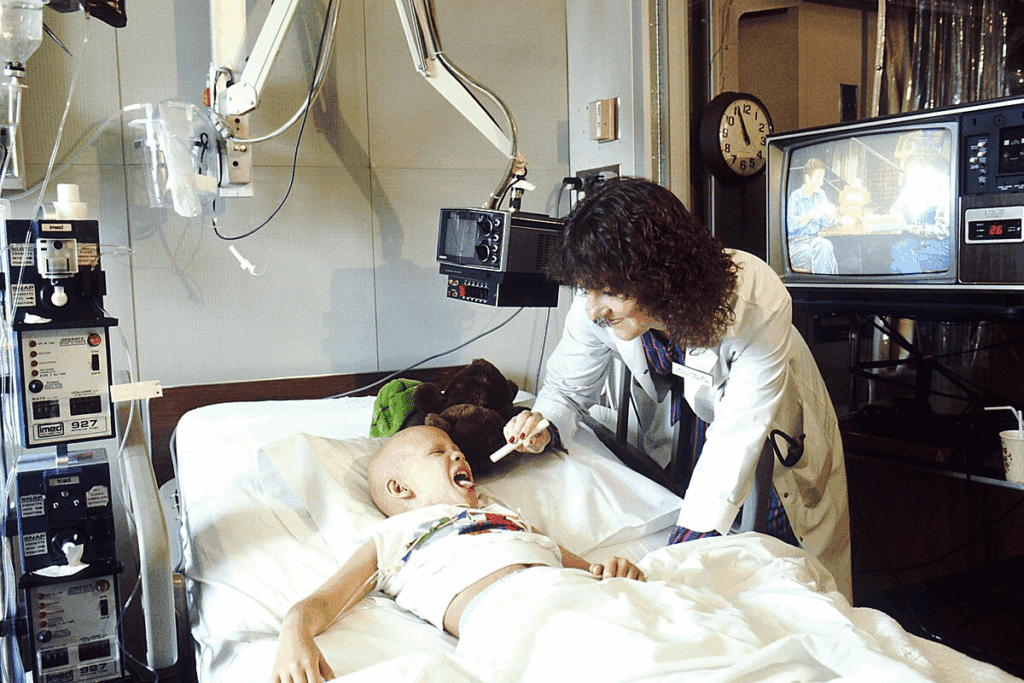
Diagnosing childhood leukemia often starts with a visit to the family doctor or a blood test that suggests a problem. The doctor will ask about symptoms and perform a physical exam. Based on this information, the doctor may refer the child to a specialist or order tests to check for leukemia or other health issues.
Laboratory tests play a key role in diagnosing and monitoring leukemia.Abnormal labs childhood leukemiaHow Is Leukemia Diagnosed? Crucial Blood Test Knowing which lab results are abnormal is vital for diagnosis and treatment planning.
Key Takeaways
- Blood tests are often the first step in diagnosing childhood leukemia.
- Laboratory tests help diagnose and monitor leukemia.
- Understanding abnormal lab results is key for treatment planning.
- A physical exam and medical history are also important in diagnosing leukemia.
- A specialist may be involved in the diagnosis and treatment process.
Understanding Childhood Leukemia

Childhood leukemia includes many types of blood cancers. It’s divided into two main types: acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). ALL is the most common, making up about 80% of cases.
Types of Childhood Leukemia
There are two main types of childhood leukemia: ALL and AML. Acute lymphoblastic leukemia (ALL) is when lymphoblasts, immature white blood cells, grow too much. On the other hand, acute myeloid leukemia (AML) is when myeloid cells grow too fast, filling the bone marrow with abnormal cells.
- ALL is the most common type, making up about 80% of childhood leukemia cases.
- AML is more aggressive and requires immediate treatment.
Pathophysiology and Its Impact on Laboratory Values
Leukemia is when abnormal white blood cells grow too much. This can change many lab results. These changes help doctors diagnose leukemia.
Leukemia significantly alters laboratory values. It can cause:
- Elevated white blood cell counts because of the growth of cancer cells.
- Anemia and low platelets because the bone marrow is filled up.
- Blast cells in the blood or bone marrow.
Importance of Early Laboratory Detection
Early detection is key to better treatment for kids with leukemia. Tests like complete blood counts (CBC) and bone marrow aspiration are very important. They help doctors diagnose and plan treatment.
Genetic testing and bone marrow aspiration are very important. They help find specific genetic problems and see how far the disease has spread. This helps doctors make treatment plans that fit each patient’s needs.
Abnormal Labs Childhood Leukemia: Complete Blood Count Findings
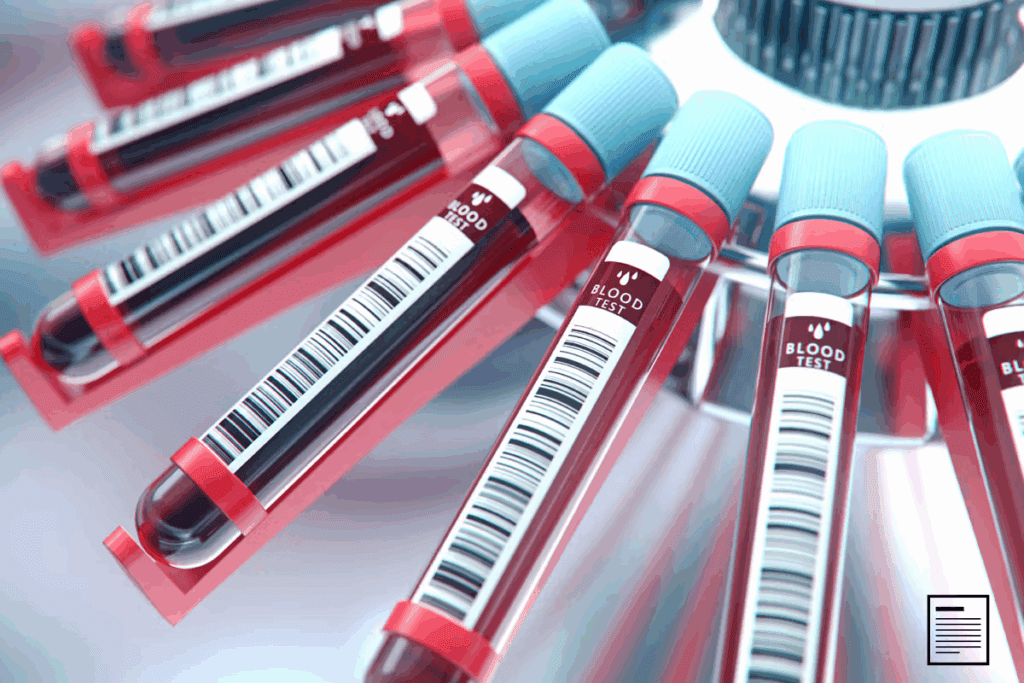
A CBC is key in finding childhood leukemia. It checks white blood cells, red blood cells, and platelets. If these counts are off, it might mean leukemia.
White Blood Cell Abnormalities
White blood cell issues are common in childhood leukemia. These can show up as leukocytosis, leukopenia, or an abnormal white cell differential.
Leukocytosis
Leukocytosis, or high white blood cell count, is seen in leukemia. This is because of the growth of bad cells.
Leukopenia
Leukopenia, or low white blood cell count, can also happen. It might be because of bad cells filling the bone marrow.
Abnormal White Cell Differential
An abnormal white cell differential shows blast cells or immature cells. This is a sign of leukemia.
Red Blood Cell Abnormalities
Red blood cell issues, like anemia, are common in children with leukemia.
Anemia Patterns in Childhood Leukemia
Anemia in leukemia can come from bone marrow failure or bad cells. This leads to fewer red blood cells.
Hemoglobin and Hematocrit Changes
Changes in hemoglobin and hematocrit show how severe anemia is. Low levels are common in leukemia patients.
| Parameter | Normal Range | Common Finding in Leukemia |
| Hemoglobin | 12-16 g/dL | Decreased |
| Hematocrit | 36-48% | Decreased |
Platelet Count Abnormalities
Platelet count issues, like thrombocytopenia, are common in leukemia.
Thrombocytopenia
Thrombocytopenia, or low platelet count, can come from bone marrow suppression or bad cells.
Rare Cases of Thrombocytosis
Thrombocytosis (high platelet count) is rare but can happen in some leukemia cases.
“The presence of thrombocytopenia in a child should prompt further investigation for leukemia, as it is a common presenting feature.”
Peripheral Blood Smear Examination
In diagnosing childhood leukemia, a key tool is the peripheral blood smear. It helps spot blast cells and other oddities. This test looks at blood under a microscope for abnormal cells.
Blast Cells in Peripheral Blood
Blast cells in the blood are a big sign of leukemia. These young cells shouldn’t be in healthy blood. Finding them helps doctors diagnose leukemia.
- Blast cells can differ in size and shape.
- Auer rods in blast cells point to acute myeloid leukemia (AML).
- The blast cell count shows how serious the disease is.
Morphological Abnormalities in Blood Cells
Other oddities in blood cells can also be seen in a blood smear. These include:
- Odd red blood cells, like anemia or poikilocytosis.
- Too few or too many platelets, showing platelet count issues.
- Strange white blood cells, like granulocytes and lymphocytes.
The Role of Blood Smear in Initial Diagnosis
The blood smear is key in starting to diagnose leukemia. It quickly shows if there are odd cells, helping plan next steps. It’s a fast and simple test, making it a first step in diagnosing leukemia in kids.
Healthcare providers use the blood smear to:
- See if more tests, like bone marrow aspiration, are needed.
- Understand how serious the disease is by looking at abnormal cells.
- Choose the best treatment plan.
Bone Marrow Examination Findings
Diagnosing childhood leukemia relies heavily on bone marrow examination findings. This process checks the bone marrow for leukemia cells. It helps understand the disease’s stage and plan the right treatment.
Bone Marrow Aspiration Results
Bone marrow aspiration takes a sample using a needle. The sample is then checked for blast cells, which are key signs of leukemia.
The results show the leukemia type, its severity, and how much bone marrow is affected.
Bone Marrow Biopsy Findings
A bone marrow biopsy removes a small bone and marrow sample. It’s vital for checking the cellularity and any changes in the bone marrow.
Biopsy results add to the understanding of the disease’s impact on the bone marrow.
Blast Percentage and Significance
The blast cell percentage is key in diagnosing leukemia. More blasts mean a more aggressive disease. Fewer blasts might show a milder condition or a treatment success.
Knowing the blast percentage helps doctors decide on the treatment’s intensity.
Cellularity and Morphological Changes
The bone marrow’s cellularity shows how much space is filled with blood-making cells. In leukemia, this space can be filled with cancer cells.
Seeing abnormal cell shapes is also important. These signs help diagnose the leukemia type and understand its cause.
“The bone marrow examination is a cornerstone in the diagnosis of leukemia, providing essential information on the disease’s characteristics and guiding treatment decisions.” A medical expert
Biochemical Markers and Serum Abnormalities
Childhood leukemia shows up in lab tests through various biochemical changes. These changes help doctors diagnose, predict outcomes, and manage the disease.
Lactate Dehydrogenase (LDH) Elevation
Children with leukemia often have high LDH levels. LDH is an enzyme in many body tissues. High levels suggest tissue damage or fast cell growth, typical in leukemia.
Uric Acid Levels
High uric acid levels are common in childhood leukemia. This happens because cancer cells break down quickly, releasing substances that turn into uric acid.
Electrolyte Imbalances
Leukemia and its treatment can cause electrolyte imbalances. This includes changes in potassium, phosphate, and calcium levels.
Tumor Lysis Syndrome Markers
Tumor lysis syndrome (TLS) is a serious side effect of leukemia treatment. It’s marked by high LDH, uric acid, potassium, and phosphate, and low calcium levels.
| Biochemical Marker | Abnormality in Leukemia | Clinical Significance |
| Lactate Dehydrogenase (LDH) | Elevated | Indicates tissue damage or rapid cell turnover |
| Uric Acid | Elevated | Result of rapid breakdown of cancer cells |
| Potassium | Elevated | Part of tumor lysis syndrome |
| Phosphate | Elevated | Part of tumor lysis syndrome |
| Calcium | Decreased | Associated with elevated phosphate levels |
Understanding these biochemical markers helps doctors better diagnose and treat childhood leukemia. This leads to better patient outcomes.
Organ Function Tests in Childhood Leukemia
Organ function tests are key in checking the health of kids with leukemia. They show how the disease impacts different organs. This info is vital for picking the right treatment.
Liver Function Test Abnormalities
The liver is important for many things, like breaking down food and making proteins. Tests for liver function are very important. They can show if leukemia is affecting the liver.
Transaminases and Bilirubin
High levels of transaminases (like ALT and AST) and odd bilirubin levels mean liver damage. In leukemia, this could be because of the disease itself or treatment side effects.
Albumin Levels
Low albumin levels can mean poor nutrition or liver problems. Keeping an eye on albumin is important for kids with leukemia. It shows how well they’re doing and can help decide treatment.
Kidney Function Abnormalities
Kidney tests are important for checking how well the kidneys work. Leukemia and its treatment can harm the kidneys. So, these tests are very important.
Blood Urea Nitrogen and Creatinine
High BUN and creatinine levels mean the kidneys might not be working right. These tests help find kidney problems early. This way, doctors can act fast.
Glomerular Filtration Rate Changes
The GFR shows how well the kidneys are working. Changes in GFR can mean kidney damage or disease. This is a big worry for kids with leukemia.
In summary, tests for organ function are very important in treating childhood leukemia. By watching liver and kidney health closely, doctors can make better treatment plans. This helps improve how well kids do.
Genetic and Molecular Diagnostic Tests
Understanding leukemia’s genetic and molecular basis is key for accurate diagnosis and treatment. Genetic and molecular tests help find specific genetic flaws linked to leukemia.
Cytogenetic Analysis
Cytogenetic analysis looks at leukemia cells’ chromosomes. It spots chromosomal issues tied to various leukemia types.
Fluorescence In Situ Hybridization (FISH)
FISH is a lab method to find and pinpoint genetic flaws in cells. It’s great for spotting leukemia-linked genetic changes.
Polymerase Chain Reaction (PCR) Testing
PCR testing is super sensitive for finding minimal residual disease. It spots tiny leukemia cells left after treatment.
Next-Generation Sequencing
Next-generation sequencing (NGS) quickly sequences big DNA or RNA chunks. It finds many leukemia-linked genetic mutations.
Prognostic Implications of Genetic Findings
The genetic results from these tests are very important. They help figure out risk levels, decide treatment intensity, and predict outcomes.
| Test | Description | Significance |
| Cytogenetic Analysis | Examines chromosomes in leukemia cells | Identifies chromosomal abnormalities |
| FISH | Detects specific genetic abnormalities | Useful in diagnosing genetic changes |
| PCR Testing | Detects minimal residual disease | Monitors treatment response |
| Next-Generation Sequencing | Sequences large stretches of DNA/RNA | Identifies multiple genetic mutations |
Interpreting Laboratory Results: Diagnostic Approach
Understanding lab findings is key to diagnosing and managing leukemia. It involves knowing the different tests used and what they mean.
Initial Screening vs. Confirmatory Tests
First, a complete blood count (CBC) is done to check for leukemia. It looks for odd blood cell counts that might show leukemia.
Then, tests like bone marrow aspiration and biopsy confirm the diagnosis. They show if leukemia cells are present and what they look like.
Differential Diagnosis Based on Lab Findings
Lab results help tell different types of leukemia apart. For example, certain genetic changes can tell if it’s acute lymphoblastic leukemia (ALL) or acute myeloid leukemia (AML).
Laboratory Monitoring During Treatment
While treating leukemia, labs check how well the treatment is working. They look at blood cell counts, liver, and kidney function.
Based on these tests, doctors can change the treatment plan to get better results.
Minimal Residual Disease Detection
Checking for minimal residual disease (MRD) is very important in leukemia care. MRD means small leukemia cells are left after treatment.
Tests like polymerase chain reaction (PCR) and flow cytometry find MRD. Knowing if MRD is present helps decide on treatment and how well the patient will do.
Conclusion
Childhood leukemia is diagnosed and monitored through lab tests. These tests find different kinds of problems. The Complete Blood Count (CBC), Peripheral Blood Smear Examination, Bone Marrow Examination, and biochemical markers are key.
It’s important for doctors to understand these lab results. This helps them manage the disease well and improve patient care. By correctly reading lab results, doctors can spot leukemia early, start the right treatment, and keep track of how the disease is doing.
Lab findings are very important in treating childhood leukemia. They help doctors work with the patient’s symptoms to give the best care. This way, doctors can make treatment plans that really help kids with leukemia live better lives.
FAQ
What are the common lab tests used to diagnose childhood leukemia?
To diagnose childhood leukemia, doctors use several tests. These include complete blood counts (CBC), peripheral blood smear exams, and bone marrow tests. They also check for biochemical markers like lactate dehydrogenase (LDH) and uric acid levels.
What abnormalities are typically seen in a CBC for childhood leukemia?
In a CBC for childhood leukemia, doctors look for certain signs. These include too many or too few white blood cells, anemia, and low platelet counts.
What is the significance of blast cells in a peripheral blood smear?
Blast cells in a blood smear are a key sign of leukemia. These cells are immature and shouldn’t be in the blood.
How is bone marrow examination used in the diagnosis of leukemia?
Bone marrow exams help diagnose leukemia. They check for blast cells, the marrow’s cell count, and any changes. This info is vital for making a diagnosis.
What biochemical markers are commonly elevated in childhood leukemia?
In childhood leukemia, LDH and uric acid levels often rise. These markers show how the disease affects the body’s metabolism.
How do genetic and molecular diagnostic tests contribute to the diagnosis of leukemia?
Genetic and molecular tests, like cytogenetic analysis and PCR, are key. They find specific genetic changes. This helps doctors choose treatments and predict outcomes.
What is the role of organ function tests in childhood leukemia?
Organ function tests check how leukemia affects the body. They help doctors decide on treatments and monitor progress.
How are laboratory results interpreted in the diagnosis of childhood leukemia?
Doctors interpret lab results by comparing screening and confirmatory tests. They also watch for cancer cells left after treatment.
What is minimal residual disease detection, and why is it important?
Minimal residual disease detection finds small cancer cells left after treatment. It’s important for checking treatment success and planning further care.
Can leukemia cause abnormalities in liver function tests?
Yes, leukemia can affect liver function tests. This might be due to the disease itself or treatment side effects.
Are genetic testing and bone marrow aspiration necessary for diagnosing leukemia?
Yes, genetic testing and bone marrow aspiration are often needed. They help diagnose leukemia and provide important information for treatment planning.
References
- Vallet, P., et al. (2024). Infections in children and adolescents with Acute Leukemia. European Journal of Pediatrics. https://www.sciencedirect.com/science/article/pii/S2772610X24000011