Last Updated on December 1, 2025 by Bilal Hasdemir
Retinoblastoma is a rare eye cancer that mainly affects kids. It can be challenging to identify because its symptoms may resemble those of other harmless conditions. One in every 15,000 to 20,000 children is diagnosed with retinoblastoma. This shows how important it is to tell them apart correctly.
Some harmless conditions can look like retinoblastoma symptoms, like leukocoria, a white glow in the eye. Getting the right diagnosis is key to not mistaking it and to treat it right.
Knowing the difference between retinoblastoma and its look-alikes is key for good care. We’ll look into these differences to help with diagnosis and treatment.
Key Takeaways
- Retinoblastoma is a rare eye cancer in children.
- Benign conditions can mimic retinoblastoma symptoms.
- Accurate diagnosis is key for effective treatment.
- Leukocoria treatment is a big part of managing retinoblastoma-like conditions.
- Understanding retinoblastoma prognosis helps in managing expectations.
Understanding Retinoblastoma and Its Clinical Presentation
Retinoblastoma can be tricky to spot, making it key to know its signs. It’s a serious eye cancer that mainly hits young kids. To diagnose it, you need to understand its definition, how common it is, and its genetic roots.
Definition and Epidemiology of Retinoblastoma
Retinoblastoma is a cancer of the retina, mostly seen in kids under five. It’s the top eye cancer in kids, happening in about 1 in 15,000 to 1 in 20,000 births. It can affect one or both eyes, with both eyes more likely if it runs in the family.
Key epidemiological features of retinoblastoma include:
- Age: Most cases are diagnosed before the age of three.
- Geographic variation: Incidence rates vary globally, with higher rates observed in certain regions.
- Genetic predisposition: Familial cases are associated with mutations in the RB1 gene.
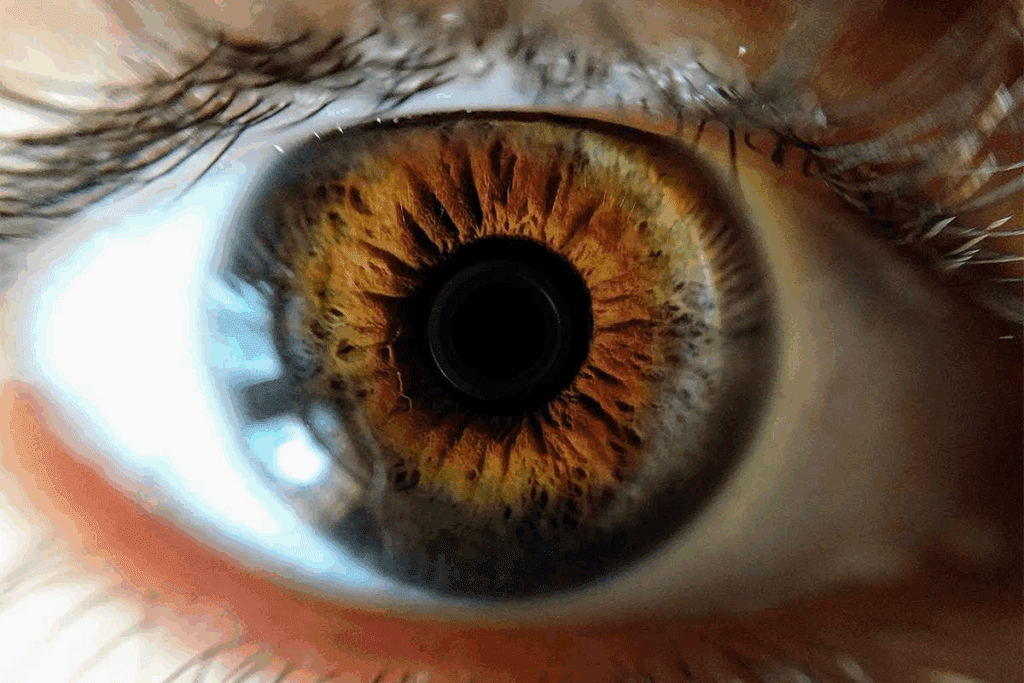
Classic Signs and Symptoms
Retinoblastoma often shows up with leukocoria (a white pupillary reflex) or strabismus (squint). Other signs include:
- Vision loss or poor vision.
- Eye redness or inflammation.
- Heterochromia iridum (different colored irises).
Spotting it early is key, as late detection can cause serious vision loss or spread to other parts of the body.
Genetic Basis of Retinoblastoma
The RB1 gene mutation is key in retinoblastoma. This gene helps control cell growth. When both copies of the RB1 gene are mutated, retinoblastoma can develop. Families with a history of the disease often have a genetic mutation in one copy, with the second mutation happening later.
Genetic counseling is vital for families with retinoblastoma history. It helps find at-risk individuals and aids in early detection and treatment.
The Importance of Accurate Diagnosis in Suspected Retinoblastoma Cases

When retinoblastoma is suspected, getting an accurate diagnosis is key. This eye cancer mainly hits young kids. It’s hard to diagnose because other conditions can look like it.
Consequences of Misdiagnosis
Misdiagnosis can cause the wrong treatment and delay the right one. For example, if a child is thought to have retinoblastoma but really has Coats’ disease, they might get too much chemotherapy. Or, not finding retinoblastoma can mean treatment is too late, leading to worse outcomes.
| Condition | Common Misdiagnosis | Consequences of Misdiagnosis |
| Retinoblastoma | Coats’ disease, Persistent Fetal Vasculature (PFV) | Unnecessary treatment, delayed actual treatment |
| Coats’ disease | Retinoblastoma | Unnecessary enucleation or chemotherapy |
Challenges in Pediatric Ocular Diagnosis
It’s hard to diagnose eye problems in kids because they can’t tell us what’s wrong. We also need special tools to look at their eyes. Plus, kids’ eyes are always changing, making it tough to figure out what’s going on.
The Concept of Pseudoretinoblastoma
Pseudoretinoblastoma is when other conditions look like retinoblastoma. This includes Coats’ disease and persistent fetal vasculature (PFV). Knowing about these is key to making the right diagnosis.
Finding the right diagnosis for retinoblastoma is a team effort. We use eye exams, scans, and sometimes DNA tests. We stress how important it is to get it right to avoid bad outcomes and make sure kids get the right care.
Overview of Benign Mimics of Retinoblastoma
Many benign eye conditions can look like retinoblastoma, making it hard for doctors to diagnose. These conditions, known as pseudoretinoblastoma, can look very similar to retinoblastoma. So, it’s very important to get the diagnosis right.
Definition and Classification of Pseudoretinoblastoma
Pseudoretinoblastoma is a group of benign conditions that look like retinoblastoma. They can be caused by many things, like birth defects, inflammation, blood vessel problems, and tumors.
Knowing how to classify these conditions helps doctors understand and treat them. This is key for making the right diagnosis and treatment plan.
Frequency of Benign Mimics in Clinical Practice
In medical practice, benign mimics of retinoblastoma are quite common. Research shows many kids thought to have retinoblastoma are actually diagnosed with something else.
This highlights the need for careful diagnosis to avoid wrong treatments. It’s important to make sure the diagnosis is correct.
Common Presenting Features of Mimics
Benign mimics of retinoblastoma can show symptoms like white reflex, eye misalignment, and vision loss. For example, Coats’ disease and retinopathy of prematurity can look like retinoblastoma.
Doctors need to know these symptoms to tell the difference between these conditions and retinoblastoma. This ensures the right care is given.
We will keep looking into these conditions. We’ll share more about how to diagnose and manage them.
Persistent Fetal Vasculature (PFV) as a Retinoblastoma Mimic
Understanding PFV is key to diagnosing and treating patients with suspected retinoblastoma. PFV is a birth defect where the fetal blood vessels don’t disappear as they should. This can lead to serious eye problems.
Clinical Features and Pathophysiology of PFV
PFV can cause symptoms like leukocoria, strabismus, and microphthalmia. The main issue is the leftover fetal blood vessels. These can cause retinal detachment and glaucoma. Early diagnosis is critical to avoid these problems and tell PFV apart from retinoblastoma.
Diagnosing PFV can be tricky because its symptoms vary. A detailed eye exam and imaging studies are needed for an accurate diagnosis.
Distinguishing PFV from Retinoblastoma
To tell PFV from retinoblastoma, we need to know the signs and imaging findings of both. PFV is marked by leftover fetal blood vessels and no calcification. Retinoblastoma, on the other hand, has calcification.
- Clinical examination findings
- Imaging characteristics, such as ultrasound and MRI findings
- Presence or absence of calcification
By looking at these details, we can make the right diagnosis and plan the best treatment.
Management Approaches for PFV
Managing PFV aims to prevent complications and save vision. Treatments might include surgery for retinal detachment or other issues. Sometimes, just watching the condition closely is enough.
Conservative management means regular check-ups to catch any problems early. Sometimes, surgery is needed to improve the outcome.
It’s important to have a team approach to PFV care. This includes pediatric ophthalmologists, ocular oncologists, and other specialists.
Coats’ Disease and Its Similarity to Retinoblastoma
Coats’ disease is often mistaken for the serious eye tumor, retinoblastoma. This is because they share some symptoms. It’s important to know the difference to get the right treatment.
Pathophysiology and Etiology
Coats’ disease happens when blood vessels behind the retina grow abnormally. This can cause the retina to detach and lead to vision loss. It usually affects young males and is often seen in one eye.
The exact reason for Coats’ disease is not known. But, it’s thought to be linked to a problem with the blood-retinal barrier. This barrier breakdown lets plasma and lipids leak into the retina. This causes fluid and lipid buildup, leading to detachment and vision problems.
Diagnostic Criteria and Imaging Findings
To diagnose Coats’ disease, doctors use a combination of exams and imaging. Key signs include:
- Retinal telangiectasias
- Exudation and retinal detachment
- No calcification, unlike in retinoblastoma
Ultrasound, fluorescein angiography, and OCT are key tools. They help spot the unique blood vessel issues in Coats’ disease.
Treatment Options and Outcomes
Treatment for Coats’ disease focuses on stopping vision loss. Options include:
- Laser photocoagulation to destroy bad blood vessels
- Cryotherapy to treat detachment and exudation
- Intravitreal anti-VEGF injections to reduce swelling
- Surgery for advanced cases
Early treatment can greatly improve vision outcomes. Regular check-ups are key to tracking the disease and adjusting treatment plans.
Retinopathy of Prematurity Mimicking Retinoblastoma
Retinopathy of prematurity (ROP) is a condition that can look like retinoblastoma in premature babies. It happens when blood vessels in the retina grow abnormally. This can cause scarring and even retinal detachment.
Pathogenesis of Retinopathy of Prematurity
ROP starts when the retina’s blood vessels don’t grow right because of early birth. This leads to areas without blood vessels. These areas can start growing new blood vessels, which can be affected by oxygen therapy, how early the baby was born, and their weight.
Stages of ROP That May Resemble Retinoblastoma
Stages 4 and 5 of ROP can look like retinoblastoma because they cause a white glow in the eye. This is the same white glow seen in retinoblastoma. It’s hard to tell them apart because of the retinal detachment and possible changes like retrolental fibroplasia.
Differential Diagnostic Features
To tell ROP apart from retinoblastoma, doctors look at the baby’s birth history, eye exams, and imaging tests. Knowing the baby was premature, if both eyes are affected, and seeing other signs of ROP helps diagnose it. Ultrasound and MRI can show how bad the detachment is and check for retinoblastoma’s hallmark, intraocular calcification.
Management Strategies for Advanced ROP
Dealing with advanced ROP needs a team of eye doctors and other specialists. They use laser treatment, injections to stop blood vessel growth, and surgery for detachment. Catching it early and acting fast is key to saving vision and improving life for babies with ROP.
Ocular Toxocariasis as a Retinoblastoma Mimic
Ocular toxocariasis is a parasitic infection caused by Toxocara species. It can look like retinoblastoma in children. This happens when young people touch contaminated soil or materials with Toxocara eggs.
Pathogenesis and Epidemiology
The infection starts when Toxocara eggs are eaten. These eggs hatch into larvae that move to the eyes. They cause inflammation and damage, making symptoms similar to retinoblastoma.
It’s more common in kids and young adults. This is true in places with poor hygiene and where pets, like dogs, are common.
Clinical Presentation and Ocular Findings
Ocular toxocariasis shows different symptoms. These include uveitis, vitreous inflammation, and retinal detachment. It can look like retinoblastoma with a white pupillary reflex or strabismus.
Other signs include:
- Peripheral or posterior pole granulomas
- Vitreous membranes or strands
- Retinal traction or detachment
Diagnostic Approaches and Serological Testing
To diagnose ocular toxocariasis, doctors use several methods. They look at clinical signs, imaging, and blood tests. Finding anti-Toxocara antibodies in blood or eye fluids helps confirm the diagnosis.
| Diagnostic Method | Description |
| Serology | Detection of anti-Toxocara antibodies |
| Ocular Ultrasound | Visualization of ocular structures and granulomas |
| Optical Coherence Tomography (OCT) | Detailed imaging of retinal layers and pathology |
Treatment Strategies and Prognosis
Treatment for ocular toxocariasis includes anti-parasitic drugs like albendazole. Anti-inflammatory therapy is also used to manage uveitis. Sometimes, surgery is needed for retinal detachment or other issues.
The outcome depends on how severe the infection is and how well it responds to treatment. Early diagnosis and treatment can help save vision and prevent eye damage.
Retinal Astrocytic Hamartoma and Other Benign Tumors
Retinal astrocytic hamartomas are benign tumors that doctors look at when checking kids for retinoblastoma. These tumors are rare but important because they can look like serious conditions.
Clinical Characteristics of Astrocytic Hamartomas
Astrocytic hamartomas are growths from the retina’s astrocytes. They are often linked to tuberous sclerosis complex (TSC), a genetic disorder that causes tumors in different parts of the body.
These hamartomas are usually small and might have calcium deposits. They look like white or yellow spots in the retina. Optical coherence tomography (OCT) and fundus fluorescein angiography (FFA) help doctors diagnose them.
Association with Tuberous Sclerosis Complex
Tuberous sclerosis complex is linked to retinal astrocytic hamartomas. People with TSC are more likely to have these hamartomas and other symptoms.
Seeing these hamartomas can help doctors diagnose TSC. So, if they find these tumors, they will check for TSC.
Other Benign Retinal Tumors
There are other benign retinal tumors that can look like retinoblastoma. These include:
- Retinal capillary hemangiomas
- Combined hamartoma of the retina and retinal pigment epithelium
- Retinal pigment epithelial hamartomas
Each of these conditions has its own signs that help doctors tell them apart from retinoblastoma and other cancers.
Management Considerations for Benign Tumors
How doctors manage benign retinal tumors depends on their type and symptoms. Often, just watching them is enough. But, regular check-ups are key to see if they change.
In some cases, treatments like laser or cryotherapy might be needed. This is to fix problems like retinal detachment or bleeding in the vitreous.
Inflammatory Conditions That Can Mimic Retinoblastoma
Several inflammatory conditions can look like retinoblastoma, making diagnosis hard. These diseases can have symptoms similar to retinoblastoma. Accurate diagnosis is key.
Endophthalmitis: Presentation and Diagnosis
Endophthalmitis is a severe eye inflammation, often from infection. It can cause pain, redness, and vision loss, like retinoblastoma. Prompt diagnosis is vital to avoid vision loss and other issues.
To diagnose endophthalmitis, doctors use clinical exams, imaging, and sometimes a vitreous tap. We must tell it apart from retinoblastoma by looking at symptoms and test results carefully.
Posterior Uveitis and Retinitis
Posterior uveitis and retinitis affect the eye’s back part. They can cause inflammation, vasculitis, and choroiditis, looking like retinoblastoma on scans.
- Clinical Features: Symptoms include floaters, blurred vision, and eye pain.
- Diagnostic Approaches: Tests like fluorescein angiography, OCT, and ultrasound help diagnose these conditions.
Toxoplasmosis Retinochoroiditis
Toxoplasmosis retinochoroiditis is caused by Toxoplasma gondii. It can cause necrotizing retinitis and choroiditis, looking like retinoblastoma. This is due to inflammation and lesions in the retina.
Diagnosis involves tests for Toxoplasma antibodies, clinical exams, and sometimes vitreous sampling for PCR. Treatment includes antiparasitic drugs and sometimes corticosteroids.
Differentiating Inflammatory Processes from Malignancy
To tell inflammatory conditions from retinoblastoma, we need a detailed approach. This includes a thorough clinical history, imaging, and sometimes diagnostic vitrectomy or fine-needle aspiration biopsy.
We use advanced imaging like MRI and ultrasound to tell them apart. The presence of calcification in a tumor is a key sign of retinoblastoma. Inflammatory conditions show different signs on scans.
In conclusion, accurately diagnosing retinoblastoma and differentiating it from inflammatory conditions is critical. We must be aware of the various presentations to provide the best care for our patients.
Congenital Anomalies Confused with Retinoblastoma
Diagnosing retinoblastoma can be tricky because of congenital anomalies that look like the disease. These anomalies make it hard to tell if it’s really retinoblastoma. A deep understanding is needed to tell them apart.
Myelinated Nerve Fibers
Myelinated nerve fibers are a harmless condition that can look like retinoblastoma. They show up as white or yellowish spots on the retina. Diagnostic imaging, like optical coherence tomography (OCT), can spot this without seeing any cancer.
Congenital Retinal Folds and Falciform Folds
Congenital retinal folds and falciform folds look like retinoblastoma but are not. They happen when the retina doesn’t develop right. Indirect ophthalmoscopy and scans can tell them apart from real retinoblastoma.
Persistent Hyperplastic Primary Vitreous
Persistent hyperplastic primary vitreous (PHPV) is now called persistent fetal vasculature (PFV). It’s a birth defect where the primary vitreous doesn’t go away. It can look like a tumor, but MRI can show it’s not cancer.
Other Developmental Abnormalities
Other issues like retinal dysplasia and colobomas can also be mistaken for retinoblastoma. A detailed eye check and scans are key to correct diagnosis. Knowing what these look like helps doctors treat the right condition.
Advanced Imaging Techniques in Differentiating Retinoblastoma from Mimics
In the field of eye cancer, advanced imaging is key. It helps tell retinoblastoma apart from look-alikes. Accurate diagnosis is vital for good treatment and patient care. We use different imaging tools to get clear views of eye tumors.
Ultrasonography Findings and Characteristics
Ultrasonography is a big help in eye tumor diagnosis, including retinoblastoma. It shows the tumor’s size, shape, and inside details. Key ultrasonographic features of retinoblastoma include:
- Presence of calcification, which is highly suggestive of retinoblastoma
- Tumor size and extent
- Assessment of retinal detachment or vitreous seeding
By looking at these signs, doctors can tell if it’s retinoblastoma or something else.
MRI Features of Retinoblastoma vs. Benign Mimics
Magnetic Resonance Imaging (MRI) is also very important. It shows how big the tumor is and if it’s spread. Key MRI features that help include:
- Presence of calcification within the tumor
- Tumor enhancement patterns after contrast administration
- Assessment of optic nerve involvement
By comparing MRI signs of retinoblastoma with its look-alikes, doctors can make better diagnoses.
Optical Coherence Tomography Applications
Optical Coherence Tomography (OCT) is a non-invasive way to see the retina clearly. In retinoblastoma, OCT is great for:
- Assessing retinal tumor seeding
- Evaluating subretinal fluid or retinal detachment
- Monitoring response to treatment
OCT’s detailed images are very helpful in managing retinoblastoma.
Fluorescein Angiography Patterns
Fluorescein angiography shows the retina’s blood vessels. In retinoblastoma, it reveals specific patterns. These include:
- Rapid filling of the tumor with fluorescein
- Presence of abnormal vascular patterns within the tumor
- Late leakage of fluorescein from the tumor
By studying these patterns, doctors can tell if it’s retinoblastoma or not.
In summary, advanced imaging is essential for diagnosing and treating retinoblastoma. Using ultrasonography, MRI, OCT, and fluorescein angiography, we can accurately spot retinoblastoma. This ensures the right treatment and better patient results.
Retinoblastoma Prognosis Compared to Its Benign Mimics
Retinoblastoma and its benign mimics have different outcomes. Retinoblastoma is a serious cancer, while its mimics are not. This means the prognosis for retinoblastoma is much worse.
Survival Rates and Long-term Outcomes in Retinoblastoma
Treatment for retinoblastoma has gotten better over time. Survival rates have gone up a lot, with over 95% of kids living into adulthood. But, the long-term results depend on when it’s found, the genes involved, and the treatment.
Early treatment is key to better survival chances and fewer long-term problems. New treatments like chemotherapy and laser therapy are helping more kids survive.
Prognosis for Vision and Eye Preservation in Benign Conditions
Benign mimics like PFV, Coats’ disease, and ROP have a much better outlook. They can often be treated early, saving vision and avoiding eye removal.
Early diagnosis is vital for these conditions. It lets doctors start the right treatment quickly, reducing risks. The chance of keeping good vision is usually high, but it depends on the condition’s severity.
Quality of Life Considerations in Different Diagnoses
Quality of life matters a lot in treating retinoblastoma and its mimics. For retinoblastoma, the goal is to beat the cancer and avoid treatment side effects. For benign conditions, it’s about keeping vision and eye looks good.
The emotional impact of a diagnosis is big for families. So, supportive care is a big part of treatment. It helps with the emotional and mental health of patients and their families.
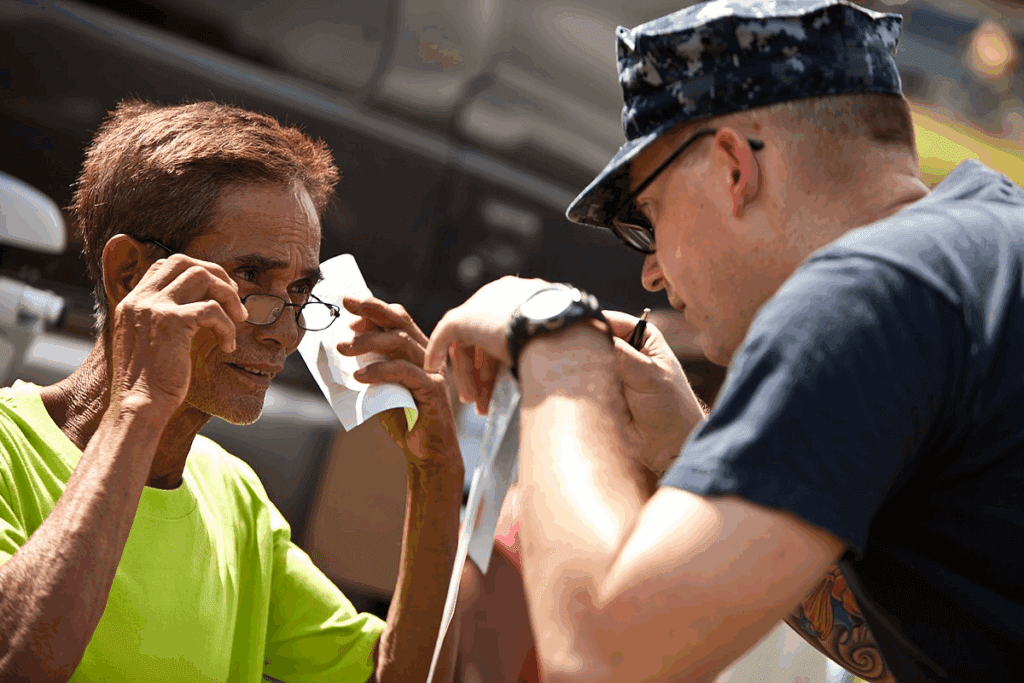
Multidisciplinary Approach to Diagnosis of Suspected Retinoblastoma
A team of experts is key to diagnosing and treating retinoblastoma. This team works together to understand the disease fully. This leads to better diagnoses and treatment plans.
Role of Pediatric Ophthalmologists and Ocular Oncologists
Pediatric ophthalmologists and ocular oncologists start the diagnosis process. They use tools like fundoscopy and imaging to spot the tumor. Their skills are important in telling retinoblastoma apart from other conditions.
Input from Pediatric Oncologists
Pediatric oncologists specialize in childhood cancers. They help figure out how far the disease has spread. They also plan treatments, like chemotherapy, and check how well the patient is doing.
Importance of Pathological Confirmation
Confirming the diagnosis through tissue samples is vital. This step is key for planning treatment and understanding the patient’s future. Methods like fine-needle aspiration biopsy or enucleation help get the needed tissue.
Genetic Counseling Considerations
Genetic counseling is important for families with retinoblastoma. Counselors help find at-risk family members and explain genetic testing. They also offer advice on family planning, which is very helpful.
| Specialist | Role in Diagnosis | Key Contributions |
| Pediatric Ophthalmologists | Initial assessment and diagnosis | Fundoscopy, imaging studies |
| Ocular Oncologists | Tumor characterization and staging | Advanced imaging, tumor biopsy |
| Pediatric Oncologists | Treatment planning and management | Chemotherapy, monitoring response |
| Genetic Counselors | Risk assessment and family guidance | Genetic testing, family planning advice |
Psychological Impact of Suspected Retinoblastoma Diagnosis
When a child might have retinoblastoma, the whole family feels a mix of emotions. The wait from suspicion to diagnosis is hard. It’s filled with worry and fear about what’s to come.
Supporting Families Through the Diagnostic Process
We know how vital it is to support families during this tough time. We offer clear, caring talks and make sure they get the help they need.
Key support strategies include:
- Providing emotional support and counseling
- Facilitating access to information and resources
- Encouraging open communication between families and healthcare providers
Coping with Uncertainty and Anxiety
Dealing with the unknown of a suspected retinoblastoma diagnosis is tough for families. It’s key to recognize these feelings and help manage them.
Effective coping mechanisms may include:
- Seeking support from family and friends
- Engaging in stress-reducing activities
- Staying informed about the diagnosis and treatment options
Resources for Families Facing Eye Disease in Children
Families dealing with the possibility of retinoblastoma or other eye diseases in kids need good resources. This includes educational materials, support groups, and counseling services.
| Resource Type | Description | Benefits |
| Support Groups | Groups for families to share experiences and support one another | Emotional support, community building |
| Educational Materials | Brochures, websites, and guides about retinoblastoma and its treatment | Informed decision-making, understanding of diagnosis and treatment |
| Counseling Services | Professional counseling for families to cope with emotional challenges | Emotional support, coping strategies |
Conclusion: Navigating the Diagnostic Challenges of Retinoblastoma Mimics
Dealing with retinoblastoma and its look-alikes needs a detailed and careful strategy. We’ve talked about several harmless conditions that can look like retinoblastoma. It’s key to get the diagnosis right and manage it well.
Getting retinoblastoma diagnosed correctly is vital to avoid wrong diagnoses and the right treatment. Knowing the challenges and spotting look-alikes can greatly help patients.
By working together and using the latest imaging, we can better tell retinoblastoma apart from harmless conditions. This boosts our accuracy and helps in finding the best ways to manage it.
In the end, we stress the importance of staying informed and educated about retinoblastoma and its look-alikes. This leads to better care and results for patients.
FAQ
What is retinoblastoma?
Retinoblastoma is a rare eye cancer that mostly affects young kids, under five. It starts in the retina, the back of the eye.
What are the symptoms of retinoblastoma?
Symptoms include a white glow in the pupil, crossed eyes, vision issues, and sometimes eye pain or redness.
What is pseudoretinoblastoma?
Pseudoretinoblastoma are conditions that look like retinoblastoma but aren’t cancer. It’s important to tell them apart.
How is retinoblastoma diagnosed?
Doctors use eye exams, imaging like ultrasound or MRI, and genetic tests to find the RB1 gene mutation.
What is the RB1 gene mutation?
The RB1 gene mutation can cause retinoblastoma. It’s a gene that stops tumors, and mutations can lead to cancer.
What are the treatment options for retinoblastoma?
Treatments include chemotherapy, laser therapy, cryotherapy, radiation, or removing the eye in severe cases.
Can retinoblastoma be cured?
Yes, early treatment can cure retinoblastoma. In developed countries, over 95% of cases are cured.
What is the prognosis for retinoblastoma?
The outlook depends on when it’s found and how well it’s treated. Early cases have a better chance of recovery.
How does retinoblastoma affect vision?
Vision loss varies by disease extent and treatment. Some treatments save vision, while others, like removing the eye, don’t.
What is the difference between retinoblastoma and its benign mimics?
Benign mimics look like retinoblastoma but aren’t cancer. It’s key to correctly diagnose to avoid unnecessary treatments.
What are some common benign mimics of retinoblastoma?
Common mimics include Persistent Fetal Vasculature, Coats’ disease, Retinopathy of Prematurity, ocular toxocariasis, and retinal astrocytic hamartomas.
How are benign mimics of retinoblastoma managed?
Management varies. Some need watching, while others require treatments like laser therapy or surgery.
Why is genetic counseling important in retinoblastoma?
Genetic counseling helps families understand the risk of passing the mutated RB1 gene. It’s about surveillance and prevention.
What is the role of a multidisciplinary team in diagnosing retinoblastoma?
A team of specialists is vital for accurate diagnosis and effective treatment of retinoblastoma.
How can families cope with a suspected retinoblastoma diagnosis?
Families can get support from healthcare, join support groups, and find resources for children with eye diseases.
References:
- Global Retinoblastoma Study Group. (2025). Early detection and MRI impact on retinoblastoma treatment outcomes: A multicenter cohort study. The Lancet Oncology, 26(1), 45-54.
https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(24)00276-3/fulltext





