Last Updated on December 3, 2025 by Bilal Hasdemir
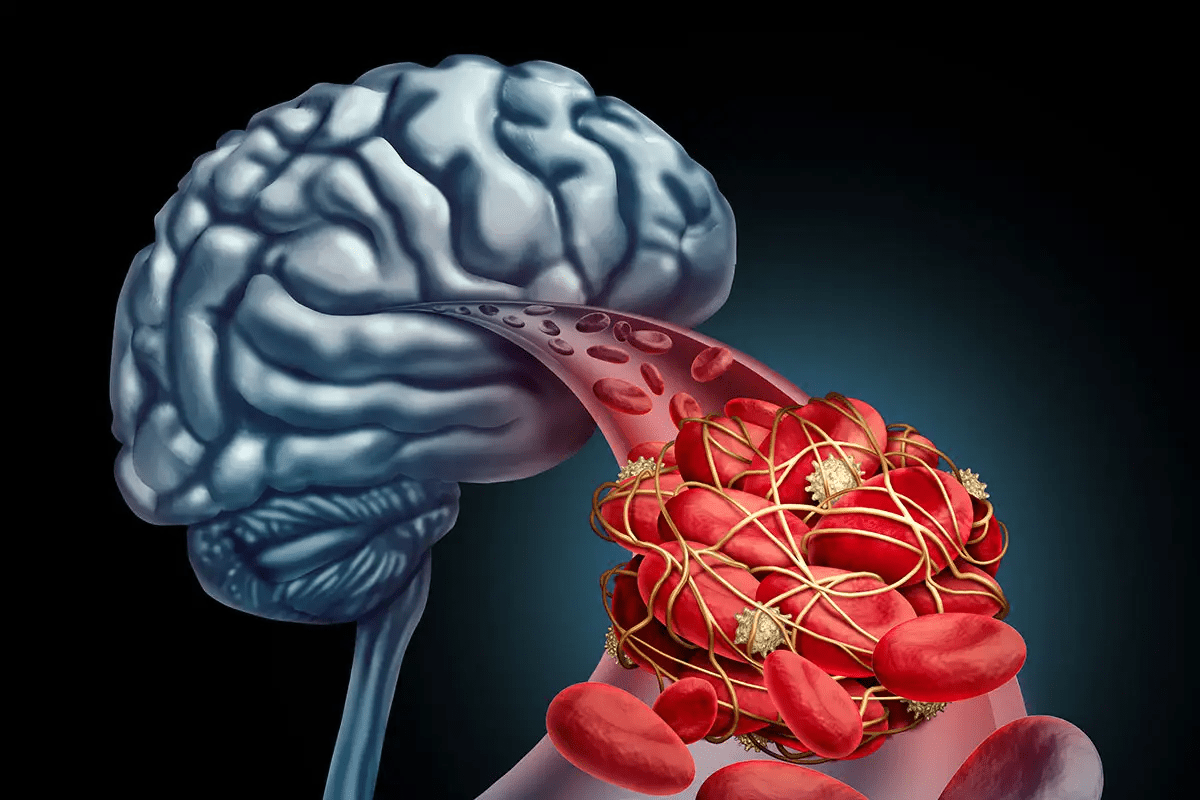
Diffuse intrinsic pontine glioma, a rare and aggressive brain cancer, affects about 300 kids in the U.S. each year.
We face a tough reality: a diagnosis that is often a death sentence. DIPG is located in the pons of the brainstem. This area controls many vital functions of the body.
It’s important to understand the causes and research on DIPG. This is key for finding better treatments and helping families with this childhood cancer.
Key Takeaways
- DIPG is a rare and aggressive brain tumor that mainly affects children.
- The exact cause of DIPG is not known, but research is ongoing.
- Symptoms can vary, but often include trouble with speech, swallowing, and coordination.
- Treatment options are limited, and the prognosis is generally poor.
- Understanding DIPG is vital for developing effective treatments and support.
What is DIPG Cancer?
DIPG, or Diffuse Intrinsic Pontine Glioma, is a very aggressive brain tumor. It starts in the pons, a key part of the brainstem. This cancer is known for its fast growth and is classified as a diffuse midline glioma, H3 K27M-mutant.
Definition and Classification of Diffuse Intrinsic Pontine Glioma
DIPG is a brain cancer that comes from the brain’s glial tissue. It’s called a diffuse intrinsic pontine glioma because it grows in the pons of the brainstem. This makes it hard to treat.
The World Health Organization (WHO) has updated how they classify DIPG. Now, it’s seen as a diffuse midline glioma, H3 K27M-mutant. This change is important because it shows the tumor’s genetic makeup. Knowing this helps doctors find new treatments.
DIPG vs. Other Pediatric Brain Tumors
DIPG is different from other brain tumors in kids. It’s located in a hard-to-reach area and has a unique genetic profile. This makes it hard to remove surgically without harming the brain.
DIPG is also very aggressive and has a poor outlook. This sets it apart from other brain cancers in kids. While some tumors can be treated well, DIPG is a big challenge. It needs more research and new treatments.
We know DIPG is a tough diagnosis for families. By understanding it better, we can see why we need more research. We also need new ways to treat it.
The Anatomy and Location of DIPG
It’s important to know where Diffuse Intrinsic Pontine Glioma (DIPG) is in the brain. DIPG is found in the pons. This part of the brainstem is key for many important body functions.
The Pons of the Brain and Its Critical Functions
The pons is a main part of the brainstem, along with the midbrain and medulla oblongata. It helps control breathing, swallowing, and sleep. It also connects different brain parts, helping them talk and work together.
The pons does many important things, like:
- Regulating sleep and wakefulness
- Managing swallowing and other cranial nerve tasks
- Helping signals move between the cerebrum and cerebellum
Why the Brainstem Location Makes DIPG Particulary Challenging
DIPG’s spot in the pons makes treating it hard. Surgery here is very tricky and often not possible.
Here are some reasons why:
| Challenge | Description |
| Surgical Risks | Brainstem surgery can lead to serious problems. |
| Limited Access | Getting to DIPG in the brainstem is hard. |
| Critical Functions | The pons handles vital tasks, making it risky to operate. |
Knowing these challenges helps us find better ways to treat DIPG. We’re always looking for new ideas to tackle this tough condition.
Epidemiology of DIPG Cancer in Children

DIPG cancer in children is rare and aggressive. It mainly affects kids. Knowing about DIPG’s spread helps plan better care and research.
Studying DIPG’s spread is key. It helps us see how big the problem is. It also points out risk factors and trends for prevention and research.
Age Distribution and Incidence Rates
DIPG mostly hits kids aged 5 to 9. It’s rare, but common in brainstem tumors in kids. This makes it a big worry in pediatric oncology.
The number of DIPG cases is steady, but low. It’s about 1-2 cases per million kids each year. This shows we need more care centers and research for DIPG.
Demographic Patterns in DIPG Occurrence
Research shows DIPG can happen to any child. But, some studies hint at slight differences in rates among ethnic groups. More study is needed to confirm this.
Knowing who gets DIPG helps find causes. It also helps make sure all kids get the care they need, no matter their background.
In short, studying DIPG in kids is vital. It helps us understand and fight this tough disease. By knowing more about DIPG, we can improve care for kids with it.
Genetic Factors in DIPG Development
Recent studies have uncovered the genetic factors behind DIPG. Knowing these factors is key to creating better treatments.
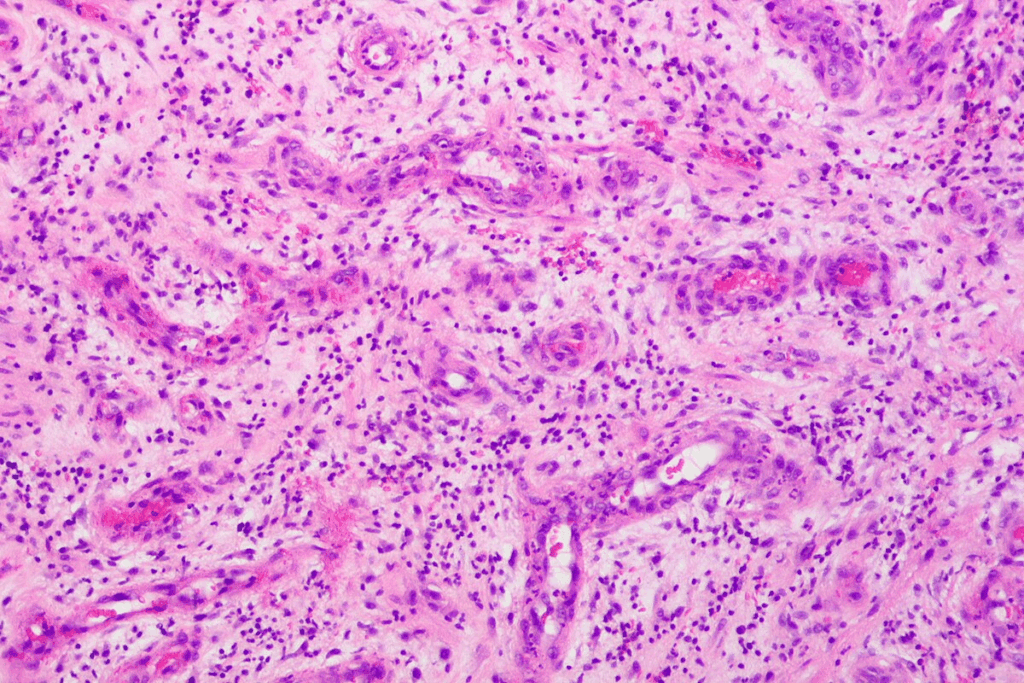
H3K27M Mutation: A Hallmark of DIPG
The H3K27M mutation is a key genetic change in DIPG tumors. It alters the histone H3 protein, changing how genes are expressed. This drives tumor growth. About 80% of DIPG cases have this mutation, making it a key sign of the disease.
This mutation is important for diagnosing and treating DIPG. It helps classify the disease and offers a target for treatment.
Other Genetic Alterations Associated with DIPG
Other genetic changes are also found in DIPG tumors. These include mutations in genes that control cell growth and repair DNA. For example, changes in TP53 and PDGFRA genes help tumors grow and spread.
It’s vital to understand all genetic changes in DIPG to develop effective treatments. Researchers are working to uncover how these changes contribute to the disease.
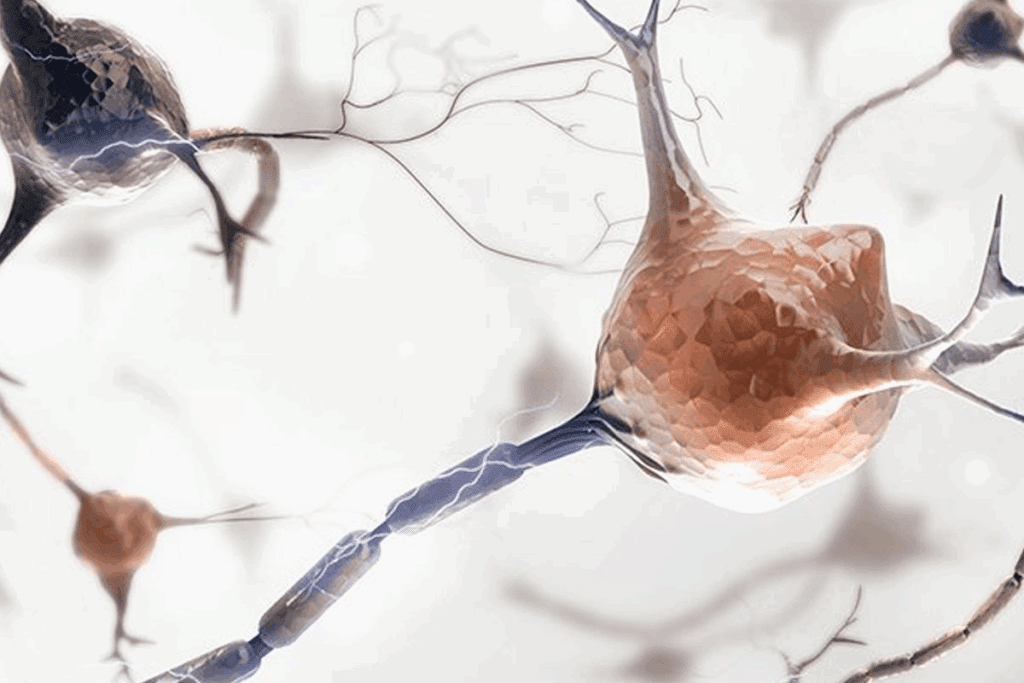
The Cellular Origins of DIPG
DIPG starts from mutations in neural progenitor cells. These cells are key for brain growth. They can turn into different brain cells, but mutations can cause tumors.
The making of DIPG is complex, with many genetic changes. Neural progenitor cells are more likely to get these mutations. This is because they grow fast and are genetically unstable.
Neural Progenitor Cells and DIPG Formation
Neural progenitor cells are vital in DIPG development. Research shows these cells can mutate and cause tumors.
- The H3K27M mutation is a key sign of DIPG, often found in these cells.
- Other genetic changes, like TP53 mutations, also help DIPG grow.
- The change of these cells into tumor cells involves many genetic and epigenetic changes.
How Normal Cells Transform into DIPG Tumor Cells
The change of normal cells into DIPG tumor cells is complex. It involves many genetic and epigenetic changes.
- First, mutations happen in these cells, affecting important genes.
- These mutations cause cells to grow out of control and form tumors.
- More genetic changes can make the tumor more aggressive.
Knowing where DIPG comes from is key to finding treatments. By focusing on the specific mutations and pathways, researchers aim to create better therapies. They hope these will help patients more.
Environmental Factors and DIPG Risk
The exact causes of DIPG are not yet known. Researchers are looking into environmental factors that might play a role. They aim to understand how these factors contribute to DIPG.
Potential Environmental Triggers Under Investigation
Several environmental factors are being studied for their link to DIPG. These include:
- Exposure to ionizing radiation: Some studies suggest that early childhood exposure to ionizing radiation may raise the risk of brain tumors, including DIPG.
- Pesticide exposure: Research is looking into the possible connection between pesticide exposure and cancer, including DIPG.
- Electromagnetic fields: Scientists are studying if electromagnetic fields play a role in cancer development, including DIPG.
It’s important to remember that while these factors are being studied, no direct link to DIPG has been proven yet.
Research on External Risk Factors
Research is ongoing to understand the link between external risk factors and DIPG. This includes:
- Examining the effects of prenatal and perinatal exposures to environmental agents.
- Looking into how parental occupational exposures might affect DIPG risk in children.
As we continue to study environmental factors linked to DIPG, a detailed research approach is key. This will help us find ways to prevent the disease and better understand it.
Why Children Are Susceptible to DIPG
It’s important to know why kids get DIPG to find better treatments. DIPG is a brain cancer that starts in the brainstem. This area controls many body functions.
Children’s brains grow fast, making them more likely to get DIPG. Looking into why this happens helps us understand more about it.
Developmental Factors in Pediatric Brain Cancer
Children’s brains grow quickly, making them more at risk for cancer like DIPG. The growth of brain cells is complex. Problems in this process can cause tumors.
Research points to neural cells as the source of DIPG. These cells are common in kids’ brains. This might explain why DIPG mostly affects children.
The Role of Age in DIPG Vulnerability
Age is a big factor in who gets DIPG. Most cases happen in kids aged 5 to 9. This shows that the brain’s stage of development at this time might make kids more likely to get DIPG.
Studies also found that certain genetic changes in DIPG happen more in young brains. This shows a strong link between age, brain development, and DIPG risk.
By studying how age and brain development affect DIPG, we can find new ways to treat it.
Recognizing DIPG: Early Signs and Symptoms
Spotting the first signs of DIPG is key to catching it early. DIPG, or Diffuse Intrinsic Pontine Glioma, is a brain tumor that mainly hits kids. Its symptoms can be tricky to spot at first. We’ll cover the common signs parents and caregivers should watch for, and how these signs might get worse over time.
Common Initial Symptoms Parents Should Know
The first signs of DIPG can differ, but often include trouble with balance, swallowing, and speaking. This is because the tumor is in the pons. The pons is a vital part of the brainstem that controls many important functions.
- Difficulty with walking or balance
- Swallowing problems (dysphagia)
- Slurred speech or changes in speech
- Weakness or paralysis of facial muscles
- Double vision or other visual disturbances
Progression of Symptoms Over Time
As DIPG gets worse, symptoms can get more severe and new ones can show up. It’s vital for parents to keep a close eye on their child’s health. They should tell their doctor about any changes right away.
| Symptom | Early Stage | Advanced Stage |
| Difficulty Swallowing | Mild, occasional choking | Severe, frequent choking, trouble eating solids or liquids |
| Speech Problems | Slurred speech, mild trouble speaking clearly | Severe speech issues, hard to understand |
| Balance and Coordination | Mild clumsiness, occasional falls | Frequent falls, big trouble walking |
Spotting DIPG symptoms early is critical for getting medical help fast. If your child shows any of these signs, see a doctor right away.
The Diagnostic Journey for DIPG
Diagnosing DIPG needs a detailed approach. It uses advanced imaging and molecular tests. These steps help find the tumor and understand its nature.
Imaging Studies and Their Characteristic Findings
Imaging is key in spotting DIPG. Magnetic Resonance Imaging (MRI) is the main tool. It shows the brainstem and nearby areas clearly.
MRI shows a big, spread-out tumor in the pons. It might push or wrap around important parts nearby.
MRI is vital for DIPG diagnosis. It helps tell it apart from other brain tumors. Special MRI scans give more details about the tumor.
Biopsy Considerations and Molecular Testing
Molecular testing is now key in confirming DIPG. The H3K27M mutation is a key sign of DIPG. Tests can find this mutation and other genetic changes.
Getting a biopsy for DIPG is tricky. The tumor is in the brainstem, a vital area. Biopsy risks are high. So, diagnosis often relies on MRI and clinical signs, with molecular tests when possible.
Current Treatment Approaches for DIPG
It’s important for patients and their families to know about DIPG treatments. DIPG is a tough disease because of its aggressive nature and hard-to-reach location. It requires a mix of therapies to manage it.
Radiation Therapy as Standard of Care
Radiation therapy is the main treatment for DIPG. It helps by making the tumor smaller and easing symptoms. Conventional radiation therapy is given daily for weeks. It doesn’t cure the disease but improves life quality for many.
Chemotherapy Options and Limitations
Chemotherapy is also used to treat DIPG. But, it’s not very effective because of the blood-brain barrier and drug resistance. Conventional chemotherapy doesn’t greatly improve survival rates. So, researchers are looking into more targeted treatments.
Emerging Experimental Treatments
New treatments for DIPG are being explored. These include targeted therapies and immunotherapies. They aim at specific genetic mutations and use the immune system to fight cancer. These options are mostly available in clinical trials.
We’re making progress in treating DIPG. These new treatments give us hope for better outcomes in the future.
Cutting-Edge Research in Understanding DIPG
Recent breakthroughs in DIPG research have opened new avenues for understanding this complex disease. We are witnessing significant advancements in the field. Ongoing studies and clinical trials are providing new insights into the biology of DIPG.
Promising Clinical Trials
Several clinical trials are currently underway, investigating new therapeutic approaches for DIPG. These trials are key in identifying effective treatments and improving patient outcomes. Some of the promising areas of research include:
- Targeted Therapies: Researchers are exploring targeted therapies that can attack DIPG tumor cells. This reduces harm to healthy brain tissue.
- Immunotherapy: Immunotherapy is another area of research. It focuses on harnessing the body’s immune system to fight DIPG.
- Combination Therapies: Combination therapies, which involve using multiple treatments together, are also being investigated. They aim to improve treatment efficacy.
Advances in Understanding DIPG Biology
Advances in genetic and molecular research have significantly enhanced our understanding of DIPG biology. We now know that DIPG is characterized by specific genetic mutations, such as the H3K27M mutation. Further research into the biology of DIPG is critical for developing effective treatments.
Some key areas of research include:
- Genetic Profiling: Detailed genetic profiling of DIPG tumors to identify therapeutic targets.
- Molecular Mechanisms: Investigating the molecular mechanisms underlying DIPG development and progression.
- Stem Cell Research: Studying the role of stem cells in DIPG initiation and growth.
These advances in DIPG research are paving the way for improved diagnosis, treatment, and patient care. As we continue to uncover the complexities of DIPG, we remain hopeful that these efforts will lead to better outcomes for patients.
Prognosis and Long-Term Outlook
The outlook for DIPG is a big worry for those affected. Knowing how the disease progresses and survival chances helps in making care choices.
Disease Course and Survival Rates
DIPG has a poor prognosis, with most patients living less than a year after diagnosis. Its aggressive nature and location in the brainstem limit treatment options. This makes the long-term outlook quite bleak.
Even so, some patients may respond better to treatment. This could lead to a slightly better short-term outlook for them.
| Survival Period | Percentage of Patients |
| Less than 6 months | 30% |
| 6 months to 1 year | 40% |
| 1 to 2 years | 20% |
| More than 2 years | 10% |
Long-Term Survivors: Insights and Hope
Though DIPG survival rates are low, some patients live longer. These cases offer clues on what might lead to a better prognosis.
Studies on long-term survivors are ongoing. They look into genetic, environmental, and treatment factors that might help. This research aims to improve treatment for future patients.
As research into DIPG deepens, there’s hope for better treatments and survival rates in the future.
Conclusion
Understanding DIPG is key to helping kids with brain cancer and supporting their families. We’ve looked into DIPG’s details, from what it is and its genetic links to how it’s treated today. We also talked about why more research is needed.
DIPG is a tough brain cancer that needs special care. By spreading the word about DIPG, we can help improve how it’s diagnosed and treated. This way, we can support families more effectively.
Our conversation about DIPG shows we must keep researching its causes and treatments. Raising awareness about pediatric brain cancer is vital. It helps families get the help they need.
FAQ
What is DIPG cancer?
DIPG, or Diffuse Intrinsic Pontine Glioma, is a brain cancer. It happens in the pons, a part of the brainstem. It’s very aggressive and mostly affects kids.
What are the symptoms of DIPG?
Early signs of DIPG include trouble walking and balancing. You might also see facial weakness, double vision, and swallowing issues. These symptoms can get worse over time.
How is DIPG diagnosed?
Doctors use MRI scans to spot DIPG. They also do molecular tests to check for genetic changes, like the H3K27M mutation.
What is the current treatment for DIPG?
Right now, the main treatment is radiation therapy. It helps manage symptoms and slow the tumor’s growth. Chemotherapy is also tried, but it’s not as effective. New treatments, like clinical trials, are being explored.
What is the prognosis for DIPG?
DIPG has a poor outlook, with quick progression. But, some kids have lived longer. Research is ongoing to find better treatments.
What causes DIPG?
We don’t know the exact cause of DIPG. But, genetic changes, like the H3K27M mutation, are key. Other factors are also being studied.
Why are children more susceptible to DIPG?
Kids are more at risk for DIPG because of their brain development. Their brains are in a different stage, making them more vulnerable.
What is the role of genetic factors in DIPG development?
Genetic changes, like the H3K27M mutation, are vital in DIPG. Other genetic changes also help the tumor grow and spread.
Are there any ongoing clinical trials for DIPG?
Yes, there are trials for new DIPG treatments. They aim to understand DIPG better and find better ways to treat it.
How can families affected by DIPG get support?
Families with DIPG can get help. They can find emotional support, medical advice, and resources to deal with the diagnosis.
References
- Djouder, N., & Rigual, M. del Mar. (2025). CNIO researchers discover a new mechanism for rapid liver regeneration triggered by glutamate. Nature. https://www.cnio.es/en/news/cnio-researchers-discover-a-new-mechanism-for-rapid-liver-regeneration-triggered-by-glutamate/