want more detailed information. Honesty and clarity are key in helping children understand their condition.
Educational Support Across Age Groups
Leukemia can affect a child’s education a lot. Educational support should match the child’s age and developmental stage. This ensures they keep learning and growing academically and socially. Individualized education plans can really help.
Psychological Interventions by Developmental Stage
Psychological support is very important for children with leukemia. It helps them deal with the emotional side of their diagnosis and treatment. The support should be tailored to the child’s age, from play therapy for younger kids to more complex therapy for teens.
Family Resources and Support Networks
Families of children with leukemia also need help. They should have access to counseling, support groups, and educational materials. Building a strong support network is key for families dealing with childhood leukemia.
By giving the right support and resources, children with leukemia and their families can handle the challenges of diagnosis and treatment better. This improves their overall well-being and quality of life.
Conclusion: Understanding the Age Factor in Childhood Leukemia
It’s key to understand how age affects childhood leukemia for early detection and better treatment. The age when leukemia is diagnosed changes a lot, affecting how we study and treat it. This is important for kids’ health.
The age when leukemia strikes, risk factors, and how it affects kids are all important. Knowing this helps doctors create the best treatment plans for each child. This way, kids get the care they need at their age.
Parents and doctors need to work together to help kids with leukemia. They should use age-friendly ways to talk, teach, and support kids’ mental health. This helps kids do well during and after treatment.
More research is needed to understand leukemia better. This will help us find even better ways to treat it. It will also help more kids survive and live well after treatment.
FAQ
At what age is leukemia most commonly diagnosed in children?
Leukemia is most often found in kids between 2 and 8 years old. The highest number of cases is in those aged 2-5, mainly for acute lymphoblastic leukemia (ALL).
How does the age distribution of childhood leukemia vary by type?
The age when leukemia is found changes with the type. ALL is most common in kids aged 2-8. AML can happen at any age, but is more common in very young kids and teens.
What are the risk factors for childhood leukemia, and how do they relate to age?
Several things can increase a child’s risk of getting leukemia. These include genetic factors, environmental exposures, and things that happen before birth. Knowing these risks helps find kids at higher risk, across different ages.
How does age impact treatment decisions and prognosis for childhood leukemia?
Age is very important in treating leukemia in kids. Younger than 1 or older than 10 often face a tougher fight. Treatment plans are made to fit the child’s age and disease.
What are the symptoms of leukemia in children, and how do they vary by age?
Symptoms of leukemia change with age. Infants and young kids might show signs like fever, being pale, and bruising. Spotting these symptoms early is key to treating it fast.
How is childhood leukemia diagnosed, and what role does genetic testing play?
Diagnosing leukemia in kids involves several steps. This includes initial tests, age-specific checks, and advanced techniques. Genetic tests are very important for finding specific genetic issues.
What are the treatment approaches for childhood leukemia, and how do they vary by age?
Treatment for leukemia in kids is customized based on their age and disease. Young and older kids might need special treatments. New treatments offer hope for better results.
What is the long-term outlook for children diagnosed with leukemia, and how does age impact survival rates?
Survival rates for leukemia in kids vary by age. Some ages have better chances than others. Knowing the long-term outlook and possible late effects is key to full care.
How can families and healthcare professionals support children with leukemia at different developmental stages?
Supporting kids with leukemia means using age-appropriate ways to talk, educate, and help their mental health. It’s also important to have family support and networks.
References:
- Puckett, Y. (2023). Acute Lymphocytic Leukemia. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK459149/