Did you know brain tumors are the second most common cancer in kids? Medulloblastoma is the top malignant brain tumor in children. It greatly affects young lives.
We are a leading institution in treating brain tumors in kids. Medulloblastoma needs a detailed approach. Our team is committed to delivering world-class healthcare with care and skill.
Key Takeaways
- Medulloblastoma is the most common malignant brain tumor in children.
- Early diagnosis is key for effective treatment.
- Our care includes the latest treatments and support services.
- International patients get personalized care and support.
Understanding Pediatric Brain Tumors
It’s important to understand pediatric brain tumors to find better treatments. These tumors are different in how they grow, where they are, and how they act. They are a big group of cancers in kids.
Prevalence and Statistics
Pediatric brain tumors are the second most common cancer in kids, after leukemia. They make up about 25% of all childhood cancers. The chance of getting these tumors changes with age.
Medulloblastoma is more common in young kids. Glioblastoma is more likely in older kids and teens.
We don’t know what causes most pediatric brain tumors. But, we know some genetic syndromes and environmental factors can raise the risk. New ways to look at tumors and study their genes have helped us understand them better.
Classification of Pediatric Brain Tumors
Pediatric brain tumors are sorted by how they look under a microscope, their genetic makeup, and where they are in the brain. The main types are:
- Astrocytomas: These tumors start from astrocytes, a kind of brain cell. They can be low-grade or high-grade.
- Ependymomas: These tumors come from ependymal cells in the brain’s ventricles. They can grow anywhere in the ventricular system.
- Medulloblastomas: These are aggressive tumors that start in the cerebellum. They can spread through the cerebrospinal fluid.
Knowing the exact type and details of a tumor is key to choosing the right treatment. It also helps predict how well the child might do.
Medulloblastoma: The Most Common Malignant Brain Tumor in Children
Medulloblastoma is a serious brain tumor mainly found in kids. It has different types that affect treatment.
Definition and Characteristics
Medulloblastoma starts in the cerebellum or posterior fossa. It grows fast and can spread through the cerebrospinal fluid (CSF). Early diagnosis is critical because it progresses quickly.
Symptoms vary based on the tumor’s location and size. Common signs include headaches, vomiting, and ataxia. Some kids might also see changes in their vision or personality.
Molecular Subtypes of Medulloblastoma
Recent studies have found four main types of medulloblastoma: WNT, SHH, Group 3, and Group 4. Each type has its own traits that affect treatment and how well a child will do.
The WNT subtype has a better outlook, while the SHH subtype is in between. Group 3 and Group 4 are harder to treat because they grow fast and spread easily.
Knowing about these subtypes helps us find better treatments. At our place, we keep up with the latest research to give kids with medulloblastoma the best care.
Other Common Pediatric Brain Tumors
Pediatric brain tumors include astrocytomas, ependymomas, and DIPG. Each has its own characteristics and treatment needs. Knowing about them helps in managing these tumors effectively.
Astrocytomas
Astrocytomas come from astrocytes, a brain cell type. They are the most common glioma in kids. These tumors can be slow-growing or aggressive.
Characteristics and Treatment: Slow-growing astrocytomas might need surgery or just watching. But aggressive ones require surgery, radiation, and chemotherapy.
Ependymomas
Ependymomas start from cells in the brain’s ventricles and spinal cord. They often appear in the back of the brain.
Treatment Approaches: Surgery is key for ependymomas. Sometimes, radiation is added based on the tumor’s type and how much was removed.
Diffuse Intrinsic Pontine Glioma (DIPG)
DIPG is a fast-growing brain tumor in kids. It starts in the pons and spreads into the brain.
Current Treatment Landscape: DIPG is hard to treat. Options include radiation and new treatments in trials.
| Tumor Type | Common Location | Typical Treatment Approaches |
| Astrocytoma | Varies (e.g., cerebellum, optic pathway) | Surgery, radiation therapy, chemotherapy |
| Ependymoma | Posterior fossa, spinal cord | Surgery, radiation therapy |
| DIPG | Pons (brainstem) | Radiation therapy, clinical trials |
It’s important to know about these tumors to plan better treatments. We’re always learning and improving to help kids with these conditions.
Pilocytic Astrocytoma: The Most Common Benign Brain Tumor in Children
Pilocytic astrocytoma is a common benign brain tumor in kids.
Characteristics and Location
This tumor grows slowly and often appears in the cerebellum. It can also be found in other brain areas like the optic pathway or brainstem. This tumor is known for its cystic appearance with a mural nodule, which helps doctors diagnose it.
The cerebellum is where this tumor usually shows up. Symptoms can include trouble with coordination and balance. This is because the tumor affects the brain around it.
Prognosis and Treatment Approach
Children with pilocytic astrocytoma usually have a good chance of recovery.
If surgery isn’t possible, other treatments like chemotherapy or targeted therapy might be used. The choice of treatment depends on the tumor’s size, location, and the child’s health.
| Treatment Modality | Indications | Benefits |
| Surgical Resection | Accessible tumors | Potential for complete cure |
| Chemotherapy | Tumors not amenable to surgery | Control tumor growth |
| Targeted Therapy | Specific molecular targets | Precision treatment with fewer side effects |
“The management of pilocytic astrocytoma requires a multidisciplinary approach, combining the expertise of neurosurgeons, oncologists, and other healthcare professionals to provide comprehensive care.”
Risk Factors for Pediatric Brain Tumors
While we don’t know the exact causes of pediatric brain tumors, research has found some key risk factors. Knowing these can help in catching and preventing them early.
Genetic Predisposition
Genetics are a big part of why some kids get brain tumors. Certain genetic syndromes, like Li-Fraumeni syndrome and neurofibromatosis, raise the risk. These syndromes have mutations in genes that help stop cancer.
For example, kids with Li-Fraumeni syndrome are more likely to get brain tumors. This is because of a gene called TP53. Neurofibromatosis type 2 also increases the risk of nervous system tumors.
Environmental Factors
Some environmental exposures might also increase the risk of brain tumors in kids. Ionizing radiation is a well-known risk. Kids who get radiation for other cancers are more likely to get brain tumors later.
Other possible risks include pesticides, electromagnetic fields, and certain chemicals. But, the evidence for these is not as clear. More research is needed to understand their role.
It’s vital to keep studying both genetic and environmental risks. This research can help us find ways to prevent and treat pediatric brain tumors. It can also improve the lives of kids with these tumors.
Recognizing the Symptoms of Childhood Brain Tumors
Brain tumors in kids can be hard to spot because their symptoms are often mild. It’s very important for parents and caregivers to watch closely. Catching these symptoms early can help a lot.
General Symptoms
Brain tumors in kids can cause a variety of symptoms. These symptoms are not specific to where the tumor is. They include:
- Headaches
- Nausea and vomiting
- Fatigue
- Changes in appetite
- Irritability
These symptoms can look like other common illnesses in kids. This makes it hard to find brain tumors early.
Location-Specific Symptoms
The symptoms of brain tumors depend on where the tumor is. For example:
| Tumor Location | Possible Symptoms |
| Cerebellum | Coordination and balance problems, difficulty walking |
| Brainstem | Difficulty swallowing, double vision, facial weakness |
| Cerebral Hemispheres | Seizures, weakness or numbness in limbs, vision changes |
Age-Related Presentation Differences
Symptoms of brain tumors can change with a child’s age. Infants might show:
- An enlarged head circumference
- Failure to thrive
- Developmental delays
Older kids can talk about their symptoms more clearly. They might say they have headaches or see things differently.
Knowing how symptoms change with age is key. It helps doctors find and treat brain tumors in kids sooner.
Diagnostic Procedures for Pediatric Brain Tumors
Diagnosing pediatric brain tumors involves several steps. These include imaging, biopsy, and molecular testing.
Imaging Techniques
Imaging is key in diagnosing pediatric brain tumors. We use MRI, CT scans, and PET scans. MRI gives us detailed images of the tumor’s size and location.
MRI is the best tool for brain tumor diagnosis. It shows the tumor’s details and how it relates to other parts of the brain. This is important for planning surgery.
| Imaging Modality | Key Features | Clinical Use |
| MRI | High-resolution images, excellent soft-tissue contrast | Tumor localization, surgical planning |
| CT Scan | Quick, widely available, good for calcifications | Emergency situations, detecting calcifications |
| PET Scan | Metabolic information, useful for tumor grading | Tumor grading, assessing treatment response |
Biopsy and Pathological Examination
A biopsy takes a tissue sample from the tumor. It’s vital for confirming the diagnosis and identifying the tumor type. Our pathologists use advanced methods to make an accurate diagnosis.
“The accurate diagnosis of pediatric brain tumors is critical for choosing the right treatment. Biopsy and pathological examination are essential in this process.”
Molecular and Genetic Testing
Molecular and genetic testing are now key in diagnosing and managing pediatric brain tumors. These tests help find specific genetic changes that affect treatment and prognosis. We use next-generation sequencing (NGS) and methylation profiling for detailed molecular information.
We combine imaging, biopsy, pathological examination, and molecular testing for a complete diagnosis. Our team works together to create a personalized treatment plan for each child. This ensures they get the best care possible.
Staging and Grading Systems for Childhood Brain Tumors
Understanding the staging and grading of childhood brain tumors is key. It helps us choose the best treatment. Accurate staging and grading tell us how serious the tumor is and what treatment is best.
Staging and grading brain tumors is complex. It helps us understand how the tumor behaves. We use different systems to classify tumors based on their features and behavior.
WHO Classification
The World Health Organization (WHO) classification is a common system for brain tumors. It sorts tumors by their look and molecular makeup. This helps us understand how the tumor will behave and its chances of success.
The WHO system gives a grade to the tumor, showing how aggressive it is. Grade I tumors are usually not aggressive and grow slowly. Grade IV tumors are very aggressive and grow fast. This grading is important for knowing the prognosis and making treatment plans.
Risk Stratification
Risk stratification is also important in managing childhood brain tumors. It looks at the tumor’s type, grade, and molecular makeup. It also considers the child’s age and health. This helps us find out who is at high risk of the tumor getting worse or coming back.
By using the WHO classification and risk stratification together, we get a better picture of each child’s situation. This approach helps us give personalized care. It aims to improve treatment results and reduce long-term side effects.
Surgical Intervention
Surgery is often the first step in treating medulloblastoma. Our goal is to remove as much of the tumor as we can. This helps keep the brain tissue safe.
The amount of tumor removed is key. Maximal safe resection means better survival chances and less chance of the tumor coming back.
Radiation Therapy
Radiation therapy is important for medulloblastoma, mainly for those with leftover tumor after surgery. We use craniospinal irradiation to hit the tumor hard but spare the healthy brain and spine.
| Radiation Type | Description | Benefits |
| Craniospinal Irradiation | Targets the entire brain and spinal cord | Effective in treating medulloblastoma that may spread to the central nervous system |
| Focal Radiation | Targets the tumor site specially | Reduces damage to surrounding brain tissue |
Chemotherapy Protocols
Chemotherapy is a big part of treating medulloblastoma. It’s often used with surgery and radiation. Our oncologists make special chemotherapy plans for each patient.
For high-risk patients, high-dose chemotherapy with stem cell rescue is promising. Multi-agent chemotherapy protocols attack the tumor from different sides.
Targeted Therapies
Targeted therapies are a new hope in treating medulloblastoma. They focus on specific ways tumors grow. Our team works together to find and use these therapies.
Understanding medulloblastoma’s molecular makeup helps us make treatments that work better for each patient. This can lead to better results.
Treatment Considerations for Other Pediatric Brain Tumors
Treatment for pediatric brain tumors varies widely. Each tumor needs a special plan for the best care. This ensures the best results for our young patients.
Astrocytoma Treatment
Astrocytomas are common in kids. Treatment depends on the tumor’s grade and where it is. Surgical resection is often the first step. It aims to remove as much of the tumor as possible without harming the brain.
- Low-grade astrocytomas might just need regular check-ups after surgery.
- High-grade astrocytomas might need more treatments like chemotherapy or radiation.
Ependymoma Management
Ependymomas are brain tumors that happen in children. Treatment includes surgery, radiation therapy, and chemotherapy. How much of the tumor is removed is key to the outcome.
- The goal is to remove as much as safely possible.
- After surgery, radiation therapy is often needed to lower the chance of the tumor coming back.
- Chemotherapy might be used if the tumor can’t be fully removed.
Approaches to DIPG
DIPG is a very aggressive and hard-to-treat brain tumor. Radiation therapy is the main treatment, helping to ease symptoms. We’re also looking into new treatments through clinical trials.
- Radiation therapy helps manage symptoms and improve life quality.
- Joining clinical trials might give access to new treatments.
We’re dedicated to giving full care to kids with brain tumors. We make treatment plans that fit each child’s needs.
Medulloblastoma Survival Rate and Prognosis
Knowing the survival rate and prognosis of medulloblastoma is key for patients and their families. It helps them understand the disease better.
Factors Affecting Prognosis
The prognosis for medulloblastoma patients depends on several factors. These include the patient’s age, how much of the tumor was removed, and if the cancer has spread.
Age at Diagnosis: Kids under 3 usually face a tougher prognosis. This is because their brains are not fully developed, limiting treatment options like radiation.
Tumor Resection: How much of the tumor was removed is very important. Removing most or all of it can lead to better outcomes.
Metastasis: If the cancer has spread at diagnosis, the prognosis gets much worse.
Long-term Survival Statistics
Treatment advances have boosted survival rates for medulloblastoma patients. Now, 5-year survival rates range from 70% to over 80% for those with favorable risk factors.
| Risk Category | 5-Year Survival Rate |
| Average Risk | 75% |
| High Risk | 60% |
Quality of Life Considerations
While survival rates have gone up, the quality of life for survivors is a big concern. Long-term effects of treatment, like brain and hormone problems, need careful management.
We aim to provide care that meets both immediate and long-term needs of our patients. We focus on their overall well-being.
Long-term Effects and Survivorship
Medical treatments have improved, focusing on the long-term effects of childhood brain tumors. Long-term survivorship is key for kids with brain tumors. Survivors often face big challenges that affect their quality of life.
Neurocognitive Outcomes
Brain tumors and their treatment can harm a child’s brain function. Survivors might struggle with memory, attention, and speed. Neurocognitive late effects differ based on the tumor, treatment, and age at diagnosis.
We do detailed brain assessments to find out what each survivor can do well. This helps us tailor support to help them reach their goals.
Endocrine and Growth Issues
Survivors of childhood brain tumors often face growth and hormone problems. Growth hormone deficiency is common, causing growth issues or metabolic problems.
Our team offers special endocrine care. We make sure survivors get the right hormone therapy and support for normal growth.
Psychosocial Impact
Being diagnosed and treated for a brain tumor deeply affects kids and their families. Survivors might deal with anxiety, depression, or finding their place in society.
We stress the need for psychosocial support. We offer counseling, support groups, and resources. This helps survivors and their families cope and improve their lives.
Long-term care is vital for childhood brain tumor survivors. By tackling long-term effects early, we can greatly improve their lives. We support them as they grow into adults.
Multidisciplinary Care for Pediatric Brain Tumors
Pediatric brain tumors need a team effort for the best treatment. This team approach makes sure kids get all the care they need.
We know treating pediatric brain tumors is tough. It takes a team of experts working together. “A multidisciplinary approach is essential in providing the best possible care for children with brain tumors,” say top pediatric neuro-oncology experts.
Pediatric Neuro-Oncology Teams
A team for pediatric brain tumors includes neurosurgeons, radiation oncologists, and more. They create treatment plans that fit each child’s needs.
Specialized Pediatric Centers
Special centers for kids with brain tumors are key. They have the latest tech and teams focused on kids’ needs.
These centers help kids get better care and support. They make sure families get the help they need, too. This makes care smoother and more effective.
Transitional Care to Adulthood
As kids with brain tumors grow up, their care changes. Transitional care helps them move from kids’ to adult healthcare.
We focus on keeping care going smoothly as kids grow up. This helps young adults deal with adult healthcare. They get support and care that fits their needs.
Advances in Pediatric Brain Tumor Research
Genomic and molecular research is changing how we fight pediatric brain tumors. It’s opening up new ways to diagnose and treat these cancers. This research is bringing hope to kids with these complex diseases.
Genomic and Molecular Discoveries
Recent studies have uncovered key genetic and molecular details about pediatric brain tumors. Genomic analyses have found specific mutations that help tumors grow. This knowledge helps doctors find better treatments.
Using molecular diagnostics has made diagnosis more accurate. It also helps tailor treatments to each patient. This is key in treating the many types of pediatric brain tumors.
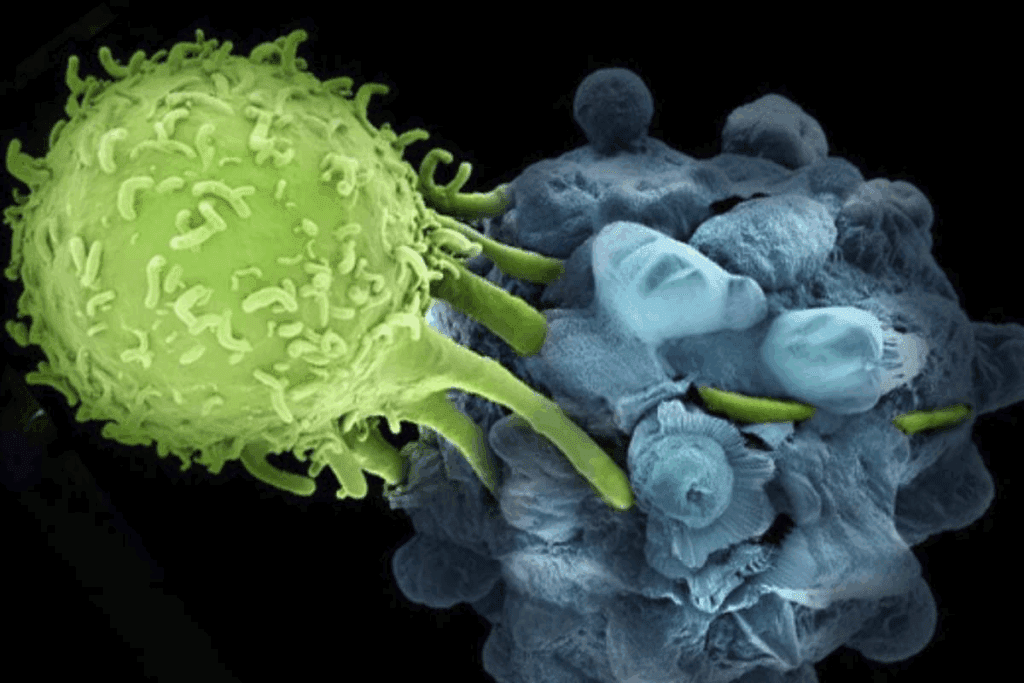
Immunotherapy Approaches
Immunotherapy is a new hope for treating pediatric brain tumors. It uses the body’s immune system to target cancer cells. Immunotherapeutic strategies, like checkpoint inhibitors and CAR-T cell therapy, are being tested in trials.
These new treatments could lead to better survival rates and fewer side effects. As research continues, immunotherapy will likely become a big part of treating these tumors.
Precision Medicine Initiatives
Precision medicine is changing how we treat pediatric brain tumors. It lets doctors find the best treatment by looking at the tumor’s genetics. Precision medicine initiatives help create targeted therapies for each patient’s tumor.
This approach makes treatments more effective and reduces side effects. As we learn more about these tumors, precision medicine will have a bigger impact.
Support Resources for Families
Families dealing with pediatric brain tumors face big challenges. But they’re not alone. Our institution offers a wide range of support to help them through tough times.
National Organizations
National organizations are key in supporting families with pediatric brain tumors. They offer lots of information, emotional support, and help in advocacy. For example, events like the charity horse race in Waregem show the community’s dedication to helping.
Some top national organizations include:
- CureSearch for Children’s Cancer: They give info on childhood cancer, including brain tumors, and support families through various programs.
- The Pediatric Brain Tumor Foundation: They offer resources, support, and funding for research into pediatric brain tumors.
- American Brain Tumor Association (ABTA): They provide educational resources, support services, and advocacy for brain tumor patients and their families.
Hospital-Based Programs
Hospital-based programs are also vital for families. They offer counseling, support groups, and educational resources. These are tailored to meet the needs of families with pediatric brain tumors.
Key parts of these programs include:
- Pediatric Oncology Teams: Teams that give full care, including medical treatment, psychological support, and social services.
- Support Groups: Groups where families can share their experiences, get emotional support, and connect with others facing similar challenges.
- Educational Workshops: Workshops that teach about managing the condition, treatment options, and coping strategies.
Educational Resources
Educational resources are key for families to understand pediatric brain tumors. They help families learn about treatment options and managing the condition. These resources include:
- Informational Brochures: Detailed brochures that give info on various aspects of pediatric brain tumors.
- Online Resources: Websites and online platforms that offer the latest info, research, and support services.
- Workshops and Seminars: Events where experts share the latest on treatments, research, and management strategies.
By using these support resources, families can better handle the challenges of pediatric brain tumors. We’re committed to making these resources available and supporting families every step of the way.
Conclusion
Understanding pediatric brain tumors is key to helping children with these conditions.
We’re committed to giving top-notch care to patients from around the world. We know how important it is to support families from start to finish. This support helps ensure the best care for kids with brain tumors.
As research gets better, we keep working to offer the latest treatments and support. We focus on meeting the needs of each child and their family. Our goal is to make a real difference in their lives.
FAQ
What is medulloblastoma, and how common is it in children?
Medulloblastoma is the most common brain tumor in kids. It starts in the cerebellum and grows fast.
What are the symptoms of a brain tumor in children?
Symptoms depend on the tumor’s location and size. Kids might have headaches, nausea, or balance issues. It’s important to catch these early.
How are pediatric brain tumors diagnosed?
We use MRI, biopsy, and molecular tests to diagnose.
What are the treatment options for medulloblastoma?
Treatment includes surgery, radiation, and chemotherapy. Our team creates a plan that fits each patient’s needs.
What is the prognosis for children diagnosed with medulloblastoma?
Prognosis depends on age, tumor size, and molecular characteristics. New treatments have improved survival rates. We focus on quality of life too.
What are the long-term effects of pediatric brain tumors?
Survivors might face cognitive, endocrine, and growth issues.
Are there any support resources available for families affected by pediatric brain tumors?
Yes, there are national organizations and hospital programs to help. We provide support to our patients and their families.
What advances are being made in pediatric brain tumor research?
Research focuses on genomics, immunotherapy, and precision medicine. These advances aim to create better treatments and improve outcomes.
How are pediatric brain tumors classified?
Tumors are classified by the World Health Organization (WHO) system. This system looks at histology, molecular characteristics, and grade. Accurate classification helps choose the best treatment.
What is the difference between astrocytoma and ependymoma?
Astrocytoma and ependymoma are different brain tumors. Astrocytomas come from astrocytes, while ependymomas come from ependymal cells. Each has its own treatment options.
References
- Xu, T., & Li, D. (2025). Global research trends in liver regeneration and immunomodulation: A perspective from bibliometric analysis. Frontiers in Immunology. https://pmc.ncbi.nlm.nih.gov/articles/PMC12218472/