Last Updated on December 1, 2025 by Bilal Hasdemir
A diagnosis of Diffuse Intrinsic Pontine Glioma (DIPG) is very tough, mainly when it hits kids. It’s a big deal because DIPG makes up about 10% of all brain tumors in children. This shows we really need good ways to treat it. Discover whether DIPG removal is possible and why surgery is often not an option.
Even though surgery is hard because of where the tumor is, we’re looking for other ways to help.
Whether DIPG can be surgically removed is a tough question. We’re all about bringing new ways to manage this disease. We want to give hope to patients and their families.
Key Takeaways
- Understanding DIPG and its impact on patients and families.
- Exploring the challenges and limitations of DIPG treatment.
- Discussing recent advancements in DIPG management.
- The role of surgical removal in DIPG treatment.
- Alternative treatment options for DIPG patients.
Understanding DIPG: A Complex Brain Tumor

DIPG is a rare and aggressive brain tumor. It’s located in the brainstem, which controls vital functions. Knowing about DIPG is key to finding effective treatments.
What is Diffuse Intrinsic Pontine Glioma?
DIPG is a type of brain tumor that starts in the brain stem, called the pons. It spreads and grows quickly, making it hard to remove surgically. This tumor is known for its fast growth and poor outlook.
Key characteristics of DIPG include:
- High-grade glioma
- Originates in the brain stem (pons)
- Diffuse and infiltrative nature
- Aggressive behavior
- Poor prognosis
Prevalence and Demographics
DIPG mainly affects children, with about 200 to 400 cases in the US each year. It’s rare but very aggressive, impacting young lives deeply.
| Demographic | Characteristics |
| Age | Primarily affects children |
| Annual Incidence (US) | 200 to 400 cases |
| Tumor Location | Brain stem (pons) |
Why DIPG is Different from Other Brain Tumors
DIPG is unique because it’s in the brainstem. This area controls basic life functions like breathing and heart rate. Its spread makes it hard to treat surgically.
Because of its complexity, DIPG needs a detailed treatment plan. A team of experts is often involved. Understanding DIPG is vital for finding the best dipg brain tumor treatment and dipg surgery options for kids.
The Challenging Location of DIPG Tumors

DIPG tumors in the brainstem are hard to treat. The brainstem connects the cerebrum to the spinal cord. It controls many vital functions of our body.
Anatomy of the Brainstem and Pons
The brainstem has three main parts: the midbrain, pons, and medulla oblongata. DIPG tumors are in the pons. This area controls breathing, heart rate, and blood pressure.
The pons also manages sleep and swallowing. It’s a key part of our brain.
Critical Functions Controlled by the Affected Area
The pons controls important functions. It regulates sleep, manages sensory information, and helps different brain parts communicate. The complex network of nerve fibers and nuclei makes surgery hard.
Damage during surgery can cause big problems. It can affect a patient’s quality of life. So, it’s key to understand the pons’ functions when thinking about DIPG tumor resection.
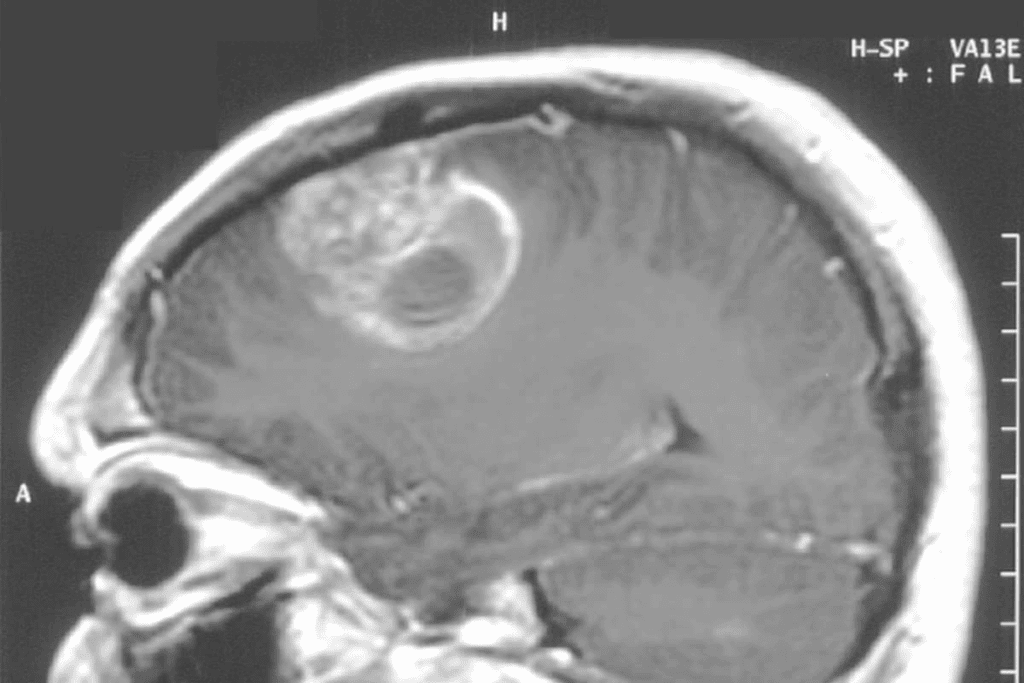
Imaging Characteristics of DIPG
Diagnosing DIPG uses advanced imaging like MRI. DIPG tumors look like diffuse, infiltrative lesions in the pons. They often spread into the surrounding brainstem structures.
This makes it hard to plan surgery. MRI sequences like diffusion-weighted imaging and MR spectroscopy help. But, DIPG’s growth into the brainstem tissue is a big challenge for surgery.
Why Traditional DIPG Removal Is Rarely Performed
Removing DIPG through surgery is rare because of many challenges. Diffuse Intrinsic Pontine Glioma (DIPG) is a tough brain tumor to treat. This is because of its location and nature.
Infiltrative Nature of DIPG
DIPG is known for its infiltrative nature. This makes it hard to tell the tumor from healthy tissue. It’s tough to remove the tumor without harming important brain parts.
The way DIPG grows makes it hard to find a clear boundary for surgery. The tumor cells mix with normal brain cells, making it hard to separate them.
Surgical Risks in the Brainstem Region
The brainstem, where DIPG is found, controls vital functions. These include breathing, heart rate, and blood pressure. Surgery in this area is risky, as it can cause serious brain damage or even death.
Doctors must think carefully about the benefits and risks of surgery. They consider the brainstem’s delicate nature and the critical functions it controls.
Historical Attempts at Surgical Resection
In the past, trying to remove DIPG surgically has had limited success. The tumor’s spread and the risks of surgery in the brainstem have led to a cautious approach. Surgery is not usually the first treatment option.
Even so, surgery might be considered in some cases. This could be for diagnostic purposes or to relieve symptoms.
In summary, removing DIPG through traditional surgery is rare. This is because of its spread and the risks of surgery in the brainstem. Understanding these challenges helps in finding better treatment options that protect the brain while treating the tumor.
Current Surgical Approaches to DIPG
Today, surgery for DIPG aims to improve diagnosis and treatment. Removing the tumor completely is hard because of its location and how it spreads. Yet, new surgical methods are being used to help patients more.
Biopsy Procedures and Their Value
Biopsies are key in diagnosing and treating DIPG. They give tissue samples that help understand the tumor’s genetics. This info is vital for making treatment plans that target the tumor.
Biopsy procedures have improved, with methods like stereotactic biopsy used to reduce risks. The value of biopsy is in giving a clear diagnosis. It’s also important for finding genetic targets for treatment.
Partial Resection Possibilities
In some cases, partial resection of DIPG is considered. This means removing part of the tumor to ease symptoms or reduce its size. It’s not a cure but can improve life quality by lessening symptoms.
Whether partial resection is possible depends on the tumor’s size, location, and the patient’s health. Advanced imaging and planning tools help assess the risks and benefits.
Debulking Surgery Considerations
Debulking surgery is another strategy for managing DIPG. It involves making the tumor smaller to ease symptoms and help other treatments work better.
When thinking about debulking surgery, the benefits must be weighed against the risks, like those from brainstem surgery. The decision is made based on the patient’s condition and the tumor’s specifics.
We understand that every patient is different. Surgical choices are made by a team of experts. The goal is to offer the best care, balancing diagnosis, treatment, and quality of life.
DIPG Removal: Challenges and Limitations
Removing DIPG is hard, even with new medical tools. The problems with removing DIPG are many.
Technical Surgical Barriers
The main issue is where the tumor is in the brainstem. This area controls important body functions. Advanced imaging and precise tools are key for surgery here.
Surgeons must be very careful in the brainstem. They need to plan well before surgery and watch closely during it. This keeps the patient safe.
Diffuse Nature of the Tumor
DIPG spreads out, making it hard to find and remove. Its growth pattern makes it hard to get rid of because it mixes with healthy brain cells.
This spread makes surgery and other treatments harder. Knowing how far the tumor has spread is key to finding good treatments.
Post-Surgical Complications
After surgery, patients face many risks. The tumor’s location and the brain’s sensitivity can lead to problems. These can include nerve damage, infection, and fluid leaks.
Dealing with these issues needs a detailed care plan. Rehabilitation and comfort care are important for recovery and quality of life.
In summary, removing DIPG is tough due to many challenges. From surgery’s technical hurdles to the tumor’s spread and post-op risks. Knowing these issues helps in making better treatment plans and improving patient care.
The Reality of DIPG Surgery Outcomes
DIPG surgery results depend on many things. These include where the tumor is and the patient’s health. Knowing these outcomes helps patients and their families understand DIPG treatment better.
Survival Statistics After Surgical Intervention
Survival rates for DIPG are low, with a median survival time of about nine months after diagnosis. Surgery’s success can vary a lot. This depends on how much of the tumor is removed and the patient’s health after surgery.
Research shows that patients who have surgery for DIPG live for different lengths of time. Some studies say they live from 6 to 12 months. The dipg surgery prognosis is usually not good because of the tumor’s aggressive nature and location.
- Median survival time after diagnosis: approximately 9 months
- Survival range after surgery: 6 to 12 months
- Factors influencing survival: extent of resection, neurological status, overall health
Quality of Life Considerations
Quality of life is very important when treating DIPG patients. Surgery tries to remove as much tumor as possible. It also aims to keep neurological function and improve quality of life.
Key quality of life considerations include:
- Managing symptoms effectively
- Maintaining neurological function
- Minimizing treatment side effects
Healthcare providers focus on these areas to help DIPG patients live better lives. This is despite the challenges the tumor poses.
Case Studies and Their Implications
Many case studies have shown the complexities and results of DIPG surgery. These studies offer insights into the benefits and risks of surgery.
A case study on a patient who had part of their DIPG tumor removed showed improved symptom management and a temporary halt in the disease’s growth. But, the dipg tumor survival rates were a concern. The patient lived for 10 months after surgery.
These case studies highlight the need for personalized treatment plans. They also show the importance of ongoing research into better DIPG treatments.
When thinking about dipg survival with surgery, it’s key to consider the benefits and risks. Discussing these with a healthcare provider is essential.
Standard Treatment Protocol for DIPG
The standard treatment for DIPG combines several therapies to improve patient outcomes. This approach is needed because of the tumor’s complexity and location.
Radiation Therapy as Primary Treatment
Radiation therapy is the main treatment for DIPG. It helps by shrinking the tumor and easing symptoms. The treatment involves doses of about 54 Gy, spread over weeks.
Radiation therapy helps with symptoms like headaches and nausea. But, it doesn’t greatly improve survival rates because DIPG is so aggressive.
Chemotherapy Options
Chemotherapy is often paired with radiation therapy. Researchers are studying its effectiveness against DIPG. Agents like temozolomide and vincristine are being tested.
| Chemotherapy Agent | Mechanism of Action | Common Side Effects |
| Temozolomide | Alkylating agent that damages DNA | Nausea, fatigue, hair loss |
| Vincristine | Mitotic inhibitor that disrupts cell division | Neuropathy, constipation, hair loss |
Steroid Treatment for Symptom Management
Steroids, like dexamethasone, help manage DIPG symptoms. They reduce swelling and improve neurological function. But, they’re not a long-term fix.
“Steroids can dramatically improve the quality of life for DIPG patients by reducing swelling and alleviating symptoms, but their use must be carefully managed due to possible side effects.”
Multidisciplinary Approach to Care
Managing DIPG requires a team effort. Neurosurgeons, radiation oncologists, pediatric oncologists, and palliative care specialists work together. They tailor treatments to each patient’s needs.
This team approach improves symptom management and quality of life. It ensures a more personalized care plan, addressing all aspects of the patient’s condition.
Experimental Approaches to DIPG Removal
New ways to treat DIPG are being explored thanks to medical research. These new methods aim to help patients with this tough brain tumor.
There’s a big change in how we treat DIPG. New surgical techniques like convection-enhanced delivery and laser interstitial thermal therapy are showing promise. Robotic and computer-assisted surgery are also being used.
Emerging Surgical Techniques
New surgical methods for DIPG focus on being precise and protecting the brain. Robotic-assisted surgery is one of these advancements. It gives surgeons better control and accuracy during tough operations.
“The integration of robotics in neurosurgery has opened new avenues for the treatment of complex brain tumors like DIPG.”
Convection-Enhanced Delivery
Convection-enhanced delivery (CED) directly puts drugs into the tumor. This method helps get more drugs to the tumor and reduces side effects.
CED is being tested in clinical trials for DIPG. It’s a promising area for future research.
Laser Interstitial Thermal Therapy
Laser interstitial thermal therapy (LITT) uses laser heat to kill tumor cells. It tries to save the healthy tissue around it.
“LITT represents a significant advancement in the treatment of brain tumors, including DIPG.”
Robotic and Computer-Assisted Surgery
Robotic and computer-assisted systems are being used in DIPG surgeries. They give surgeons real-time data and better precision. This makes surgeries safer and more effective.
These new methods are promising for treating DIPG better. They’re early steps, but they’re important in the fight against this disease.
Innovative Non-Surgical Treatments for DIPG
The medical world is seeing big changes in treating Diffuse Intrinsic Pontine Glioma (DIPG). New non-surgical methods are coming up. These offer hope for better care for patients.
Immunotherapy Developments
Immunotherapy uses the body’s immune system to fight cancer. Checkpoint inhibitors and CAR T-cell therapy are being looked at. They aim to boost the body’s fight against the tumor.
Immunotherapy could change how we treat DIPG. It uses the immune system to fight the tumor, which could lead to better treatments.
Targeted Molecular Therapies
Targeted molecular therapies focus on specific genetic changes in DIPG. They aim to find and attack the tumor’s weak spots. This could lead to treatments that work better and have fewer side effects.
Precision medicine is being studied. It tailors treatments to each patient’s unique genetic makeup.
Blood-Brain Barrier Disruption Techniques
The blood-brain barrier (BBB) makes it hard to get drugs to DIPG. Scientists are working on ways to open the barrier. This would let drugs reach the tumor more easily.
Focused ultrasound and BBB disruption technologies are being tested. They could make treatments more effective.
Gene Therapy Approaches
Gene therapy adds healthy genes to cells to fix faulty ones. For DIPG, it tries to fix the genetic problems that cause the tumor. It’s a new area of research, but it shows promise.
As we keep exploring these new treatments, the future of DIPG care looks bright. By combining the latest research with caring for patients, we can make a difference in their lives.
Clinical Trials for DIPG Treatment
Clinical trials are a key way for DIPG patients to get new treatments. These trials help find better ways to fight DIPG. They give hope to patients and their families.
Current Active Trials
Many trials are happening now. They test new drugs and ways to treat DIPG. We keep up with these new options to help our patients.
Some of the ongoing trials involve:
- Novel drug combinations aimed at improving treatment results
- Immunotherapy to help the body fight DIPG cells better
- Targeted therapies that target specific genetic changes in tumors
Promising Research Directions
Research on DIPG is moving fast. New methods like convection-enhanced delivery and laser therapy are being tested. They might lead to better treatments.
How to Access Clinical Trials
Finding clinical trials can be hard. It involves checking if you’re a good match. Talk to your doctor to see if you qualify for a trial.
| Steps to Access Clinical Trials | Description |
| 1. Consultation | Discuss clinical trial options with your healthcare provider. |
| 2. Eligibility Assessment | Undergo evaluation to determine suitability for a specific trial. |
| 3. Trial Enrollment | Participate in the selected clinical trial, following the trial protocol. |
Considerations for Trial Participation
Think about the good and bad before joining a trial. Know what the trial aims to do and what side effects might happen. Talking openly with your team is key.
Trials offer new treatments and help research. They can lead to better care for others in the future.
Decision-Making Process for DIPG Treatment
Choosing the right treatment for DIPG is complex. A team of experts, like neurosurgeons and oncologists, work together. They aim to create a plan that meets each patient’s needs.
Medical Team Considerations
A team of doctors is key in deciding DIPG treatment. Neurosurgeons, oncologists, radiologists, and palliative care specialists come together. They look at the tumor, the patient’s health, and the pros and cons of treatments.
Family Involvement in Treatment Choices
Families are important in making DIPG treatment choices. Open communication helps everyone understand the plan. Families offer emotional support and help make decisions that match the patient’s wishes.
Quality of Life Factors
Quality of life matters a lot in DIPG treatment. The team looks at how treatment might affect the patient’s life. Palliative care helps manage symptoms and improve life, even with a tough diagnosis like DIPG.
Second Opinion Importance
Getting a second opinion is a big part of deciding on DIPG treatment. A second opinion can provide additional insights. It can also lead to new treatment options that were not considered first.
By considering these factors and working with a team, patients and families can make informed choices. These choices focus on the patient’s well-being and quality of life.
Palliative Care Approaches for DIPG
Palliative care is key in managing DIPG, focusing on controlling symptoms and improving life quality. It’s vital to prioritize the patient’s comfort and well-being as we tackle DIPG treatment.
Symptom Management Strategies
Managing symptoms is critical in DIPG care. We use many strategies to reduce pain, nausea, and swallowing issues. Medications are a big help, and we work with patients and families to find the best approach.
Physical therapy and occupational therapy also play a big role. They help patients stay functional and independent. These therapies are customized to meet each patient’s needs, greatly improving their life quality.
Supportive Care Options
Supportive care is a big part of DIPG care, covering physical, emotional, and social needs. We offer a wide range of services, like counseling, nutritional support, and spiritual care.
- Counseling services to address emotional and psychological distress
- Nutritional support to manage dietary needs and preferences
- Spiritual care to provide comfort and support during challenging times
Improving Quality of Life
Our main goal is to enhance the patient’s life quality, despite DIPG’s challenges. We do this by providing detailed palliative care that meets their unique needs and preferences.
By focusing on symptom management, supportive care, and emotional well-being, we greatly improve life quality. This approach helps patients keep their dignity and comfort, even with serious illness.
End-of-Life Considerations
As DIPG advances, end-of-life care becomes a key consideration. We work closely with patients and families to respect their wishes and meet their needs.
This includes discussing advance care planning, pain management, and other end-of-life matters. Our team offers compassionate support, ensuring patients receive the care they need to stay comfortable and dignified.
By focusing on palliative care and addressing DIPG patients’ complex needs, we can enhance their life quality. We provide the support they need throughout their journey.
International Perspectives on DIPG Treatment
Looking at DIPG treatment worldwide shows a mix of strategies and new research areas. This rare and aggressive brain tumor mainly hits kids, making it a big challenge everywhere. This leads to different ways to tackle it.
Treatment Variations Across Countries
DIPG treatment varies a lot from country to country. It’s shaped by things like local health policies, medical setup, and research focus. For example, some places might get to try new clinical trials, while others stick to what’s known.
Key differences in DIPG treatment approaches include:
- Availability of advanced radiation therapy techniques
- Access to experimental therapies through clinical trials
- Use of innovative surgical techniques
- Integration of palliative care services
Centers of Excellence for DIPG
Some places around the world are leading in DIPG care and research. They offer special treatments and help a lot in understanding this condition. These centers also work together, sharing knowledge and resources to move the field forward.
“Collaboration is key in the fight against DIPG. By working together, we can accelerate the development of effective treatments and improve patient outcomes globally.”
Global Collaborative Research Efforts
Working together is key to tackling DIPG. International partnerships help share data, resources, and skills. This lets researchers do bigger, better studies, which is important for finding new treatments.
Some big global efforts include:
- International clinical trials for DIPG treatments
- Global DIPG registries for data collection and analysis
- Collaborative research networks focusing on DIPG biology and treatment
Access to Specialized Care
Getting to specialized DIPG care is not the same everywhere. Some patients get full care at special centers, but others face barriers like distance, cost, or healthcare system issues.
Efforts to improve access to specialized care include:
- Telemedicine services for remote consultations
- Patient support programs for financial assistance
- Education and training for healthcare professionals in DIPG management
Conclusion
DIPG is a tough condition to treat because of its complex nature and brain location. Traditional treatments often can’t remove it. But, new research and treatments offer hope for better patient outcomes.
Dealing with DIPG needs a caring and all-around approach. Research into new treatments and surgeries gives us hope. We aim to give top-notch care and support to patients from around the world.
We’re working hard to find new treatments and improve existing ones. The question of removing DIPG surgically is being looked into. Our goal is to provide the latest care and support to those facing this condition.
FAQ
What is DIPG and how is it different from other brain tumors?
DIPG, or Diffuse Intrinsic Pontine Glioma, is a brain tumor that starts in the pons. This part of the brainstem controls important functions. Because of its location, DIPG is hard to treat surgically.
Can DIPG be surgically removed?
Removing DIPG through surgery is not common. This is because of its location and how it spreads. Yet, doctors are looking into other surgical methods like biopsies and partial removals.
What are the current surgical approaches to DIPG?
Doctors use biopsies to diagnose DIPG. They also try partial removals and debulking surgery. These methods aim to help patients by reducing tumor size and improving symptoms.
What are the challenges and limitations of DIPG removal?
Removing DIPG is hard because of its location and how it spreads. It’s also risky because of possible complications after surgery. These issues make surgery a less likely option.
What is the standard treatment protocol for DIPG?
Treatment for DIPG includes radiation, chemotherapy, and steroids. This approach aims to improve life quality and extend life. It’s a team effort to care for patients.
Are there any experimental approaches to DIPG removal?
Yes, new methods like convection-enhanced delivery and laser therapy are being tested. These could lead to better treatment results.
What innovative non-surgical treatments are being developed for DIPG?
New treatments include immunotherapy and gene therapy. These options offer hope for DIPG patients.
How can patients access clinical trials for DIPG treatment?
Patients can find trials through their doctors or online. It’s important to understand the risks and benefits of participating.
What factors are important in the decision-making process for DIPG treatment?
Important factors include a team of doctors and family input. Quality of life and seeking a second opinion are also key. These help create a complete treatment plan.
What is the role of palliative care in DIPG management?
Palliative care focuses on managing symptoms and improving life quality. It’s a vital part of DIPG care, ensuring patients receive full support.
How does DIPG treatment vary across different countries?
Treatment for DIPG varies worldwide. Some places are leaders in care and research. But, getting specialized care can be hard.
What are the survival statistics after DIPG surgery?
Survival rates after surgery depend on several factors. Understanding these statistics helps set realistic hopes for patients.
How does the location of DIPG affect treatment options?
DIPG’s location in the brainstem limits treatment options. It controls vital functions and poses risks. Knowing the anatomy is key to understanding treatment possibilities.
References
- Djouder, N., & Rigual, M. del Mar. (2025). CNIO researchers discover a new mechanism for rapid liver regeneration triggered by glutamate. Nature. https://www.cnio.es/en/news/cnio-researchers-discover-a-new-mechanism-for-rapid-liver-regeneration-triggered-by-glutamate/





