After a PET scan, many wonder why they must stay away from others. A PET scan uses a radioactive tracer, like FDG, to check for health issues, like cancer.
Those with low FDG tumors worry about the tracer not being absorbed well. This could make the scan less accurate. The tracer’s radioactive nature also raises radiation safety concerns. So, patients are told to avoid being around pregnant women and kids to reduce radiation exposure.
Key Takeaways
- PET scans involve radioactive tracers that require safety precautions.
- Patients with low FDG tumors may have specific concerns related to tracer absorption.
- Radiation safety guidelines are in place to protect others from exposure.
- Isolation after a PET scan is key to reducing radiation exposure.
- Following post-PET scan instructions is vital for patient and public safety.
The Science Behind PET Scans
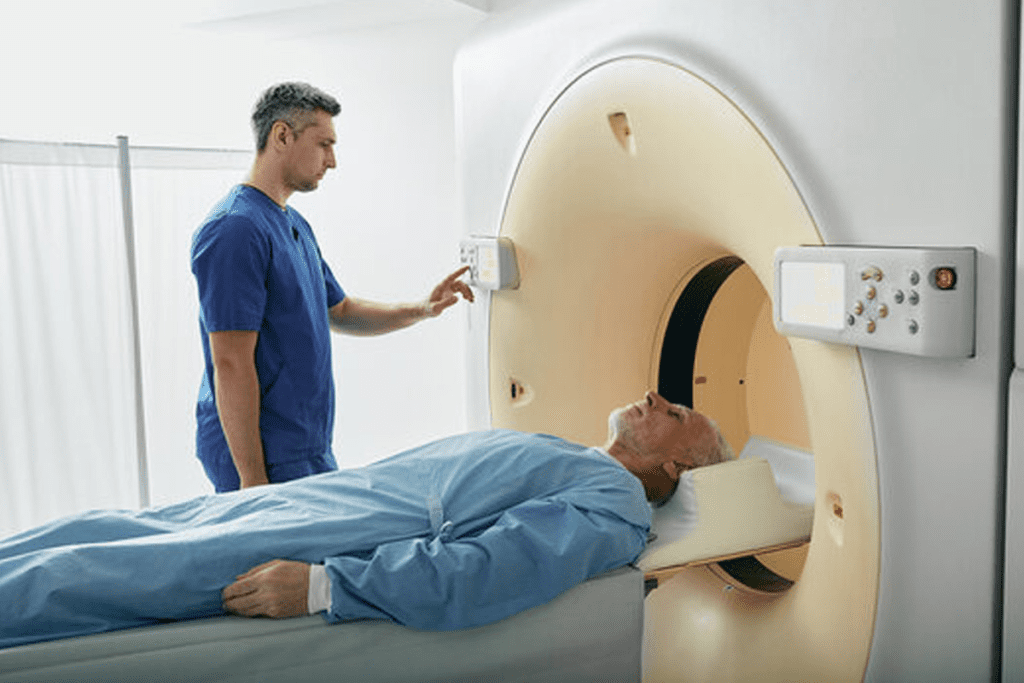
PET scans have changed nuclear medicine a lot. They give deep insights into how our bodies work. This method uses energy from a radioactive tracer to see inside us.
What is a PET scan?
A PET scan is a special imaging tool. It helps find and treat diseases, like cancer. It uses a tiny bit of radioactive material, called a radiotracer, injected into the body.
How radioactive tracers work in the body
Radioactive tracers send out positrons. These positrons meet electrons in our bodies, making gamma rays. The PET scanner catches these rays, showing us what’s inside.
Common applications in disease diagnosis
PET scans are key in fighting cancer. They help doctors see how the disease is growing. They also check the heart and brain for problems.
| Application | Description |
| Oncology | Cancer diagnosis, staging, and treatment monitoring |
| Cardiology | Assessing heart function and viability |
| Neurology | Studying brain disorders and neurodegenerative diseases |
PET scans are very useful in medicine. They help doctors find and treat diseases better. Knowing how they work helps doctors give better care.
Radioactive Tracers: FDG and Beyond
Radioactive tracers have changed how we do PET scans. These tracers give off radiation that the PET scanner picks up. This helps make detailed pictures of what’s inside our bodies.
Understanding FDG (fluorodeoxyglucose)
FDG is the top choice for PET scans. It’s a special glucose molecule with a radioactive fluorine-18 atom. Cancer cells, which use a lot of glucose, take up more FDG. This lets doctors see tumors and other high-glucose areas.
How tracers emit radiation
Tracers like FDG give off radiation as they decay. FDG’s fluorine-18 atom sends out positrons. These positrons meet electrons and turn into gamma rays. The PET scanner catches these rays.
Decay patterns and half-life considerations
The half-life of a tracer is how long it takes for half to decay. Fluorine-18’s half-life is about 110 minutes. Knowing this helps plan PET scans and understand the images better.
| Tracer | Half-life | Primary Use |
| FDG (Fluorine-18) | 110 minutes | Cancer diagnosis, metabolic studies |
| Rubidium-82 | 1.27 minutes | Myocardial perfusion imaging |
| Oxygen-15 | 2.04 minutes | Brain and tumor studies |
Each tracer has its own half-life and use.Each tracer has a specific half-life and application; the choice depends on diagnostic goals and tracer characteristics.
Post-Scan Radiation Emission
Knowing how long radiation stays after a PET scan is key for safety. After a PET scan, the body gives off radiation because of the tracer used. This is important for patient safety and peace of mind.
Duration of Radioactivity
The time a patient stays radioactive depends on the tracer type and amount. The tracer fluorodeoxyglucose (FDG) has a short half-life. This means it breaks down quickly.
Most patients see their radiation levels drop a lot within a few hours after the scan. It’s important to follow the advice of healthcare professionals to avoid exposing others to radiation.
Measuring Radiation Levels
There are ways to check radiation levels after a PET scan. Tools like Geiger counters can measure this. These tools help figure out when it’s safe for a patient to be around others.
Influencing Factors
Several things can change how fast radiation leaves the body. These include:
- Hydration levels: Drinking lots of water helps get rid of the tracer.
- Metabolic rate: People with a faster metabolism might clear the tracer faster.
- Overall health: Some health conditions can affect how the body handles the tracer.
By knowing these factors and following post-scan advice, patients can reduce their radiation exposure. This ensures a safe recovery for everyone.
Radiation Safety Protocols After PET Scans
Keeping everyone safe is key after a PET scan. There are rules to protect patients and those around them. These rules help keep radiation levels low and make sure everyone is safe.
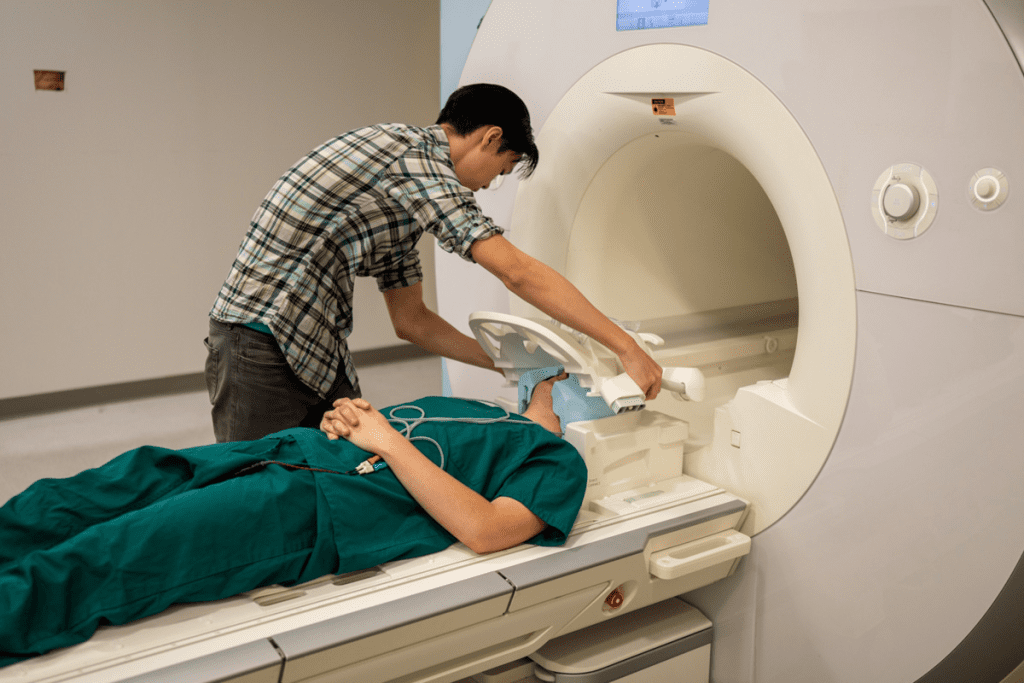
Standard Isolation Requirements
After a PET scan, patients must follow certain rules. They should stay away from pregnant women and kids. This is to keep them safe from radiation.
“The American College of Radiology states that patients should maintain a safe distance from others for a certain period after the scan”. This shows how important it is to stay isolated.
Duration of Precautionary Measures
How long patients need to follow these rules changes. It depends on the type and amount of radioactive tracer used. Usually, the tracer goes away fast, and patients get clear instructions right after the scan.
Hospital vs. Outpatient Guidelines
Hospitals and clinics have their own rules for safety. Inpatients stay in special rooms to keep radiation away. Outpatients get specific advice for home, like drinking lots of water and staying away from others for a bit.
By following these rules, patients help keep others safe. Medical teams stress that
“Radiation safety is everyone’s responsibility, and following these protocols is key for everyone’s health.”
Protecting Others from Radiation Exposure
It’s important for patients who have had a PET scan to know about secondary radiation exposure. This is when others might get exposed to radiation near someone who has had a PET scan.
The Concept of Secondary Radiation Exposure
During a PET scan, a patient gets a radioactive tracer, oftenFDG (fluorodeoxyglucose). This tracer goes to active areas in the body, like tumors, and sends out positrons. These positrons meet electrons, creating gamma rays that the PET scanner uses to make images. But, these gamma rays can also go outside the body, possibly exposing others to radiation.
To lower the risk of secondary radiation, distance and time are key. The radiation weakens with distance, thanks to the inverse square law. This means the closer you are to the patient, the more radiation you might get.
Distance and Time Considerations
The time a patient is radioactive is also important. The radioactive tracer loses strength over time, making exposure risk lower. For example, Fluorine-18, used in FDG, has a half-life of about 110 minutes. This means its radiation halves every 110 minutes. So, the risk of radiation exposure to others drops quickly over a few hours.
Regulatory Requirements for Patient Release
Groups like theNuclear Regulatory Commission (NRC) in the U.S. set rules to keep patients safe after nuclear medicine tests, like PET scans. These rules often tell patients how far to stay from others, like pregnant women and kids, for a certain time.
| Guideline | Description | Recommendation |
| Distance | Maintain a safe distance from others | Stay at least 3 feet away from others, specially children and pregnant women |
| Time | Limit close contact | Avoid close contact for at least 4-6 hours post-scan |
| Hygiene | Practice good hygiene | Flush toilet twice after use and wash hands thoroughly |
By following these guidelines, patients can help keep those around them safe from radiation. This makes sure everyone stays safe and healthy.
Low FDG Tumors: Detection Challenges
Low FDG tumors are hard to find because they don’t take up much glucose. This makes them tricky to spot with PET scans.
Definition and Characteristics
These tumors don’t take up much fluorodeoxyglucose (FDG), a sugar used in PET scans. This makes them hard to see, making diagnosis tough.
These tumors can be different, but they often have low metabolic rates. This is because they are low-grade malignancies or have specific types.
Why Some Cancers Show Minimal Glucose Uptake
Some cancers don’t take up much glucose because of their biology. For example, some tumors have slower glucose metabolism. This makes them hard to find with FDG-PET.
“The variability in FDG uptake among different tumor types poses a significant challenge for PET imaging, as it can lead to false negatives in cancers with low metabolic activity.”
Journal of Nuclear Medicine
Impact on Diagnostic Accuracy
PET scans are less accurate when dealing with low FDG tumors. These tumors don’t take up FDG well, so they can be missed. This can lead to delayed diagnosis and affect treatment plans.
| Tumor Type | FDG Uptake | Detection Difficulty |
| Low-grade Malignancies | Low | High |
| High-grade Malignancies | High | Low |
| Specific Histological Subtypes | Variable | Moderate |
Types of Cancer with Low FDG Uptake
Certain cancers are hard to spot with FDG PET scans because they don’t use much energy. This makes it tough to find the cancer. PET scans work by looking at how active cells are.
Common Low-Metabolic Activity Malignancies
Some cancers, like prostate cancer, don’t show up well on FDG PET scans. This is because they don’t use much energy. Other cancers, like neuroendocrine tumors, might be better seen with different scans.
Neuroendocrine tumors can be tricky to spot because they don’t always show up on FDG scans. 68Ga-DOTATATE scans might work better for them. Mucinous adenocarcinomas also don’t show up well because they’re full of mucin.
Histological Features Affecting FDG Avidity
The look of a tumor affects how it shows up on PET scans. Tumors with few cells and lots of mucin don’t use much glucose. This makes them harder to see.
How well a tumor is formed also matters. Well-formed tumors use less energy than those that aren’t as formed. Knowing this helps doctors understand PET scan results better.
Prognostic Implications of Low Uptake
Tumors that don’t use much energy might have a better outlook. This is because they might not grow as fast. But finding these tumors is tricky.
Doctors need to use many ways to find these tumors. They also need to think carefully about what the scans mean. A study said, “The different ways tumors show up on scans means we need to find the best way to look at each one.”
“The different ways tumors show up on scans means we need to find the best way to look at each one.”
Radiation Risk vs. Diagnostic Benefit
PET scans are very useful for diagnosis but they also expose you to radiation. This means we need to think carefully about the benefits and risks. The radiation from PET scans might raise your cancer risk. So, it’s important to know how much radiation you get and compare it to the natural background radiation.
Quantifying Radiation Exposure from PET
The amount of radiation from a PET scan depends on the tracer and the scan type. For example, a F-FDG PET scan usually gives about 7-10 mSv of effective dose.
Comparison to Natural Background Radiation
The average yearly background radiation in the U.S. is 3.1 mSv. So, a PET scan is like getting 2-3 years of background radiation in one go.
| Radiation Source | Effective Dose (mSv) |
| Annual Background Radiation | 3.1 |
| Typical F-FDG PET Scan | 7-10 |
Long-term Risk Assessment
Looking at long-term risks means considering your age, how much radiation you get, and how you might react to it. Even though the risk is low, doctors must think about these risks and benefits when they suggest PET scans.
Contraindications for PET Imaging
Some medical conditions and factors can make PET imaging not suitable or need special care. It’s key to know these contraindications for patient safety and scan success.
Medical Conditions that Preclude Scanning
Some health issues can stop a patient from getting a PET scan. For example, severe claustrophobia can make staying in the scanner hard. Also, patients with certain metal implants or pacemakers might need special steps or other imaging methods.
| Condition | Consideration |
| Severe Claustrophobia | May require sedation or alternative imaging |
| Metal Implants | May need to be checked for compatibility with PET scan |
| Pacemakers | Requires checking the device’s compatibility and potentially adjusting its settings |
Medication Interactions and Concerns
Some medicines can mess with PET scan results. For instance, diabetes medications that change blood sugar levels can affect the scan’s accuracy. It’s vital for patients to tell their healthcare provider about any medicines they’re taking.
When to Reschedule Your Appointment
If a patient has certain conditions or is taking medicines that could mess with the PET scan, they might need to reschedule. Guidelines usually say to reschedule if a patient has:
- Consumed caffeine or nicotine recently before the scan
- Taken certain medications that could change the scan results
- Had a recent infection or inflammation that could affect the scan’s meaning
By knowing these contraindications and taking the right steps, patients can safely get PET imaging and get accurate results.
The Impact of Blood Glucose on PET Results
Blood glucose levels can greatly affect the accuracy of PET scan results. High levels, or hyperglycemia, can make PET scans less clear, mainly when using FDG (fluorodeoxyglucose). This is because FDG and glucose compete for cell uptake.
Hyperglycemia and Scan Quality
High blood sugar can lower FDG uptake in tumors. This might lead to scans that are not clear or accurate. It’s a big issue for people with diabetes, whose blood sugar can change a lot. Keeping blood sugar in check is key for a good scan.
Diabetes Management Before Imaging
For those with diabetes, managing their condition is vital before a PET scan. They might need to adjust their meds, watch their blood sugar, and eat certain foods. Keeping blood sugar right is important for a good scan.
Fasting Requirements and Preparation
Fasting is often needed before a PET scan to keep blood sugar low. How long you fast can vary, but it’s usually a few hours. Here’s what you need to know:
| Preparation Step | Guideline |
| Fasting Duration | 4-6 hours |
| Blood Glucose Monitoring | Check levels before scan |
| Medication Adjustment | As advised by doctor |
By following these steps, patients can help make sure their PET scan is as accurate as it can be.
Recent Surgery and Inflammatory Responses
Recent surgery can change how PET scans are read because of the body’s inflammatory response. After surgery, the body starts to heal, which includes inflammation. This inflammation can make PET scans show up differently, as it can look like both healing tissues and cancer.
Impact of Healing Tissue on PET Scan Interpretation
The inflammation from surgery can make the PET scan show more activity. This can make it hard for doctors to tell if it’s cancer or not. It’s important to know when the PET scan is done after surgery to get the right results.
Recommended Waiting Periods After Surgical Procedures
To avoid mistakes in PET scan results, waiting a bit after surgery is often advised. The wait time depends on the surgery type and how fast the body heals. Usually, doctors suggest waiting 4 to 6 weeks, but it varies.
Distinguishing Inflammation from Malignancy
Telling the difference between surgery inflammation and real cancer is a big challenge. Doctors use advanced imaging and look at the patient’s history to figure it out. The table below shows some key differences.
| Characteristics | Inflammation | Malignancy |
| PET Scan Uptake Pattern | Diffuse uptake around the surgical site | Focal uptake in tumor areas |
| Clinical Context | Recent surgery, wound healing | Known cancer, metastasis |
| Temporal Changes | Decreases over time as healing progresses | Persists or increases over time |
Knowing these differences helps doctors make better diagnoses and treatment plans.
Small Lesion Detection Limitations
Small lesion detection is key in PET imaging, but it faces resolution constraints. Being able to spot small lesions is vital for accurate diagnosis and treatment plans.
Technological Constraints
Today’s PET scan tech has limits in resolution, impacting its ability to find small lesions. The scanner’s hardware and software set its resolution.
Resolution constraints in PET scans cause partial volume effects. This spreads out the signal from small lesions, making them harder to spot. This is a big problem in oncology, where finding small tumors early is critical.
Size Thresholds for Reliable Detection
There’s a size limit below which PET scans struggle to detect lesions reliably. This limit changes based on the scanner and its use.
Research shows that lesions under 5-7 mm are often missed due to resolution and sensitivity limits. But, new scanner tech is pushing these limits higher.
| Lesion Size (mm) | Detection Reliability (%) |
| 5-7 | 60 |
| 8-10 | 80 |
| >10 | 95 |
Combining Imaging Modalities
To beat PET scan limits in finding small lesions, mixing imaging types works well. MRI and CT scans add valuable info that boosts accuracy.
Using info from various imaging methods helps doctors better find and understand small lesions. This leads to better care for patients.
Managing Radiation Exposure in Healthcare Settings
Healthcare facilities must take strong steps to manage radiation exposure. This protects staff, patients, and the environment. It’s key to have good radiation safety plans to lower risks from medical tests and treatments.
Protocols for Medical Staff
Medical staff are key in keeping everyone safe from radiation. They follow these steps:
- They get regular training on how to handle radiation safely.
- They wear personal protective equipment (PPE) during procedures.
- They check their radiation exposure with dosimeters.
The National Council on Radiation Protection and Measurements (NCRP) says, “Radiation safety training is vital for all who work with radiation in medicine.”
Facility Design Considerations
The design of healthcare buildings is very important for safety. Here are some key points:
| Design Element | Purpose |
| Shielding in walls and doors | To cut down radiation exposure in other areas |
| Controlled access zones | To keep exposure to those who should be there |
| Radiation therapy rooms | They have special safety features to reduce exposure during treatment |
Monitoring and Documentation Requirements
Keeping track of radiation and documenting it is very important. This means:
- Checking radiation levels in the environment often
- Keeping records of how much radiation patients get
- Tracking how much radiation staff get
By following these steps, healthcare places can keep everyone safe. The American College of Radiology says, “A detailed radiation safety plan is key to reducing exposure and ensuring top-notch care for patients.”
Conclusion: Balancing Safety and Diagnostic Needs
PET scans are key in finding and managing diseases, but they do involve radiation. It’s important to find a balance between keeping patients safe and getting the needed information.
Keeping radiation exposure low is a top priority. This includes protecting patients, doctors, and others. Knowing how PET scans work helps doctors take the right steps to keep everyone safe.
Doctors must think about the risks of radiation when deciding to use PET scans. By using the right protocols and following safety rules, they can get the most information while keeping risks low.
It’s all about finding the right balance for each patient. By focusing on safety and getting accurate results, doctors can give the best care possible.
FAQ
What is a PET scan and how does it work?
A PET scan is a test that uses a radioactive tracer to see how the body works. It injects a small amount of radioactive material into the body. This material is then absorbed by cells.
Why is isolation necessary after a PET scan?
Isolation is needed after a PET scan because the tracer stays in the body and emits radiation. This radiation can be detected by others. To protect others, patients must follow safety protocols, including staying isolated for a while.
How long do patients remain radioactive after a PET scan?
The time a patient stays radioactive after a PET scan varies. It depends on the tracer used and how fast the body breaks it down. Usually, patients stop emitting significant radiation a few hours to a day after the scan.
What are low FDG tumors, and why are they challenging to detect?
Low FDG tumors are cancers that don’t take up much glucose. This makes them hard to spot with FDG-PET scans. They might have low activity or other traits that reduce their glucose uptake. This requires other imaging methods or special diagnostic steps.
Can PET scans be used for all types of cancer?
PET scans are useful for many cancers but not all. They work best for cancers that take up a lot of glucose. For cancers with low glucose uptake, other imaging methods might be needed.
How does hyperglycemia affect PET scan results?
High blood sugar can lower the accuracy of PET scans. This is because it reduces the glucose uptake in tumors. People with diabetes or high blood sugar should manage their levels before a PET scan for the best results.
What are the contraindications for PET imaging?
Some conditions make PET imaging unsafe, like pregnancy or breastfeeding. Certain medications can also affect the scan’s safety or accuracy. It’s important to talk to your doctor about your medical history and any concerns before a PET scan.
How can radiation exposure from PET scans be minimized?
To reduce radiation exposure from PET scans, follow safety protocols like staying isolated for a while. Healthcare providers also use safe dosing and scanning techniques to protect staff and others.
Are there alternative imaging modalities for detecting low FDG tumors?
Yes, other imaging methods like MRI or CT scans can help find low FDG tumors. The right choice depends on the cancer type and the patient’s situation. This shows the importance of a personalized approach to diagnosis.
What are the benefits and limitations of PET scans in cancer diagnosis?
PET scans are very sensitive and specific for cancer diagnosis. They show metabolic activity. But, they might not work for all tumors, like those with low glucose uptake. This means other imaging methods might be needed for a complete picture.
References
- Flavell, R. R., Naeger, D. M., Aparici, C. M., Hawkins, R. A., Pampaloni, M. H., & Behr, S. C. (2016). Malignancies with low fluorodeoxyglucose uptake at PET/CT: Pitfalls and prognostic importance. Radiographics / PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4801421/
- Aldousari, H., Abuhadi, N., Izz, M., Alshammari, T., Ali, Z., Aldaas, R., Bakry, A. E. H., & Abukonna, A. (2023). Assessment of external radiation dose rate after 18F-FDG PET/CT examination. Egyptian Journal of Radiology and Nuclear Medicine, 54, Article 80. Retrieved from https://ejrnm.springeropen.com/articles/10.1186/s43055-023-01031-y
- Berberoglu, K., Ozudogru, E., Fikri, B., & Oral, A. (2019). External radiation exposure rate after 18F-FDG PET/CT: Radioprotection study. Radioprotection / External radiation exposure rate after 18F-FDG PET/CT. Retrieved from https://www.radioprotection.org/articles/radiopro/full_html/2019/02/radiopro190004/radiopro190004.html