Last Updated on October 22, 2025 by mcelik

Every year, nearly 225,000 people in the United States are diagnosed with lung cancer. Many of these cases begin with the discovery of lung nodules during screenings. A 7mm nodule can raise concern, but its risk often depends on cancerous lung nodule locations within the lung.
Nodules found in the upper lobes, for example, are more likely to be malignant compared to those in lower lobes. Understanding whether a nodule is cancerous and its exact location is crucial for assessing risk and planning the next steps in diagnosis and treatment.
Key Takeaways
- The size and location of a lung nodule are critical in assessing its potential to be cancerous.
- A 7mm nodule is considered small, but its positioning can affect the risk assessment.
- Understanding the stage and location of lung cancer is vital for treatment planning.
- Lung nodule screenings are key for early detection of lung cancer.
- The American Cancer Society provides valuable resources for understanding lung cancer and nodule risks.
What Are Lung Nodules?
Lung nodules are small growths in the lungs. They can be harmless or cancerous. Often, they are found by accident during chest scans. These pulmonary nodules come in different sizes and shapes. Knowing their details is key to figuring out if they are serious.
Definition and Characteristics
Lung nodules are usually round or oval and less than 3 cm in size. They can be alone or in groups. Their look on scans can vary, like being solid or partly solid.
The size, shape, and density of these nodules give clues about what they might be.
Common Causes of Lung Nodules
Lung nodules can come from many sources. Some are harmless, like infections or granulomas. Others are cancerous tumors. Infectious granulomas might come from old infections like tuberculosis.
Benign tumors and inflammation can also cause them.
Prevalence in the General Population
Lung nodules are quite common, thanks to more computed tomography (CT) scans. Many people have them, but most are not serious. The chance of having them goes up with age and if you smoke or are exposed to certain things.
The Significance of Nodule Size: Focus on 7mm
The size of a lung nodule, like one that’s 7mm, is very important. These small tissue masses can be harmless or cancerous. Their size helps doctors figure out if they might be cancer.
Size Classification of Lung Nodules
Lung nodules are sorted by size to gauge their cancer risk. The Fleischner Society Guidelines set these size groups. They guide how often to check and manage these nodules.
What a 7mm Measurement Means Clinically
A 7mm lung nodule is not too big, but not too small either. It needs close attention. Doctors recommend regular imaging to watch for any changes.
Size as a Predictor of Malignancy Risk
The size of a lung nodule affects its cancer risk. Bigger nodules are more likely to be cancerous. But, even small ones, like 7mm, can be cancerous. This means they need careful monitoring.
Knowing how big a nodule is, like a 7mm one, is key. It helps doctors decide the best course of action. By looking at size and characteristics, they can manage patient care better.
Benign vs. Malignant Lung Nodules
It’s important to know the difference between benign and malignant lung nodules. These nodules are small, round tissue masses found in lung scans. They can be a sign of health or a serious issue.
Characteristics of Benign Nodules
Benign nodules are not cancerous. They don’t spread or grow into other tissues. They often look different on scans because they are calcified or have a unique shape. Types include granulomas, hamartomas, and inflammatory nodules.
Warning Signs That Suggest Malignancy
Malignant nodules are cancerous. They can grow and spread. Signs of cancer on scans include irregular borders, spiculated margins, and rapid growth. These signs might mean you need more tests, like a biopsy.
Statistical Likelihood Based on Size and Features
The chance of a nodule being cancerous depends on its size and look. Bigger nodules and those with suspicious signs are more likely to be cancer. A 7mm nodule has a low but not zero chance of being cancerous, more so in people at high risk.
Doctors use rules and models, like the Fleischner Society’s, to guess the risk. These help decide if more tests or scans are needed. They guide how to check if a nodule is cancerous.
Cancerous Lung Nodule Locations and Their Significance
The location of lung nodules is very important. It helps doctors figure out if a nodule might be cancer. Where the nodule is in the lung can tell a lot about its chance of being cancerous.
Upper Lobe Cancer Distribution Patterns
Lung nodules that are cancerous often show up in the upper lobes. Upper lobe cancer is common. This is because of smoking and how the lung is structured.
The upper lobes get hit hard by tobacco-related carcinogens. Most lung cancers start here. So, doctors watch these areas closely.
Peripheral vs. Central Nodule Implications
There’s a big difference between peripheral nodules and central lung nodules. Peripheral nodules are on the outside, while central ones are near the airways.
Peripheral nodules are often adenocarcinoma, a common lung cancer. Central nodules, being closer to the airways, can cause coughing and breathing trouble.
Right vs. Left Lung Cancer Prevalence
Lung cancer is more common in the right lung than the left lung. This might be because the right lung is bigger and gets more carcinogens.
Doctors need to know these patterns to manage lung nodules well. The location of a nodule affects its risk and treatment plan.
Risk Factors That Increase Concern for a 7mm Nodule
Knowing the risk factors for a 7mm lung nodule is key. It helps figure out if cancer is likely. Some factors make cancer more of a concern for nodules this size.
Smoking History and Pack-Years
Smoking is a big risk for lung cancer. The risk goes up with pack-years. People with more pack-years are at higher risk.
For example, smoking one pack a day for 30 years means 30 pack-years. This puts someone in a higher risk group.
| Pack-Years | Lung Cancer Risk Level |
| 0 | Low |
| 1-20 | Moderate |
| 21+ | High |
Age and Gender Considerations
Age is a big factor, with risk going up after 50. Gender also matters, with some groups at higher risk. Knowing these factors helps understand the overall risk.
Family History of Lung Cancer
A family history of lung cancer might mean a genetic risk. People with a first-degree relative with lung cancer might be at higher risk.
Previous Cancer Diagnosis
Having had cancer before changes the risk for a new nodule. The type and stage of the cancer, and the treatment are important.
Healthcare providers use these risk factors to assess a 7mm lung nodule. They can then decide the best next steps.
Diagnostic Procedures for Evaluating Lung Nodules
Diagnostic procedures are key in checking lung nodules. They help doctors figure out if the nodule is harmless or cancerous. This information guides the treatment plan.
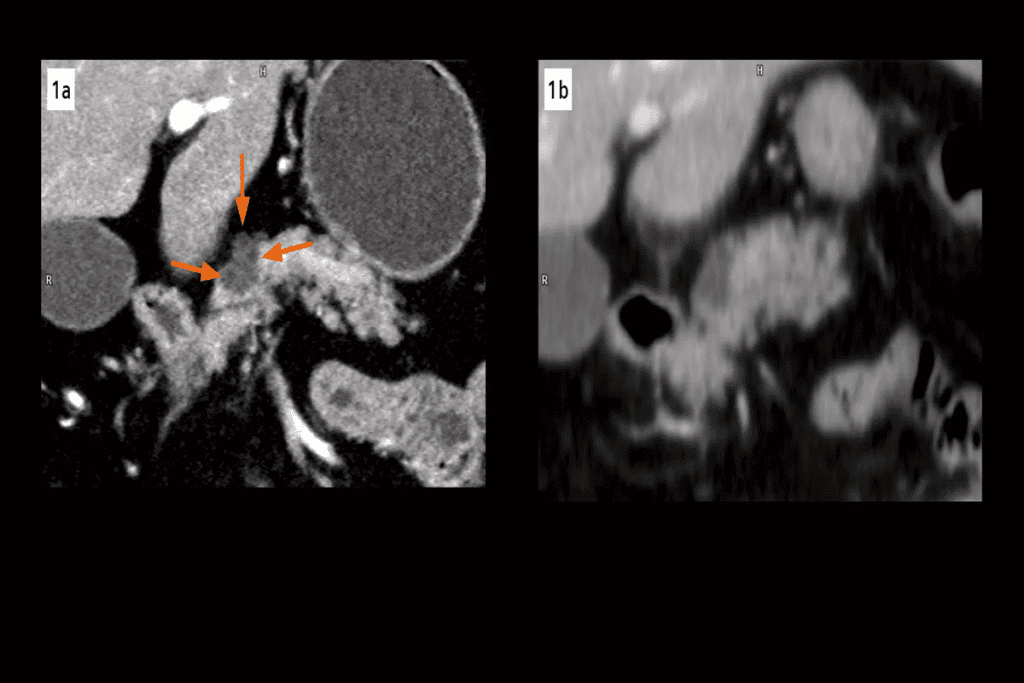
Imaging Studies: CT, PET, and MRI
Imaging studies are vital for lung nodule checks. Computed Tomography (CT) scans give detailed lung images. They help track nodule size and shape over time.
Positron Emission Tomography (PET) scans show how active the nodule is. This can tell if it’s cancer. Magnetic Resonance Imaging (MRI) is less used but helpful in some cases.
| Imaging Modality | Primary Use | Key Benefits |
| CT Scan | Monitoring nodule size and characteristics | High-resolution images, detailed nodule assessment |
| PET Scan | Assessing metabolic activity | Helps identify cancerous nodules based on metabolic activity |
| MRI | Specific situations where CT or PET is not suitable | Useful for patients who cannot undergo CT or PET scans |
Biopsy Options and Procedures
Biopsy takes a tissue sample from the nodule for lab tests. There are percutaneous needle biopsy and transbronchial biopsy options. The choice depends on the nodule’s location and the patient’s health.
Bronchoscopy and Other Minimally Invasive Techniques
Bronchoscopy lets doctors see the airways and take samples. Techniques like navigational bronchoscopy help diagnose nodules without major surgery.
The Fleischner Society Guidelines for 7mm Nodules
The Fleischner Society Guidelines play a big role in managing 7mm lung nodules. They offer a clear plan for checking and handling these nodules. This plan depends on the nodule’s size and the patient’s risk factors.
Current Recommendations Based on Risk Factors
The guidelines look at several things to figure out the risk of cancer in lung nodules. These include the patient’s age, smoking history, and the nodule’s features. For a 7mm nodule, the approach changes based on the patient’s risk level.
Follow-up Intervals for Monitoring
For patients at low risk with a 7mm nodule, a CT scan is suggested every 6-12 months. Those at high risk might need more checks, like a PET scan or other tests.
| Risk Category | Recommended Follow-up |
| Low Risk | CT scan at 6-12 months |
| High Risk | PET scan or more frequent CT scans |
When Immediate Action Is Warranted
Right away, action is needed if the nodule looks suspicious. This includes features like spiculation, large size, or quick growth. In these cases, a biopsy or other tests are often advised.
By sticking to the Fleischner Society Guidelines, doctors can make smart choices about 7mm lung nodules. They aim to be careful without doing too much.
Upper Lobe Cancer: Patterns and Concerns
Lung cancer often starts in the upper lobes. This makes them a key area for doctors to check and treat. The upper lobes get cancer more often because of their shape and what we breathe in.
Why Upper Lobes Are Common Sites for Malignancy
The upper lobes get cancer more because of their shape and what we breathe in. Anatomical factors like the bronchi’s structure and gravity’s pull on lung tissue help explain this. Also, environmental exposures, like breathing in harmful substances, play a big role in cancer here.
- The upper lobes get more of the harmful stuff we breathe in, raising cancer risk.
- Gravity’s pull affects how lung tissue and harmful substances settle.
Right Upper Lobe Nodule Significance
Nodules in the right upper lobe are very worrying because they might be cancerous. Research shows lung cancer is more common in the right lung than the left, with the upper lobe being a hotspot.
- The size and spot of the nodule are key in figuring out cancer risk.
- Things like smoking and family history of lung cancer affect how serious a nodule is.
Left Upper Lobe Cancer Patterns
Left upper lobe cancer is less common but just as serious. Cancer patterns in the left upper lobe can vary from the right, with different types and behaviors of tumors.
Knowing these patterns is key for finding and treating cancer effectively. The tumor’s location and details help doctors choose the best treatment.
Peripheral Nodules vs. Central Masses: Location Matters
The place of a lung nodule is key in figuring out its health risks and treatment. Lung nodules fall into two main types: peripheral nodules and central masses. Each type has its own traits and challenges.
Subpleural Nodules and Their Clinical Implications
Subpleural nodules sit near the lung’s edge, close to the pleura. They tend to have a lower risk of being cancerous than central ones. Yet, they can be cancerous and need a thorough check-up. Because they’re on the lung’s edge, they’re easier to reach for biopsies and treatments.
Subpleural nodules are known for:
- Being near the pleura
- Generally having a lower cancer risk
- Being easier to get to for tests and treatments
Central Lung Cancer Characteristics and Challenges
Central lung cancer starts in the lung’s main airways and tends to grow fast. It can cause coughing, bleeding, and pneumonia because of its central spot. Treating central lung cancer is tough because it’s hard to get to and there’s a higher chance of problems during treatment.
Central lung cancer is marked by:
- Starting in the main airways
- Being more aggressive
- Having a higher risk of treatment complications
Outer Lung Tumors: Accessibility and Treatment Options
Outer lung tumors, like subpleural nodules, are easier to treat because they’re on the lung’s edge. Treatments might include surgery, radiation, or other small procedures. The best treatment depends on the tumor, the patient’s health, and other factors.
The choice of treatment for outer lung tumors depends on the tumor’s size, location, and the patient’s overall health.
Lung Cancer Types and Their Typical Anatomical Distribution
It’s important to know the different types of lung cancer and where they usually grow. Lung cancer is divided into types based on cell type and how they look under a microscope. Each type grows in a specific area of the lung.
Adenocarcinoma Location Patterns and Prevalence
Adenocarcinoma is the most common lung cancer, often found in non-smokers. It grows in the outer lung parts, mainly in the upper lobes. This type is more common in women and is increasing in prevalence.
Characteristics of Adenocarcinoma:
- Often peripheral in location
- May be associated with scar tissue
- Tends to grow more slowly than other types
Squamous Cell Carcinoma Distribution
Squamous cell carcinoma is linked to smoking and grows in the central airways. It’s usually found near the lung’s hilum and can block major airways, causing symptoms.
Key Features:
- Central location, often causing airway obstruction
- Cavitation can occur, leading to a characteristic appearance on imaging
- Linked to smoking history
Small Cell Lung Cancer Presentation
Small cell lung cancer is aggressive and linked to smoking. It grows in the central airways and spreads quickly, often with widespread metastasis at diagnosis.
Presentation Characteristics:
- Central location with early metastasis
- Often associated with paraneoplastic syndromes
- Rapid growth and poor prognosis
Large Cell Carcinoma Anatomical Patterns
Large cell carcinoma includes undifferentiated non-small cell lung carcinomas. It can grow anywhere in the lung and spreads quickly.
Notable Features:
- Can occur in any part of the lung
- Lacks the distinct features of other lung cancer types
- Tends to have a poor prognosis due to late diagnosis
Knowing where lung cancer types grow is key for diagnosis and treatment. This knowledge helps doctors plan care and improve outcomes for patients.
| Lung Cancer Type | Typical Location | Characteristics |
| Adenocarcinoma | Peripheral, Upper Lobes | Slow-growing, associated with scar tissue |
| Squamous Cell Carcinoma | Central, near Hilum | Cavitation, linked to smoking |
| Small Cell Lung Cancer | Central Airways | Aggressive, early metastasis, paraneoplastic syndromes |
| Large Cell Carcinoma | Anywhere in the Lung | Undifferentiated, poor prognosis |
Non-Cancerous Causes of 7mm Lung Nodules
Finding a 7mm lung nodule can be scary. But, it’s important to know that many nodules are not cancer. They can come from different non-cancerous reasons.
Infectious Granulomas and Their Appearance
Infectious granulomas are a common reason for lung nodules. They happen when the body fights off infections like tuberculosis or histoplasmosis. These granulomas can look like cancer on scans.
Hamartomas and Other Benign Tumors
Hamartomas are small, benign tumors in the lung. They are made of different tissues like cartilage, fat, and muscle. Other benign tumors, like adenomas and fibromas, can also show up as nodules.
Inflammatory Conditions That Mimic Cancer
Some inflammatory conditions, like rheumatoid arthritis or sarcoidosis, can cause lung nodules. These nodules are not cancer. They are part of the body’s fight against inflammation.
Post-Infectious Scarring and Calcifications
Old infections can leave scars or calcifications in the lung. These can look like nodules on scans. They are usually harmless and show the body’s healing process.
To understand lung nodules better, let’s look at their differences:
| Cause | Typical Characteristics |
| Infectious Granulomas | Often calcified, may be associated with infection history |
| Hamartomas | Contain fat, may have a characteristic “popcorn” calcification |
| Inflammatory Conditions | May be multiple, associated with systemic symptoms |
| Post-Infectious Scarring | Often have a history of previous infection, may be stable over time |
Knowing the non-cancerous reasons for 7mm lung nodules is key for correct diagnosis and treatment. Doctors look at the nodule’s features and the patient’s history. This helps them figure out the cause and what to do next.
Monitoring and Follow-up Protocols for 7mm Nodules
Managing 7mm lung nodules requires careful monitoring and follow-up. These steps help spot changes early. This is key for deciding the best next steps.
Surveillance Imaging Schedules Based on Risk
The timing of surveillance imaging for 7mm nodules varies by risk. Those at higher risk for lung cancer might need more frequent scans. Risk-based schedules make sure monitoring fits each person’s needs, keeping a closer eye on those at higher risk.
Concerning Changes in Size, Shape, and Density
Any changes in size, shape, or density of the nodule are watched closely. An increase in size or changes in density could mean cancer. Regular imaging catches these changes early, allowing for quick action if needed.
When to Consider More Aggressive Evaluation
If changes raise concerns, a more detailed check might be needed. This could include more scans or biopsy procedures to figure out the nodule’s nature. The choice to go for more detailed evaluation depends on the person’s risk and the nodule’s features.
By sticking to these monitoring and follow-up plans, doctors can manage 7mm lung nodules well. This way, any problems can be tackled quickly.
Treatment Options If a Nodule Is Concerning
When a lung nodule is concerning, several treatment options are available. These depend on the nodule’s size, location, and other factors. A team of healthcare experts works together to decide the best course of action. They consider the patient’s health, medical history, and the nodule’s details.
Surgical Approaches Based on Nodule Location
Surgery is often the first choice for concerning lung nodules. The type of surgery depends on where the nodule is. For nodules on the lung’s edge, video-assisted thoracic surgery (VATS) is used. This method is less invasive and helps patients recover faster.
Nodules closer to the airways might need a more open surgery. This approach is more traditional but sometimes necessary.
Radiation Therapy Options for Different Lung Zones
Radiation therapy is another option for lung nodules. It’s best for those who can’t have surgery or have hard-to-reach nodules. Stereotactic body radiation therapy (SBRT) is very precise. It targets the nodule with high doses while protecting healthy tissue.
The choice of radiation therapy depends on the nodule’s location and the patient’s health.
Emerging Minimally Invasive Techniques
New, less invasive methods are being explored for lung nodules. Minimally invasive techniques like percutaneous ablation and bronchoscopic ablation aim to reduce complications. These methods are promising for treating nodules with fewer side effects.
Treatment Decisions Based on Nodule Positioning
The nodule’s location in the lung affects treatment choices. Below is a table showing treatment options based on location:
| Nodule Location | Preferred Treatment | Alternative Options |
| Peripheral | VATS | SBRT, Percutaneous Ablation |
| Central | Open Thoracotomy | Radiation Therapy, Bronchoscopic Ablation |
| Upper Lobe | Surgical Resection | SBRT |
Treatment plans are tailored to each patient. They consider the nodule’s details, the patient’s health, and the latest medical technology.
Living with Uncertainty: Psychological Aspects
Getting a lung nodule diagnosis is tough. It brings a lot of uncertainty into your life. This can really affect how you feel every day. Worrying about cancer and test results can feel too much to handle.
Coping with “Watchful Waiting” Anxiety
The “watchful waiting” time is hard. You might feel really anxious waiting for test results. Learning to cope with this can help. Things like mindfulness, meditation, or joining a support group can ease your mind.
Knowing more about your condition and why doctors are waiting can also help. It can make you feel more at ease.
When to Seek a Second Opinion
Getting a second opinion is important if you’re unsure. It lets you double-check your diagnosis and look at other treatment choices. Don’t be afraid to ask for more medical advice if you’re worried.
Support Resources for Patients with Lung Nodules
Having support resources is key. There are online forums, support groups, and counseling services out there. They help you deal with the emotional side of your diagnosis. They also offer a sense of community and understanding.
Communicating with Healthcare Providers
Talking openly with your doctors is important. You should ask questions about your condition and treatment. Good communication builds trust and makes sure you get the care you need.
Conclusion: Putting a 7mm Lung Nodule in Perspective
Understanding a 7mm lung nodule is complex. It involves looking at risk factors, nodule details, and treatment choices. A 7mm lung nodule can worry people, but its importance varies. It depends on where it is, how big it is, and the patient’s health.
Managing lung nodules well means checking these factors closely. Knowing the difference between benign and malignant nodules helps patients. This knowledge aids in understanding diagnosis and treatment.
Looking at a 7mm lung nodule in the big picture is key. Healthcare providers should consider the patient’s health and medical history. This way, they can offer tailored advice and treatments. It helps lower lung cancer risk and improves health outcomes. This approach encourages patients to be involved in their care.
FAQ
What is a lung nodule?
A lung nodule is a small growth in the lung, usually under 3 cm. It can be harmless or cancerous.
What does a 7mm lung nodule mean?
A 7mm lung nodule is small. Its importance depends on several factors. These include the patient’s health, the nodule’s features, and where it is located.
Are all lung nodules cancerous?
No, most lung nodules are not cancer. But, the chance of cancer grows with the nodule’s size and certain characteristics.
What are the risk factors for a malignant lung nodule?
Risk factors include smoking, age, family history of lung cancer, and previous cancers. Genetic mutations also play a role.
How are lung nodules diagnosed?
Diagnosis uses imaging like CT and PET scans, biopsies, and bronchoscopy. The choice depends on the nodule and patient factors.
What are the Fleischner Society Guidelines for 7mm nodules?
The guidelines suggest follow-up based on risk. High-risk patients need more frequent checks.
Can a 7mm nodule be cancerous if it’s in the upper lobe?
Yes, upper lobe nodules can be cancerous. The upper lobes are common sites for lung cancer, mainly in smokers.
What is the difference between peripheral and central lung nodules?
Peripheral nodules are in the outer lung. Central nodules are near the hilum. Peripheral nodules are more common in adenocarcinoma, while central nodules are typical of squamous cell carcinoma.
How are lung nodules monitored?
Monitoring uses regular CT scans. These track changes in size, shape, and density of the nodule.
What are the treatment options for concerning lung nodules?
Treatment varies based on the nodule, patient risk, and diagnosis. Options include surgery, radiation, and new, less invasive methods.
How can I cope with the uncertainty of a lung nodule diagnosis?
Seek support from healthcare and consider second opinions. Use patient resources to manage anxiety and uncertainty.
Are there non-cancerous causes of lung nodules?
Yes, many nodules are benign. They can be caused by infections, hamartomas, inflammation, or scarring after an infection.
Can lung nodules be a sign of lung cancer?
Yes, nodules can be an early sign of lung cancer. But, most are benign. A cancer diagnosis needs more tests and evaluation.
References
- Chu, Z., et al. (2019). Primary solid lung cancerous nodules with different sizes: Distribution and CT features. BMC Cancer. Retrieved from https://bmccancer.biomedcentral.com/articles/10.1186/s12885-019-6274-0 BioMed Central
- Loverdos, K., et al. (2019). Lung nodules: A comprehensive review on current Nodule Classification, Risk Stratification, and Imaging Strategies. PMC (Frontiers/Review). Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6784443/