Getting a cancer diagnosis can change your life. It’s important to know about cancer therapy options. Solid tumors are abnormal tissue masses, which can be either benign or malignant. They need a detailed approach to tumor management.
Effective oncology treatment uses different methods. Our treatment plans are made for each tumor’s type, stage, and location. Thanks to new medical tech, patients have many treatment choices now.
Key Takeaways
- Knowing the tumor’s type and stage is key to picking the right treatment.
- Treatment choices depend on the tumor’s features and the patient’s health.
- Good tumor management needs a team effort and a detailed plan.
- Oncology treatment has grown a lot, giving hope to people all over.
- Customized treatment plans are crucial for maximizing outcomes in cancer care.
Understanding Solid Tumors
To tackle solid tumors, we must first understand what they are. They are abnormal tissue masses that can grow in different parts of the body. These include epithelial, connective, and muscle tissue.
Definition and Classification of Solid Tumors
Solid tumors are defined by where they come from and their tissue type. The classification of these tumors is based on the cell type. For example, carcinomas start from epithelial cells, which line organs and glands. Sarcomas come from connective or muscle tissue.
Understanding the grade and stage of solid tumors is also key. The grade shows how much the tumor cells look like normal cells. The stage tells us how far the tumor has spread. This info helps doctors predict outcomes and choose the best treatment.
How Solid Tumors Differ from Other Cancers
Solid tumors are different from liquid tumors like leukemias, which affect the blood. Solid tumors form a mass that can be seen with imaging like X-rays or CT scans.
Treatment for solid tumors varies based on their location, size, grade, and stage. Knowing these differences helps doctors create treatments that fit each tumor’s unique needs.
By understanding solid tumors, healthcare professionals can improve cancer treatment. This leads to better outcomes for patients.
The Multidisciplinary Approach to Solid Tumor Treatment
Managing solid tumors is complex and benefits from a team effort. It takes the work of surgeons, medical oncologists, and radiation oncologists, among others. Their collaboration is key to effective treatment.
The Role of Oncology Teams
Oncology teams are vital in treating solid tumors. They consist of many healthcare professionals working together. They ensure all aspects of a patient’s care are covered, from start to finish.
Each team member brings their expertise to the table. Surgeons help decide if surgery is an option. Medical oncologists advise on chemotherapy and other treatments.
Importance of Integrated Care
Integrated care is essential for treating solid tumors. It combines the services of different healthcare professionals. This approach leads to better disease management and patient outcomes.
Integrated care also makes the patient’s journey smoother. It includes support services like nutrition and psychological support, along with medical treatment.
Treatment Decision-Making Process
The process of deciding on treatment for solid tumors involves teamwork. This teamwork ensures treatment plans fit each patient’s needs.
The team discusses all treatment options with the patient and their family. They consider the tumor type, stage, patient health, and personal preferences. This helps create a treatment plan that works best for each patient.
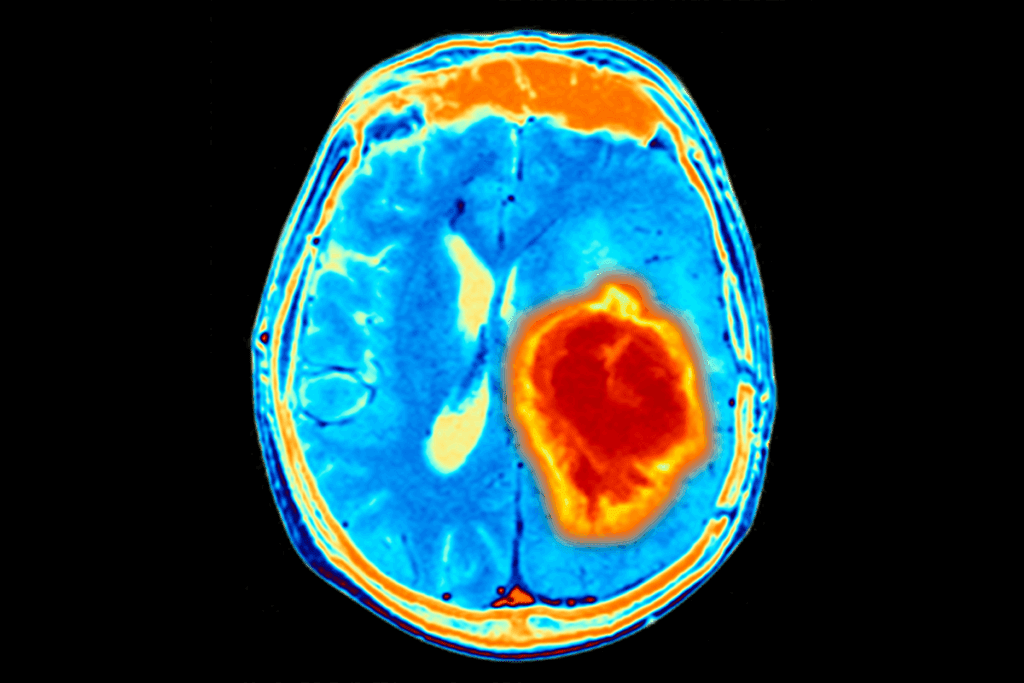
Diagnosis and Staging of Solid Tumors
Accurate diagnosis and staging of solid tumors are key to finding the right treatment. This helps improve patient outcomes. We use many diagnostic techniques to understand the tumor’s nature and size.
Diagnostic Techniques and Procedures
Several methods are used to diagnose and stage solid tumors. These include:
- Imaging Tests: CT scans, MRI, and PET scans show the tumor’s size, location, and spread.
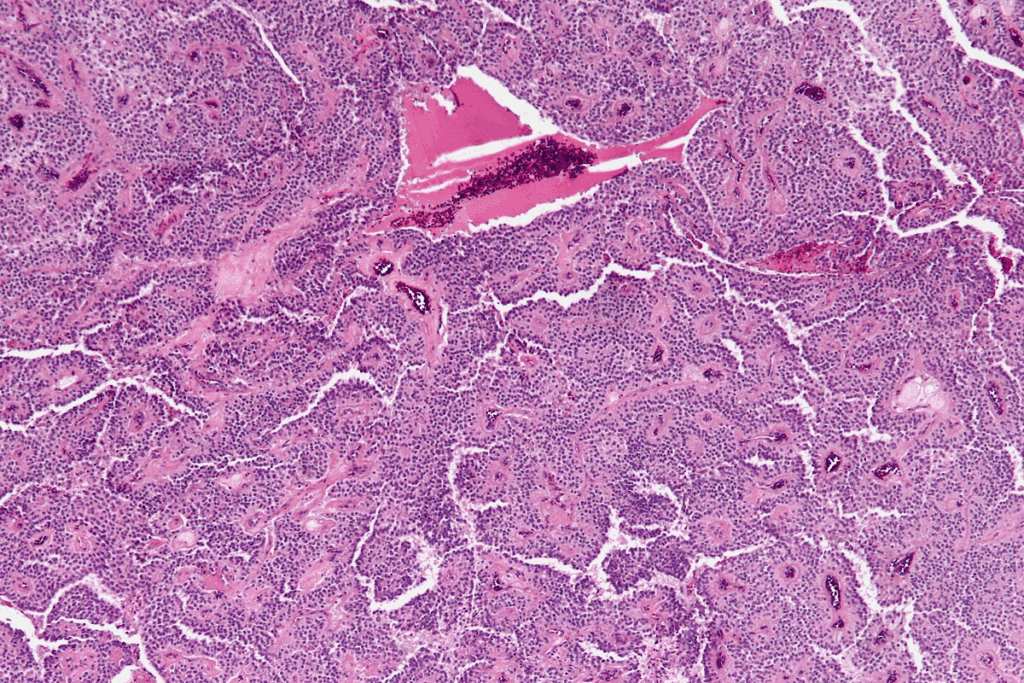
- Biopsy: A biopsy takes a tumor sample for pathological examination to determine its type and grade.
- Laboratory Tests: Blood tests and other tests provide information on the tumor’s presence and markers.
“The integration of imaging and biopsy results is key for accurate staging and effective treatment planning.”
Understanding Tumor Staging and Grading
Tumor staging shows how far the tumor has spread. Grading evaluates the tumor cells’ appearance under a microscope. Both are vital for understanding the prognosis and guiding treatment.
| Stage | Description |
| I | Tumor is localized, no spread |
| II | Tumor is larger, possible spread to nearby lymph nodes |
| III | Tumor has spread to lymph nodes or other nearby tissues |
| IV | Tumor has metastasized to distant parts of the body |
How Staging Influences Treatment Choices
The tumor’s stage greatly affects treatment choices. Early-stage tumors might be treated with surgery or localized radiation therapy. Advanced-stage tumors may need a mix of treatments, including chemotherapy, targeted therapy, or immunotherapy.
We look at several factors to choose the best treatment. These include the tumor’s stage, grade, and the patient’s overall health. This helps us create a personalized treatment plan for the best outcome.
Surgical Removal of Solid Tumors
Surgery is key in treating solid tumors. It offers a chance for a cure or to improve symptoms. For many, removing the tumor is the main treatment.
Types of Cancer Surgery
Cancer surgery is divided by purpose and extent. Curative surgery aims to remove the whole tumor. It’s the main treatment for cancers that haven’t spread.
Palliative surgery aims to ease symptoms and improve life quality for advanced cancers. We also have diagnostic surgery for biopsies to confirm cancer. Debulking surgery makes tumors smaller, helping other treatments work better.
Minimally Invasive Surgical Techniques
Minimally invasive surgery has changed cancer treatment. It cuts down recovery time and scarring. Laparoscopy and robot-assisted surgery use small incisions for precise tumor removal.
- Laparoscopy uses a laparoscope for surgery through small incisions in the abdomen.
- Robot-assisted surgery improves precision and flexibility for complex procedures.
Recovery and Outcomes After Tumor Surgery
Recovery from cancer surgery depends on the surgery type and extent. Post-operative care is vital for pain management, infection prevention, and smooth recovery. Patients are advised on post-surgery rehabilitation to regain strength and mobility.
Outcomes after surgery depend on several factors. These include cancer stage, tumor removal success, and patient health. Follow-up care is key to watch for recurrence and manage surgery effects.
Radiation Therapy for Solid Tumors
Solid tumors often need radiation therapy to kill cancer cells and shrink tumors. This treatment uses high-energy beams. It targets cancer cells precisely, protecting healthy tissue nearby.
External Beam Radiation
External beam radiation therapy (EBRT) uses beams from outside the body. EBRT is highly effective for solid tumors. It targets the tumor site with precision.
We use advanced technology to control the radiation dose. This ensures cancer cells get the most impact while healthy cells are protected.
Internal Radiation (Brachytherapy)
Brachytherapy places radioactive material inside or near the tumor. It delivers a high dose of radiation right to the tumor. This reduces the risk to surrounding tissues.
It’s very effective for some solid tumors, like prostate cancer.
Managing Side Effects of Radiation
Radiation therapy can cause side effects like fatigue and skin irritation. We help patients manage these by using medication and lifestyle changes. Our goal is to reduce discomfort and ensure the best outcome.
Understanding radiation therapy helps patients make informed choices. Our team provides full care, supporting patients through their treatment.
Chemotherapy in Solid Tumor Treatment
Solid tumor treatment often involves chemotherapy. This treatment uses powerful drugs to target cancer cells in the body. Chemotherapy is a systemic treatment, reaching cancer cells that may have spread beyond the original tumor site.
How Chemotherapy Works Against Solid Tumors
Chemotherapy uses drugs that stop cancer cells from growing, dividing, and spreading. These drugs can be taken by mouth or given through an IV, depending on the treatment plan. The goal of chemotherapy is to shrink tumors, slow their growth, or destroy cancer cells that may have spread to other parts of the body.
Chemotherapy can be used in several ways:
- As a primary treatment to shrink tumors before surgery or radiation therapy.
- In conjunction with other treatments, such as surgery or radiation therapy, to enhance their effectiveness.
- To control symptoms and improve quality of life in cases where the cancer is advanced.
Common Chemotherapy Regimens
The choice of chemotherapy regimen depends on several factors. These include the type and stage of the cancer, as well as the patient’s overall health. Common chemotherapy drugs used for solid tumors include doxorubicin, cisplatin, and paclitaxel. These drugs can be used alone or in combination to create a regimen tailored to the individual patient’s needs.
Some common chemotherapy regimens for solid tumors include:
- AC (doxorubicin and cyclophosphamide) for breast cancer.
- PE (cisplatin and etoposide) for lung cancer and other tumor types.
- TP (paclitaxel and carboplatin) for ovarian cancer and other gynecologic malignancies.
Side Effect Management Strategies
While chemotherapy is effective against solid tumors, it can cause significant side effects. Managing these side effects is key to maintaining the patient’s quality of life and ensuring they can continue with their treatment as planned.
Common side effects of chemotherapy include:
- Nausea and vomiting.
- Hair loss.
- Fatigue.
- Increased risk of infection.
To manage these side effects, healthcare providers may recommend:
- Medications to prevent nausea and vomiting.
- Scalp cooling devices to reduce hair loss.
- Rest and relaxation techniques to combat fatigue.
- Prophylactic antibiotics to reduce the risk of infection.
Targeted Therapy for Solid Tumors
Targeted therapy is a big step forward in treating solid tumors. It gives hope to patients with certain molecular profiles. This method targets cancer cells’ unique traits, leading to more precise treatments with fewer side effects.
Customized treatment plans are crucial for maximizing outcomes in cancer care.
Molecular targets are genes or proteins that help cancer cells grow and survive. By finding these targets, we can make therapies that block their action. This stops tumors from growing. Common targets include:
- Proteins that promote cell division
- Genes that are mutated in cancer cells
- Pathways involved in angiogenesis (the formation of new blood vessels)
Knowing these targets is key to making effective targeted therapies.
Types of Targeted Medications
There are many types of targeted medications for solid tumors. These include:
| Type of Medication | Mechanism of Action | Examples |
| Monoclonal Antibodies | Bind to specific proteins on cancer cells, marking them for destruction | Trastuzumab, Bevacizumab |
| Tyrosine Kinase Inhibitors | Block signals that promote cell division and growth | Imatinib, Erlotinib |
| Proteasome Inhibitors | Interfere with protein degradation, leading to cell death | Bortezomib |
These drugs can be used alone or with other treatments to improve results.
Effectiveness and Limitations
Targeted therapy has shown great promise in treating solid tumors. It works by targeting cancer cells more precisely, which reduces harm to normal cells. But, there are challenges, including:
- Resistance to targeted therapies can develop over time
- Not all patients have tumors with identifiable molecular targets
- Side effects can occur, but they are often less severe than with traditional chemotherapy
Despite these hurdles, targeted therapy keeps improving, providing new options for patients with solid tumors.
Immunotherapy: Harnessing the Immune System
Immunotherapy is a new way to fight cancer by using the body’s immune system. It helps the body fight solid tumors better. This method has shown great promise in treating different cancers.
We’re entering a new era in cancer treatment. The focus is on making the immune system stronger to fight cancer cells. Immunotherapy includes checkpoint inhibitors, CAR T-cell therapy, and cancer vaccines. Each targets a different part of the immune response.
Checkpoint Inhibitors
Checkpoint inhibitors are drugs that let the immune system attack cancer cells better. They block proteins on immune cells that normally stop them from attacking healthy cells. This lets the immune system fight cancer cells more effectively.
These drugs have been very effective in treating solid tumors like melanoma, lung cancer, and kidney cancer. They help the immune system destroy cancer cells more efficiently.
CAR T-Cell Therapy
CAR T-cell therapy changes a patient’s T cells to fight cancer. It takes T cells from the blood, changes them to target cancer cells, and then puts them back in the body. This treatment has been very successful in blood cancers.
Researchers are also looking into using it for solid tumors. But, it can cause severe side effects, like cytokine release syndrome.
Cancer Vaccines
Cancer vaccines help the immune system fight cancer cells. They can be made from tumor cells or proteins from cancer cells. These vaccines aim to start an immune response against cancer.
While they’re in the early stages, cancer vaccines could be a big help in fighting cancer. They might work alone or with other treatments.
In summary, immunotherapy is changing how we treat cancer. It uses the body’s immune system to fight tumors. As research grows, we’ll see even better treatments for cancer patients around the world.
Hormone Therapy for Hormone-Sensitive Tumors
Hormone therapy is key in treating cancers that rely on hormones. It targets tumors sensitive to hormones, like some breast, prostate, and uterine cancers.
Cancers Responsive to Hormone Therapy
Not all cancers are affected by hormones, but those that are can benefit from hormone therapy. Breast cancer and prostate cancer are prime examples. For breast cancer, tumors that respond to estrogen are treated with therapies that lower estrogen or block its action on cancer cells. In prostate cancer, treatments aim to reduce male hormones or stop them from growing cancer cells.
Other cancers, like uterine cancer and some ovarian cancer types, may also use hormone therapy. The choice depends on the cancer type, its hormone receptor status, and the patient’s health.
Types of Hormone Treatments
There are many hormone treatments, based on the cancer and its hormone sensitivity. For prostate cancer, treatments include:
- Orchiectomy (surgical removal of the testes to reduce testosterone levels)
- Gonadotropin-releasing hormone (GnRH) agonists or antagonists to decrease testosterone production
- Anti-androgens to block the action of male hormones
For breast cancer, treatments might involve:
- Aromatase inhibitors to lower estrogen levels
- Selective estrogen receptor modulators (SERMs) or downregulators to block estrogen receptors
- Ovarian suppression or ablation to reduce estrogen production
| Cancer Type | Hormone Therapy Approach | Mechanism of Action |
| Prostate Cancer | GnRH agonists/antagonists | Reduce testosterone production |
| Breast Cancer (ER-positive) | Aromatase inhibitors | Lower estrogen levels |
| Uterine Cancer | Progestins | Counteract estrogen’s effects |
Side Effects and Management
Hormone therapy can be effective but comes with side effects. Side effects vary by treatment type and cancer. For prostate cancer, hormone therapy can cause hot flashes, fatigue, and sexual problems. In breast cancer, it might lead to hot flashes, mood swings, and bone thinning.
It’s important to manage these side effects to keep quality of life during treatment. Lifestyle changes, medications, or alternative therapies can help. Patients should talk to their healthcare team to find the best way to manage side effects.
Neoadjuvant and Adjuvant Therapy Approaches
When treating solid tumors, two key approaches are used: neoadjuvant and adjuvant therapy. These methods aim to boost the main treatment’s success, usually surgery. They help improve patient results.
Treatment Before Surgery (Neoadjuvant)
Neoadjuvant therapy is given before surgery to shrink tumors. This makes them easier to remove. It also helps check how well the tumor responds to treatment.
Benefits of Neoadjuvant Therapy:
- Reduces tumor size, making surgery more manageable
- Helps in evaluating the effectiveness of the treatment
- Can potentially improve surgical outcomes
Treatment After Surgery (Adjuvant)
Adjuvant therapy is given after surgery to kill any cancer cells left behind. This lowers the chance of cancer coming back and boosts survival chances.
Key aspects of adjuvant therapy include:
- Targeting microscopic cancer cells that remain after surgery
- Reducing the risk of cancer recurrence
- Improving overall survival rates
Determining the Need for Additional Therapy
Choosing between neoadjuvant or adjuvant therapy depends on several factors. These include the cancer type and stage, the patient’s health, and the tumor’s characteristics.
Factors influencing the decision:
- Tumor size and location
- Cancer stage and grade
- Patient’s health status and preferences
Combination Therapy Strategies for Solid Tumors
Combination therapy is key in fighting solid tumors. It uses different treatments together to tackle cancer’s complexity. This way, we can create detailed plans to fight solid tumors effectively.
Benefits of Multi-Modal Treatment
Benefits of Multi-Modal Treatment
Combination therapy attacks cancer in many ways. This makes it harder for cancer to resist treatment. A top oncologist says,
“Combination therapy represents a paradigm shift in cancer treatment, allowing us to attack tumors from multiple angles and potentially achieve more durable responses.”
This method combines surgery, radiation, chemotherapy, targeted therapy, and immunotherapy. It lets us customize treatment based on the tumor’s unique traits. This can lead to better results for patients.
Common Combination Protocols
Protocols for combining treatments vary by tumor type and stage. For example, some use chemotherapy before surgery for breast and lung cancers. Others use radiation and chemotherapy together for advanced tumors.
- Chemotherapy combined with radiation therapy for enhanced local control
- Surgery followed by adjuvant therapy to eliminate residual cancer cells
- Targeted therapy in combination with immunotherapy to leverage the body’s immune response
Balancing Efficacy and Toxicity
It’s important to balance how well treatment works and its side effects. Combining treatments can be more effective but also raises the risk of harm. So, we must carefully manage these treatments to keep side effects low while keeping treatment effective.
To find this balance, we adjust doses, use supportive care, and watch how patients react. As we learn more about cancer and treatment, we can make combination therapy better for patients.
Treatment for Pediatric Solid Tumors
For pediatric solid tumors, a custom treatment plan is key. These cancers need special care that’s different from adult cancers.
Common Childhood Solid Tumors
Childhood solid tumors include neuroblastoma, Wilms tumor, and rhabdomyosarcoma. Each type needs its own treatment plan.
| Type of Tumor | Typical Age Group | Common Treatment Approaches |
| Neuroblastoma | Infants and young children | Surgery, chemotherapy, radiation therapy |
| Wilms Tumor | Children aged 3-4 years | Surgery, chemotherapy |
| Rhabdomyosarcoma | Children and adolescents | Surgery, chemotherapy, radiation therapy |
Special Considerations in Pediatric Oncology
Pediatric oncology is more than treating cancer. It’s about the child’s health, mind, and future. Family-centered care is key, keeping the family involved in care.
Long-term Follow-up Care
Survivors of pediatric solid tumors need ongoing care. This includes watching for treatment side effects, managing health issues, and supporting their mental health. A detailed follow-up plan helps survivors live healthy lives.
Treating pediatric solid tumors is complex. It needs a team of experts. With specialized care and support, we can help children with these tough cancers.
Personalized Medicine in Solid Tumor Treatment
As we learn more about cancer, personalized medicine is key in treating solid tumors. It means treating each patient based on their unique needs. This is a big step forward in fighting cancer.
Genetic Testing and Biomarkers
Genetic testing and biomarkers are vital in personalized medicine. They help us find out what’s causing a tumor to grow. This lets us choose treatments that are more likely to work.
Biomarkers also help us see how well a treatment is working. They tell us if a tumor is responding to a treatment. This helps us change the treatment plan if needed.
“The integration of genetic testing and biomarkers into clinical practice has revolutionized the way we approach cancer treatment, enabling us to provide more effective and personalized care to our patients.”
Tailoring Treatment to Individual Patients
Personalized medicine lets us tailor treatments to each patient. We look at genetic mutations, tumor type, and what the patient wants. This way, we create a treatment plan that’s just right for them.
- Identifying specific genetic mutations that drive tumor growth
- Selecting targeted therapies that are more likely to be effective
- Monitoring treatment response using biomarkers
- Adjusting treatment plans based on patient response and preferences
Future Directions in Personalized Oncology
The field of personalized oncology is growing fast. New technologies and treatments are being developed all the time. Liquid biopsies and advanced targeted therapies are some of the new things coming.
As we keep moving forward, personalized medicine will play an even bigger role in treating solid tumors. By understanding cancer better and creating new tools, we can give our patients better care.
Managing Recurrent Solid Tumors
Managing recurrent solid tumors requires a detailed plan. This includes finding the tumor, treating it, and supporting the patient’s mental health. When a tumor comes back, we need to look at the patient’s situation again and plan a new treatment.
Detection of Recurrence
Finding a tumor early is key to managing it well. We use scans like CT, MRI, and PET to spot tumors early. This helps us act fast.
Patients who have had tumors before need regular check-ups. These visits help us catch any new tumors early. This way, we can treat them quickly.
Treatment Options for Recurrent Disease
Choosing a treatment for a tumor that comes back depends on many things. These include the type of cancer, where the tumor is, and the patient’s health. We look at options like surgery, radiation, chemotherapy, targeted therapy, and immunotherapy.
| Treatment Option | Description | Applicability |
| Surgery | Removal of the recurrent tumor | Localized recurrence |
| Radiation Therapy | High-energy rays to kill cancer cells | Inoperable or widespread recurrence |
| Chemotherapy | Drugs to kill rapidly dividing cells | Systemic recurrence |
Psychological Support During Recurrence
Living with a tumor that comes back is tough for patients and their families. We stress the need for mental support. This includes counseling and joining support groups to handle the stress and feelings of recurrence.
Our goal is to make life better for patients with recurring tumors. We do this by giving them care that includes mental support.
Clinical Trials and Emerging Solid Tumor Treatment Options
The field of solid tumor treatment is always changing. This is thanks to ongoing clinical trials. These trials help check if new treatments are safe and work well. They also give patients access to new therapies that might not be available yet.
Accessing Clinical Trials
To join a clinical trial, patients must meet certain criteria. This includes the type and stage of their cancer, past treatments, and overall health. It’s key for patients to talk about their eligibility with their doctor.They can also look for trials online at .
Choosing to join a clinical trial is a big decision. Patients should know the possible benefits and risks well.
Promising New Treatment Approaches
New treatments being tested include immunotherapies, targeted therapies, and mixtures of treatments. Immunotherapy uses the body’s immune system to fight cancer, showing promise for some. Targeted therapies aim at specific cancer-causing molecules.
- Checkpoint inhibitors
- CAR T-cell therapy
- Personalized neoantigen-based therapies
Considerations Before Joining a Trial
Before joining a trial, patients should think about several things. This includes the benefits and risks, the trial’s design, and what to expect. It’s also vital to know their rights and how their safety is protected.
| Consideration | Description |
| Potential Benefits | Access to new treatments, closer monitoring, and helping medical research |
| Potential Risks | Unknown side effects, possible ineffectiveness, and extra challenges |
| Trial Design | Understanding if the trial is randomized, controlled, and its phase |
By carefully thinking about these points and talking with their healthcare team, patients can make smart choices about joining trials.
Conclusion: The Future of Solid Tumor Treatment
The treatment of solid tumors is complex and involves many steps. Ongoing research and new treatments are making progress. We see big steps forward in cancer therapy, like targeted therapy and immunotherapy.
Understanding solid tumors better and finding new treatments gives hope to patients. As we keep exploring, more people will get better care and live better lives.
The outlook for solid tumor treatment is good, with new therapies coming. We’re dedicated to top-notch healthcare and support for patients from around the world.
FAQ
What are solid tumors and how are they different from other types of cancer?
Solid tumors are abnormal tissue masses that can be benign or malignant. They are different from liquid cancers like leukemia because they form a distinct tumor mass. We discuss their classification and differences in our section on Understanding Solid Tumors.
What is the multidisciplinary approach to solid tumor treatment?
The multidisciplinary approach involves a team of specialists. This team includes surgeons, medical oncologists, and radiation oncologists. They work together to create a treatment plan tailored to the patient’s needs.
How are solid tumors diagnosed and staged?
Diagnosis uses imaging studies and biopsies. Staging is key to understanding the disease’s extent. It helps guide treatment decisions. We explain these steps in our section on Diagnosis and Staging of Solid Tumors.
What are the treatment options for solid tumors?
Treatment options include surgery, radiation therapy, and chemotherapy. Targeted therapy, immunotherapy, and hormone therapy are also used. The choice depends on the tumor’s type, stage, and location, along with the patient’s health.
What is the role of surgery in solid tumor treatment?
Surgery is often the primary treatment for solid tumors. It aims to remove the tumor completely. We discuss different cancer surgeries and the benefits of minimally invasive techniques in our section on Surgical Removal of Solid Tumors.
How does radiation therapy work against solid tumors?
Radiation therapy uses high-energy rays to kill cancer cells or slow their growth. It can be delivered externally or internally. We explain the different types and how to manage side effects in our section on Radiation Therapy for Solid Tumors.
What is targeted therapy and how is it used in solid tumor treatment?
Targeted therapy uses drugs that target cancer cells’ molecular characteristics. It’s used for tumors with specific genetic mutations or biomarkers. We discuss the concept, types, and effectiveness in our section on Targeted Therapy for Solid Tumors.
Can immunotherapy be used to treat solid tumors?
Yes, immunotherapy is used for certain solid tumors. It harnesses the immune system to fight cancer. Types include checkpoint inhibitors, CAR T-cell therapy, and cancer vaccines. We explore the different types and their benefits in our section on Immunotherapy.
What is the significance of neoadjuvant and adjuvant therapy in solid tumor treatment?
Neoadjuvant therapy is given before the main treatment, usually surgery, to shrink the tumor. Adjuvant therapy is given after to reduce recurrence risk. We discuss their benefits and purposes in our section on Neoadjuvant and Adjuvant Therapy Approaches.
How is combination therapy used in treating solid tumors?
Combination therapy uses multiple treatments, like chemotherapy and radiation, together or in sequence. It aims to increase effectiveness and reduce resistance. We discuss the benefits and challenges in our section on Combination Therapy Strategies for Solid Tumors.
Are clinical trials available for new solid tumor treatments?
Yes, clinical trials are available for testing new treatments. We provide information on accessing clinical trials and considerations before joining in our section on Clinical Trials and Emerging Solid Tumor Treatment Options.
What is personalized medicine in the context of solid tumor treatment?
Personalized medicine tailors treatment to the patient’s tumor characteristics, using genetic testing and biomarkers. We discuss its role in our section on Personalized Medicine in Solid Tumor Treatment.
How are recurrent solid tumors managed?
Managing recurrent solid tumors involves early detection and choosing treatment options. This may include surgery, radiation, chemotherapy, or other therapies. We discuss the challenges and options in our section on Managing Recurrent Solid Tumors.
What are the future directions in solid tumor treatment?
Future directions include advancements in personalized medicine, immunotherapy, and targeted therapy. Improvements in surgical techniques and combination therapy protocols are also expected. We highlight progress and hope in cancer therapy in our concluding section.
References
- Huang, J., & Zhang, L. (2021). The role of surgery in the multidisciplinary management of solid tumors. Journal of Clinical Medicine, *10*(15), 3298. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8347462/








