
Nearly 1.8 million new cancer cases are diagnosed in the United States each year. A big part of these are solid tumors. The causes of solid tumors are complex, involving both genetic and environmental factors.
Recent studies have found that genetic mutation triggers and the cellular transformation process are key in solid tumor formation. Knowing how these work is key to finding better ways to prevent and treat cancer.
We aim to give a detailed look at solid tumor causation factors. This helps those looking for top-notch medical care and support.
Key Takeaways
- Genetic and environmental factors contribute to the development of solid tumors.
- Understanding genetic mutation triggers is key for prevention.
- The cellular transformation process is a key element in tumor formation.
- Effective prevention and treatment strategies rely on understanding these causes.
- Comprehensive care for cancer patients involves addressing these underlying factors.
Understanding Solid Tumors: Definition and Classification

It’s key to know about solid tumors to fight this serious disease. Solid tumors are abnormal tissue masses that can be benign or malignant. They grow out of control, causing health problems based on where they are and what they are.
Distinguishing Solid Tumors from Other Cancer Types
Solid tumors are different from liquid tumors like leukemia. Liquid tumors affect the blood and bone marrow. Solid tumors, on the other hand, form masses that can be felt or seen on scans. This difference is important for diagnosis and treatment.
Key characteristics of solid tumors include:
- Abnormal cell growth leading to tumor formation
- Potential to be benign or malignant
- Varied tissue origins, influencing treatment approaches
Common Types of Solid Tumors
Solid tumors are grouped by where they start and how they look under a microscope. The main types are:
Carcinomas, which start in epithelial cells, are the most common. Examples are breast, lung, and colon cancers. Sarcomasstart in connective or muscular tissues. Gliomas, from the brain’s glial cells, are another big group.
“The classification of solid tumors is not just a matter of academic interest; it has direct implications for patient care and treatment outcomes.”
Knowing about these solid tumor types and their features is critical. It helps in creating targeted treatments and better patient results.
The Cellular Transformation Process
It’s key to grasp the cellular transformation process for better cancer prevention and treatment. This process happens when normal cells get genetic mutations. These mutations mess up how cells work normally.
Normal Cell Growth vs. Cancerous Growth
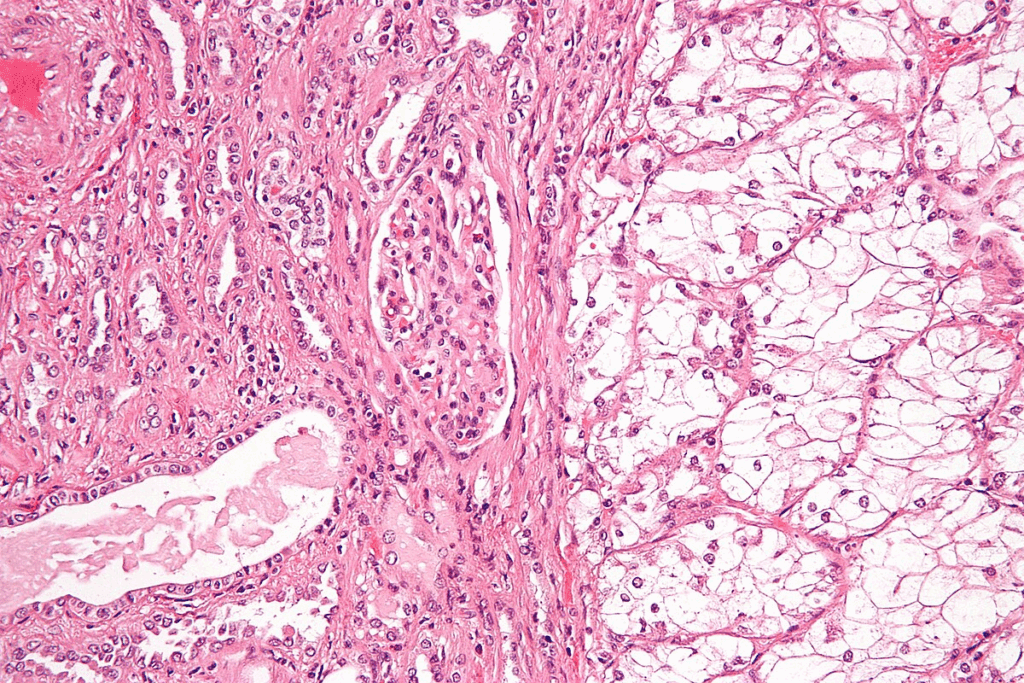
Normal cell growth is tightly controlled. It ensures cells divide, grow, and die properly. But, cancerous growth is out of control. It leads to cells growing too much, losing their shape, and not dying when they should.
Genetic mutations are the main difference between normal and cancerous growth. These mutations can come from many sources. This includes harmful substances in the environment, genetic traits, and viruses.
Stages of Cellular Transformation
The transformation of cells goes through several stages:
- Initiation: This is the start where genetic changes happen due to different causes.
- Promotion: Here, these changes get stronger, leading to pre-cancerous growths.
- Progression: The last stage where these growths turn into invasive cancer.
Knowing these stages helps us find ways to stop or treat cancer more effectively.
Genetic Mutations as Primary Triggers
Genetic mutations play a big role in solid tumors. They affect oncogenes, tumor suppressor genes, and DNA repair genes. These changes can lead to uncontrolled cell growth, which is a hallmark of cancer.
Oncogenes and Their Activation
Oncogenes are genes that can lead to cancer if they mutate or are overactive. They help cells grow and divide. But, when they mutate, they can make cells grow too much.
There are many ways oncogenes can become active. For example, the KRAS gene is often mutated in cancers. This makes a protein that helps tumors grow.
Tumor Suppressor Gene Inactivation
Tumor suppressor genes keep cells in check. They help fix DNA and make cells die if they’re too damaged. When these genes are turned off, cells can keep growing and spreading.
Numerous cancers exhibit mutations in genes such as TP53. Without TP53, cells can’t die when they should. This helps tumors grow.
DNA Repair Gene Dysfunction
DNA repair genes fix DNA damage. If these genes don’t work right, cells can get more mutations. This raises the chance of getting cancer.
For instance, BRCA1 and BRCA2 help fix DNA breaks. But, if they’re mutated, it raises the risk of breast and ovarian cancers. People with these mutations need to be watched closely.
Hereditary Factors in Tumor Development
The study of hereditary factors in tumor development is complex and important. We’re learning how genetics can make some people more likely to get cancer.
Inherited Cancer Syndromes
Some genetic syndromes raise the risk of certain cancers. For example, BRCA1 and BRCA2 mutations increase the risk of breast and ovarian cancers. Knowing about these syndromes helps with early detection and prevention.
- BRCA1 and BRCA2 mutations are linked to higher risks of breast and ovarian cancers.
- Lynch syndrome raises the risk of colorectal, endometrial, and other cancers.
- Familial adenomatous polyposis (FAP) leads to many polyps in the colon, increasing colorectal cancer risk.
Family History and Cancer Risk Assessment
A family history of cancer is a big risk factor for tumors. We check this risk by looking at how many relatives have cancer, their age at diagnosis, and genetic syndromes.
- Collect detailed family history to spot cancer patterns.
- Look at the age of diagnosis for first-degree relatives (parents, siblings, children).
- Consider genetic testing for known cancer-causing mutations if there’s a strong family history.
By understanding hereditary factors and family history, we can spot those at higher risk. This helps us take steps to prevent cancer.
Solid Tumor Causation Factors: A Comprehensive Overview
Solid tumors grow due to many genetic, environmental, and lifestyle factors. Knowing these factors and how they work together is key to fighting cancer.
Multifactorial Nature of Cancer Development
Cancer doesn’t come from one thing; it’s many factors working together. Genetic predispositions are a big part, with some genes making certain cancers more likely.
Things we’re exposed to, like carcinogenic chemicals and radiation, also raise cancer risk. Our choices, like tobacco use, diet, and physical activity levels, play a role too.
Interaction Between Different Causative Agents
When different causes work together, the risk of cancer can grow. For example, if you have a genetic risk and are exposed to harmful substances, your risk goes up a lot.
“The interplay between genetic, environmental, and lifestyle factors in cancer development highlights the need for a complete approach to fighting cancer.”
Getting how these factors interact helps us find who’s at highest risk. This way, we can make better plans to lower cancer rates and help patients more.
Environmental Carcinogens and Exposure Risks
Environmental carcinogens are key in causing many cancers. It’s vital to know how they affect us. We face many environmental carcinogens every day, often without realizing it. These come from air and water pollution, industrial activities, and some products we use.
Chemical Carcinogens in the Environment
Chemical carcinogens are substances that can lead to cancer. They are in many pollutants, like:
- Polycyclic aromatic hydrocarbons (PAHs) from car exhaust and factories
- Volatile organic compounds (VOCs) in cleaning products and paints
- Pesticides and herbicides in farming
These chemicals can pollute air, water, and soil. This leads to widespread exposure. It’s important to cut down on these substances to prevent cancer.
Radiation Exposure
Radiation is a big environmental carcinogen. There are two kinds: ionizing and non-ionizing radiation.
- Ionizing radiation, like X-rays and radon, can damage DNA and cause cancer.
- Non-ionizing radiation, such as UV from the sun or tanning beds, can also harm DNA and raise cancer risk.
By using sunscreen and following safety rules during medical tests, we can lower our cancer risk.
Industrial and Occupational Hazards
Some jobs expose workers to specific carcinogens, raising their cancer risk. For example:
- Asbestos in construction and mining
- Benzene in the petrochemical industry
- Formaldehyde in manufacturing and funeral homes
By enforcing strict safety rules and giving protective gear, we can lower cancer risk in these jobs.
In summary, environmental carcinogens are a big health risk. Knowing where these carcinogens come from and how to avoid them is key to preventing cancer. By tackling these risks together, we can make a big difference in cancer prevention.
Viral and Bacterial Infections Leading to Cancer
Some infections caused by viruses and bacteria can increase the risk of cancer. We will look at how these microorganisms lead to cancer. We will also talk about how to prevent or treat these infections.
Human Papillomavirus (HPV) and Cancer
Human Papillomavirus (HPV) is a major cause of several cancers. This includes cervical cancer and other cancers in the genital and throat areas. HPV is the most common sexually transmitted infection worldwide. While many infections go away on their own, some can lead to cancer if they don’t clear up.
To prevent HPV, vaccines are available and very effective. Screening for cervical and other HPV-related cancers is also important. This helps find and treat cancer early.
Hepatitis Viruses and Liver Cancer
Hepatitis B and C viruses (HBV and HCV) are big risks for liver cancer. Chronic infection can cause liver cirrhosis and cancer. Vaccination for HBV is key to prevention. Treatment for HCV has improved a lot with new medicines.
Preventing and treating hepatitis virus infections is vital to lower liver cancer rates. Public health efforts include vaccines, blood donation screening, and safe injection education.
Helicobacter pylori and Gastric Cancer
Helicobacter pylori (H. pylori) infection raises the risk of gastric cancer. This bacterium causes chronic gastritis, which can lead to cancer. Getting rid of H. pylori with antibiotics can lower gastric cancer risk. This is true, even for those with a family history of the disease.
| Infection | Cancer Type | Prevention/Treatment |
| HPV | Cervical, Anogenital, Oropharyngeal | Vaccination, Screening |
| HBV/HCV | Liver Cancer | Vaccination (HBV), Antiviral Treatment |
| H. pylori | Gastric Cancer | Antibiotic Eradication |
It’s important to understand the link between infections and cancer. This knowledge helps us develop better ways to prevent and treat cancer. By tackling these infections, we can greatly reduce cancer’s impact worldwide.
Chronic Inflammation and Its Impact on Tumor Formation
Chronic inflammation is when the immune system stays active for too long. It plays a big role in cancer growth. We will look at how it helps tumors form.
Inflammatory Pathways in Cancer Development
The inflammatory process has complex pathways. When these pathways go wrong, they can lead to cancer. Key players include cytokines, chemokines, and immune cells.
These molecules and cells create an environment that helps tumors grow. For example, chronic inflammation can cause the body to make reactive oxygen species (ROS). ROS can damage DNA and cause genetic mutations.
Chronic Diseases Associated with Increased Cancer Risk
Some chronic diseases raise the risk of getting cancer. For example, ulcerative colitis and Crohn’s disease increase the risk of colorectal cancer.
Chronic pancreatitis also raises the risk of pancreatic cancer. Knowing these links helps us spot people at higher risk. We can then take steps to watch them more closely.
| Chronic Disease | Associated Cancer Risk |
| Ulcerative Colitis | Colorectal Cancer |
| Crohn’s Disease | Colorectal Cancer |
| Chronic Pancreatitis | Pancreatic Cancer |
| Chronic Hepatitis B/C | Liver Cancer |
Lifestyle Factors Contributing to Cancer Risk
Our daily habits and lifestyle choices greatly affect our chance of getting cancer. Things like tobacco use, alcohol, diet, and exercise play big roles in cancer risk. Knowing and changing these factors can lower our cancer risk.
Tobacco Use and Smoking
Tobacco is the top cause of preventable cancer deaths globally. Smoking links to lung, throat, and mouth cancers. Smokers face a much higher risk than non-smokers. Quitting can greatly lower this risk.
“Tobacco use is a major public health threat, and quitting is key for cancer prevention.”
Good smoking cessation programs and laws are vital to cut down tobacco-related cancer.
Alcohol Consumption
Drinking too much alcohol also raises cancer risk. Heavy drinking is linked to liver, breast, and esophageal cancers. Cutting down on alcohol can lower this risk.
- Limiting alcohol intake can help reduce cancer risk.
- Avoiding binge drinking is key.
- Moderate drinking, up to one drink a day for women and two for men, is safer.
Diet and Nutrition
Eating well, with lots of fruits, veggies, and whole grains, can lower cancer risk. Some diets, like the Mediterranean one, are linked to lower cancer risks. But, diets heavy in processed and red meat may raise risks.
| Dietary Component | Cancer Risk Association |
| Fruits and Vegetables | Reduced risk |
| Whole Grains | Reduced risk |
| Processed and Red Meat | Increased risk |
Physical Inactivity and Obesity
Not moving enough and being overweight also raise cancer risks, like in breast, colon, and kidney cancers. Regular exercise and a healthy weight are key to preventing cancer.
Doing regular activities like walking, cycling, or swimming can lower cancer risk. Also, keeping a healthy weight through diet and exercise is very important.
Epigenetic Modifications in Cancer Development
Epigenetic changes are key to understanding cancer. These changes affect how genes work without changing the DNA. They play a big role in cell growth and development. But, when they go wrong, they can lead to cancer.
DNA Methylation Patterns
DNA methylation is a major epigenetic change. It adds a methyl group to DNA, which can turn off genes. In cancer, this process goes awry, silencing genes that should stop tumors.
“The wrong methylation of DNA is a sign of cancer,” says recent research. It helps tumors grow by turning off important genes.
Histone Modifications
Histone modifications are vital for controlling gene expression. Histones are proteins that DNA wraps around. Changes to these proteins can affect how genes are turned on or off.
For example, histone H3K27me3 is linked to gene silencing in cancer cells. This shows how histone changes can lead to cancer.
Non-coding RNAs in Cancer
Non-coding RNAs, like miRNAs and lncRNAs, are important in gene regulation. In cancer, their levels often change. Some miRNAs can fight cancer by targeting genes that promote tumor growth.
On the other hand, some lncRNAs can help cancer grow. Studying these RNAs can help find new treatments.
Molecular Signaling Pathway Disruptions
Molecular signaling pathways play a big role in cancer. They control how cells grow, divide, and survive. When these pathways get disrupted, cells can grow out of control and form tumors.
We will look at three main areas where these disruptions happen. These are growth factor signaling problems, cell cycle checkpoint failures, and apoptosis resistance.
Growth Factor Signaling Abnormalities
Growth factor signaling pathways help control cell growth and division. When these pathways don’t work right, it can cause overactive signaling. This can lead to cells growing too much.
For example, mutations in genes for growth factor receptors can make them work too much. This can help tumors grow.
“The dysregulation of growth factor signaling pathways is a hallmark of many cancers, making them good targets for treatment.”
Cell Cycle Checkpoint Failures
Cell cycle checkpoints are important for making sure cells divide correctly. If these checkpoints fail, it can cause uncontrolled cell division. This lets damaged cells keep growing.
Many cancers have mutations in genes that control these checkpoints. One common mutation is in the TP53 gene.
- Without working checkpoints, damaged DNA can be copied.
- This leads to unstable DNA, which makes cancer worse.
- Such instability can make cancer cells more aggressive.
Apoptosis Resistance Mechanisms
Apoptosis, or programmed cell death, is key for getting rid of damaged cells. Cancer cells often resist apoptosis, letting them live even with a lot of DNA damage. Changes in the BCL-2 family of proteins and inhibition of caspase activityare some ways cancer cells resist apoptosis.
Understanding these disruptions is key to finding better cancer treatments. By focusing on the specific problems that make tumors grow, we can make treatments more effective and tailored to each patient.
Tumor Microenvironment and Its Role
The tumor microenvironment is complex and drives cancer growth. It includes non-cancerous cells like stromal cells, blood vessels, and immune cells. These cells work with cancer cells to help the tumor grow.
Stromal Cells and Cancer Progression
Stromal cells, like cancer-associated fibroblasts, are key in cancer growth. They release growth factors and proteins that help tumors grow. These cells also help tumors spread by changing the tissue around them.
Angiogenesis in Tumor Growth
Angiogenesis is vital for tumor growth and spreading. Tumors make new blood vessels by releasing factors like VEGF. This ensures they get the oxygen and nutrients they need.
| Pro-angiogenic Factors | Role in Tumor Growth |
| VEGF | Stimulates endothelial cell proliferation and migration |
| Angiopoietin-2 | Regulates vascular destabilization and remodeling |
| PDGF | Promotes pericyte recruitment and vessel stabilization |
Immune System Evasion
Tumors find ways to avoid the immune system. They use molecules like PD-L1 to stop T-cells from attacking. Knowing how they do this helps us create better treatments.
Looking at the tumor microenvironment helps us understand cancer better. We aim to provide care that meets the complex needs of cancer patients.
Age as a Risk Factor for Solid Tumors
As we get older, the chance of getting solid tumors goes up. This is because our cells get damaged over time. Our cells change in ways that can lead to cancer.
Cellular Aging Processes
Cellular aging is a complex process that affects how cells work and repair themselves. As we age, cells can get genetic and epigenetic changes. These changes can cause cancer.
- Telomere shortening: Telomeres protect the ends of chromosomes. As we age, telomeres shorten, potentially leading to genetic instability.
- Epigenetic changes: Aging cells often exhibit changes in DNA methylation and histone modification, affecting gene expression.
- Accumulation of DNA damage: Cells are constantly exposed to DNA-damaging agents. With age, the ability to repair this damage can decline.
Cumulative Exposure to Carcinogens
As people age, they are more likely to have been exposed to various environmental carcinogens. This includes UV radiation, tobacco smoke, and industrial chemicals. This exposure can raise the risk of solid tumors.
Key factors include:
- Lifetime exposure to UV radiation, increasing the risk of skin cancers.
- Prolonged exposure to tobacco smoke, a major risk factor for lung and other cancers.
- Occupational exposure to carcinogenic chemicals, which can lead to various types of cancer.
Age-related Immune System Changes
Aging affects the immune system, known as immunosenescence. This can make it harder for the body to fight off cancer cells. This can lead to tumor growth.
Immunosenescence involves:
- Reduced function of immune cells, such as T cells and macrophages.
- Altered cytokine production, affecting immune responses.
- Increased inflammation, which can promote tumor development.
Understanding how age affects the risk of solid tumors is key. It helps in creating prevention and treatment plans. By tackling these factors, we can lower the risk of solid tumors in older people.
Emerging Research on Tumor Causation
New studies are showing us how different parts of our lives can lead to tumors. Our lifestyle, environment, and body’s inner workings all play a role. This is changing how we see cancer.
Gut Microbiome Influence
The trillions of microbes in our gut are key to our health, including fighting cancer. An imbalance in these microbes, or dysbiosis, can cause chronic inflammation. This inflammation might help tumors grow. The ways microbes affect cancer risk are complex, involving many body systems.
Some microbes make substances that help or hurt tumors. For example, some produce anti-inflammatory acids, while others make substances that can lead to cancer. The mix of these microbes and their activities is important for cancer risk.
Circadian Rhythm Disruption
Our modern lives often disrupt our natural body clock. This can increase cancer risk. Our body’s clock controls many functions, and disrupting it can cause problems like metabolic issues and weakened immune systems.
Circadian disruption might affect hormone levels, cell cycles, and how our body fixes DNA damage. For instance, melatonin, made at night, helps fight cancer. Light at night can lower melatonin levels, raising cancer risk.
Psychological Stress and Cancer
Stress and cancer have a long history of research. Long-term stress can weaken our immune system. This can make our body more welcoming to tumors.
While the exact link is not fully understood, stress clearly affects our body in ways that can influence cancer. More research is needed to grasp how stress, immunity, and tumors interact.
Conclusion: The Complex Web of Solid Tumor Causation
We’ve looked into how solid tumors are caused. It’s a mix of genetics, environment, and lifestyle. Knowing this helps us find better ways to prevent and treat cancer.
Genetics and the environment both play big roles. Genetic changes, family history, and harmful substances can start and grow cancer. Understanding how these factors work together is key to knowing why solid tumors happen.
Seeing how genetics, environment, and lifestyle are connected helps us get cancer treatment right. This knowledge lets us create better plans to fight cancer and improve treatment results.
FAQ
What are the primary causes of solid tumors?
Solid tumors come from a mix of genetic, environmental, and lifestyle factors. These include genetic mutations, exposure to harmful substances, viral and bacterial infections, and chronic inflammation.
How do genetic mutations contribute to cancer development?
Genetic mutations can turn on genes that promote cancer and turn off genes that stop it. They can also mess up DNA repair, leading to uncontrolled cell growth and cancer.
What is the role of environmental carcinogens in cancer risk?
Environmental carcinogens, like chemicals and radiation, can damage DNA and disrupt cell processes. This increases cancer risk.
How do viral and bacterial infections contribute to cancer development?
Viruses like HPV and bacteria like Helicobacter pylori can cause cancer. They disrupt cell processes and lead to chronic inflammation.
What lifestyle factors contribute to cancer risk?
Lifestyle choices like smoking, drinking too much alcohol, and being inactive can raise cancer risk. So can a bad diet and being overweight.
How does chronic inflammation impact tumor formation?
Chronic inflammation can help tumors grow by creating a supportive environment for cancer cells.
What is the role of epigenetic modifications in cancer development?
Epigenetic changes, like DNA methylation, can affect gene expression. This can lead to cancer by promoting cell growth.
How do molecular signaling pathway disruptions contribute to cancer?
Problems in molecular pathways, like growth factor signaling, can help cancer cells grow and survive.
What is the role of the tumor microenvironment in cancer progression?
The tumor microenvironment, including cells and blood vessels, supports cancer growth. It helps cancer cells evade the immune system.
How does age affect the risk of solid tumors?
Age increases the risk of solid tumors. This is due to cellular aging, exposure to carcinogens, and immune system changes.
What are some emerging research areas in tumor causation?
New research looks into the gut microbiome, disrupted circadian rhythms, and psychological stress. These areas may shed light on solid tumor causes.
Can understanding the causes of solid tumors lead to better prevention and treatment strategies?
Yes, knowing the causes of solid tumors can help create better prevention and treatment plans. It’s about understanding the complex factors involved.
References:
- Sierra, M. S., & de Sanjosé, S. (2014). The burden of infection-associated cancers in the Americas. Cancer Epidemiology, 38(6), 659-665. Retrieved from https://www.sciencedirect.com/science/article/pii/S1877782114002252




































