Last Updated on December 1, 2025 by Bilal Hasdemir

Neuroblastoma is a big worry in childhood cancer research. It’s one of the top solid tumors found outside the brain in kids. This emphasizes the importance of accurately identifying and diagnosing pediatric solid tumor types.
We need to classify medical tumors accurately to help kids. Looking into neuroblastoma, we see how key early spotting and detailed treatment plans are. They help make a big difference in how well kids do.
Key Takeaways
- Neuroblastoma is a common extracranial solid tumor in children.
- Understanding pediatric solid tumor types is key for diagnosis and treatment.
- Medical tumor classification is very important in childhood cancer research.
- Early detection and detailed care are essential for better results.
- Getting the diagnosis right is critical for the right treatment.
Overview of Childhood Solid Tumors
Childhood solid tumors are a complex group of cancers. They have different looks and symptoms. Knowing what they are helps doctors diagnose and treat them better.
Definition and Distinguishing Features
Childhood solid tumors are abnormal growths of tissue. They are not like blood cancers because they form solid masses. These masses can appear anywhere in the body.
Neuroblastoma comes from nerve cells, and Wilms tumor from kidney cells. This shows how different these tumors can be.
“The diversity in the histological features of childhood solid tumors necessitates a comprehensive diagnostic approach,” say pediatric oncologists. Doctors use imaging, tissue tests, and genetic analysis to diagnose.
Epidemiology in Pediatric Populations
The occurrence of childhood solid tumors changes with age and location. Neuroblastoma is the most common, making up 6% of childhood cancers. Other common ones are Wilms tumor, rhabdomyosarcoma, and Ewing sarcoma.
Some tumors are more common in babies, while others hit kids a bit older. For example, Wilms tumor often shows up in kids under 5, peaking at 3 to 4 years old. Knowing this helps doctors catch these tumors early.
Looking into each tumor type shows we need a team effort to treat them. Doctors, surgeons, and others work together for the best care.
Neuroblastoma: The Leading Extracranial Solid Tumor
Neuroblastoma is the top solid tumor outside the brain in kids. It’s important to know where it comes from and how it shows up. We’ll look at how it starts, its signs, and what might make it more likely to happen.
Embryological Origin and Development
Neuroblastoma starts from cells called neural crest cells. These cells help make the nervous system. The tumor can grow anywhere along the nervous system, from the neck to the pelvis. It happens because of genetic changes that mess up how cells grow and work.
Studies show that neuroblastoma is linked to changes in genes that control cell growth. Knowing this helps us find better treatments. We’re working to understand how genes and the environment work together to cause neuroblastoma.
Incidence and Age Distribution
Neuroblastoma is about 6% of all childhood cancers. It’s the most common tumor outside the brain in kids. Most cases happen in the first year of life. Finding it early is key to better treatment for kids.
- Most cases happen in the first year.
- Most are found before age 5.
- It’s very rare in older kids and adults.
Clinical Presentation and Symptoms
How neuroblastoma shows up can vary a lot. Symptoms include a big tummy, bulging eyes, and bone pain. Doctors use imaging and tests to find it, like checking urine for certain chemicals.
Screening tests are very important for catching neuroblastoma early. Tools like MRI and CT scans help see how big the tumor is. These help doctors plan the best treatment.
Genetic and Environmental Risk Factors
Genes and the environment both play a part in getting neuroblastoma. Genes are a big risk factor, with some families more likely to get it. But how the environment affects it is not as clear.
- Genetic changes, like in the ALK gene, raise the risk.
- Having family members with neuroblastoma or other cancers matters.
- Some chemicals might also play a role, but it’s not proven yet.
It’s important to understand how genes and the environment work together. This helps us find ways to prevent and treat neuroblastoma better. We keep studying to get better at this.
Comprehensive Guide to Pediatric Solid Tumor Types
Pediatric solid tumors are a wide range of cancers that need to be classified well for treatment. They can start in different tissues and organs, making diagnosis and treatment tricky.
Classification Based on Tissue Origin
Pediatric solid tumors are grouped by where they start. Knowing this helps doctors understand the tumor and choose the best treatment.
- Neuroblastomas: These tumors start in neural crest cells and are common in young kids.
- Wilms Tumor: Starting in the kidneys, Wilms tumor is a common cancer in kids.
- Rhabdomyosarcomas: These tumors start in muscle cells and are a type of soft tissue cancer.
- Brain Tumors: Including medulloblastoma, astrocytomas, and ependymomas, these tumors start in brain cells.
- Bone Tumors: Osteosarcoma and Ewing’s sarcoma are common bone cancers in kids.
Developmental and Genetic Considerations
Pediatric solid tumors often start from genetic changes and developmental factors. Knowing these causes helps in early detection and treatment.
Some tumors are linked to genetic syndromes, such as:
- Li-Fraumeni syndrome and its link to various childhood cancers.
- Beckwith-Wiedemann syndrome associated with Wilms tumor.
Relative Frequency and Distribution
The types and how common they are change with age and location. For example, neuroblastoma is common in young kids, while osteosarcoma is more common in older kids and teens.
| Tumor Type | Typical Age Range | Relative Frequency |
| Neuroblastoma | 0-5 years | High |
| Wilms Tumor | 3-6 years | Moderate |
| Osteosarcoma | 10-16 years | Moderate |
Knowing how common these tumors are helps doctors diagnose and research better treatments.
Wilms Tumor: The Most Common Renal Malignancy
Wilms tumor is the most common kidney cancer in kids. It needs quick medical help. This cancer, also known as nephroblastoma, happens in the kidneys of children under 7.
Pathophysiology and Development
Wilms tumor starts from immature kidney cells and is linked to genetic mutations. It can grow big before it’s found, sometimes reaching the renal vein or inferior vena cava.
Genetic factors, like mutations in the WT1 gene, play a big role in Wilms tumor. These changes mess up normal kidney growth, causing tumors.
Clinical Manifestations
Kids with Wilms tumor often have a big belly mass. This is usually the first sign noticed by parents or doctors. They might also have belly pain, fever, and blood in their urine.
High blood pressure is common because of the tumor pressing on the kidney or making too much renin. In some cases, the tumor can burst, causing severe belly pain and serious problems.
Associated Syndromes and Genetic Factors
Some genetic syndromes raise the risk of Wilms tumor. These include WAGR syndrome, Denys-Drash syndrome, and Beckwith-Wiedemann syndrome.
Knowing about these genetic risks is key for early detection and treatment. Kids with these syndromes should get regular check-ups to catch Wilms tumor early.
Genetic Syndromes Associated with Wilms Tumor
| Syndrome | Characteristics | Risk of Wilms Tumor |
| WAGR Syndrome | Wilms tumor, Aniridia, Genitourinary anomalies, mental Retardation | High |
| Denys-Drash Syndrome | Early-onset nephrotic syndrome, genital anomalies, Wilms tumor | High |
| Beckwith-Wiedemann Syndrome | Overgrowth, macroglossia, omphalocele, increased cancer risk | Moderate |
Understanding Wilms tumor’s genetics and symptoms helps doctors give better care. This improves the chances of a good outcome for kids with this cancer.
Brain Tumors in the Pediatric Population
Brain tumors are common in kids and need careful study and treatment. We’ll look at the different types of brain tumors in children. We’ll also cover how they are diagnosed and treated.
Medulloblastoma Characteristics
Medulloblastoma is the most common brain tumor in kids. It starts in the cerebellum and can spread through the cerebrospinal fluid (CSF). Symptoms include headache, vomiting, and ataxia. We’ll talk about how medulloblastoma is staged and risk-stratified, which helps decide treatment.
Treatment for medulloblastoma includes surgery, chemotherapy, and radiation. New discoveries in genetics have found different types of medulloblastoma. This might change how we treat it in the future.
Astrocytomas and Ependymomas
Astrocytomas come from astrocytes in the brain. They can be low-grade (like pilocytic astrocytoma) or high-grade (like glioblastoma). Low-grade astrocytomas are more common in kids and often have a good outlook with the right treatment.
Ependymomas start from ependymal cells in the ventricles and spinal cord. They’re common in kids. The treatment depends on the tumor’s grade, location, and how much is removed.
Brainstem Gliomas and Other Rare Variants
Brainstem gliomas are tumors in the brainstem. This area controls many important functions. They are hard to remove surgically because they spread out. The outcome for brainstem gliomas varies, depending on the type.
Other rare tumors in kids include primitive neuroectodermal tumors (PNETs), atypical teratoid/rhabdoid tumors (ATRTs), and craniopharyngiomas. Each needs a special treatment plan because of its unique features.
| Type of Tumor | Common Age Group | Typical Location | Prognosis |
| Medulloblastoma | Children | Cerebellum/Posterior Fossa | Variable, depends on risk stratification |
| Pilocytic Astrocytoma | Children and young adults | Cerebellum, optic pathways | Generally favorable |
| Ependymoma | Children and adults | Near the ventricles | Varies based on grade and resection |
| Brainstem Glioma | Children | Brainstem | Generally poor, varies by subtype |
Rhabdomyosarcoma and Soft Tissue Sarcomas
Diagnosing and treating rhabdomyosarcoma and soft tissue sarcomas in kids is complex. We need to know about their different types and how they show up. We’ll look into these cancers, their traits, how to diagnose them, and what affects their outcome.
Embryonal and Alveolar Subtypes
Rhabdomyosarcoma comes in two main types: embryonal and alveolar. The embryonal subtype is common in young kids. It often shows up in the head, neck, or bladder area. It looks like muscle tissue from an embryo.
The alveolar subtype is more common in older kids and teens. It usually appears in the chest or limbs. It grows faster and has specific genetic changes.
Anatomical Distribution and Presentation
Rhabdomyosarcoma and other soft tissue sarcomas can happen in many places. Where the tumor is affects how it shows up. Tumors in the head and neck might cause bulging eyes, blocked nose, or nerve problems.
Tumors in the genitourinary tract can block urine or cause blood in the urine. Where and how big the tumor is when found matters a lot for treatment and chances of getting better.
Prognostic Factors and Risk Assessment
The outlook for kids with these cancers depends on several things. These include the type of cancer, how far it has spread, the child’s age, and how well it responds to treatment. We use a system to group patients by risk level.
This helps us decide how intense the treatment should be. Our goal is to cure as many patients as possible while keeping side effects low.
By knowing more about rhabdomyosarcoma and other soft tissue sarcomas, we can make treatments better. We can tailor them to meet each patient’s unique needs.
Bone Malignancies in Children
Bone cancers in kids are a big worry in pediatric oncology. Osteosarcoma and Ewing sarcoma are the top types. They need quick diagnosis and good treatment plans to help kids get better.
Osteosarcoma Characteristics and Demographics
Osteosarcoma is the main bone cancer in teens and young kids. It starts in bone tissue and makes bone matrix. It often happens when kids grow fast, suggesting a link between growth and cancer.
Key Features of Osteosarcoma:
- Most common in adolescents during the growth spurt
- Originates in bone tissue
- Characterized by osteoid production
Ewing Sarcoma Family of Tumors
Ewing sarcoma is a very aggressive tumor that can start in bones or soft tissues. It’s the second most common bone cancer in young people. It needs strong treatment like chemo, radiation, and surgery.
Ewing Sarcoma Characteristics:
- Highly malignant
- Arises in bones or soft tissues
- Requires intensive multimodal treatment
Less Common Bone Tumors
While osteosarcoma and Ewing sarcoma are common, other rare types like chondrosarcoma and malignant fibrous histiocytoma exist. These rare cancers need the right diagnosis and treatment too.
| Type of Bone Tumor | Characteristics | Typical Age Group |
| Osteosarcoma | Produces osteoid, most common primary malignant bone tumor | Adolescents |
| Ewing Sarcoma | Highly malignant, arises in bones or soft tissues | Children and young adults |
| Chondrosarcoma | Rare in children, involves cartilage | Adults, rare in children |
In conclusion, bone cancers in kids, like osteosarcoma and Ewing sarcoma, are big challenges. Knowing about them helps us find better ways to treat them.
Diagnostic Approaches and Imaging Techniques
Diagnosing childhood cancers involves many steps. We use different methods to find and treat cancer early. This ensures kids get the right care fast.
Initial Evaluation and Screening
First, we take a detailed medical history and do a physical check-up. We look for signs like tumors, nerve problems, or bone pain. Blood tests and other screenings help spot cancer signs.
Imaging is key in the early stages. Ultrasound is often the first choice because it’s safe and doesn’t use radiation. But, more tests are needed to understand the tumor better.
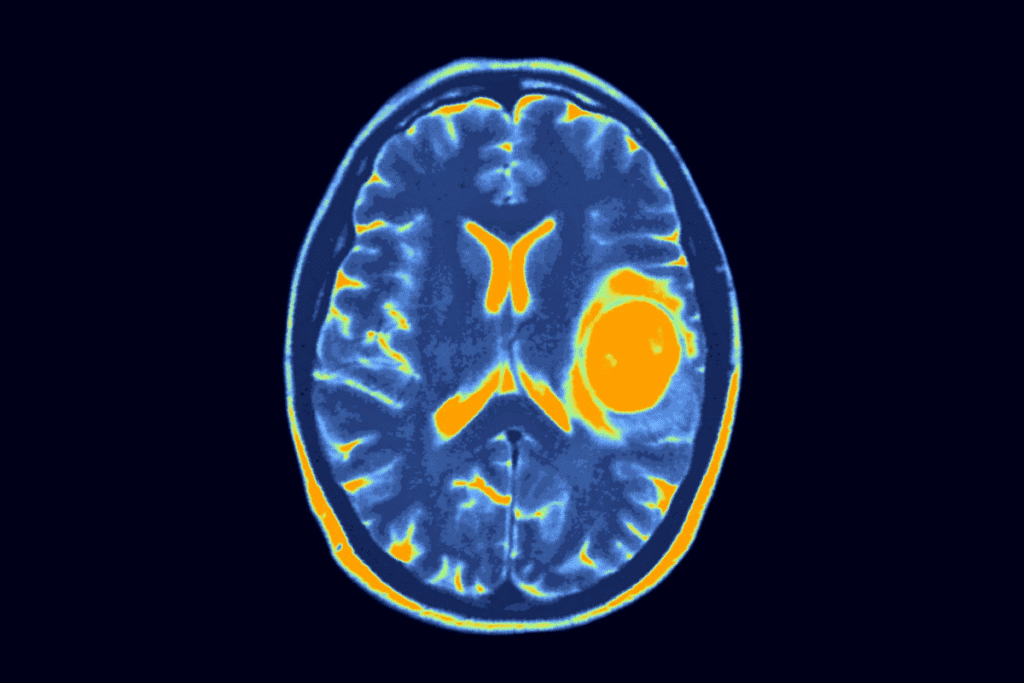
Advanced Imaging Modalities
For a detailed look at tumors, we use advanced imaging. Magnetic Resonance Imaging (MRI) is great for soft tissue tumors. It shows the tumor’s size and where it is. Computed Tomography (CT) scans help see tumors in the belly and chest. They give clear images for treatment planning.
Positron Emission Tomography (PET) scans check how active tumors are. They help tell if a tumor is cancerous and how well treatment is working.
Laboratory Markers and Tests
Laboratory tests are very important for diagnosing and managing tumors. Tumor markers like alpha-fetoprotein and human chorionic gonadotropin help diagnose and track treatment. Genetic tests also guide specific treatments.
We use a team approach to diagnose and treat tumors. This includes clinical findings, imaging, and lab results. It helps us give kids with cancer the best care.
Biopsy and Pathological Assessment
Diagnosing childhood cancers starts with a biopsy and pathological assessment. These steps are key to figuring out the cancer type and stage. This info helps doctors decide on the best treatment.
Tissue Sampling Techniques
Biopsy takes a tissue sample from the body for study. In kids’ cancer care, different biopsy methods are used. The choice depends on the tumor’s location and size.
Needle biopsy is used for tumors that are easy to reach. It’s less invasive than surgery. Incisional biopsy removes part of the tumor, while excisional biopsy takes out the whole tumor. This is for small tumors that can be removed fully.
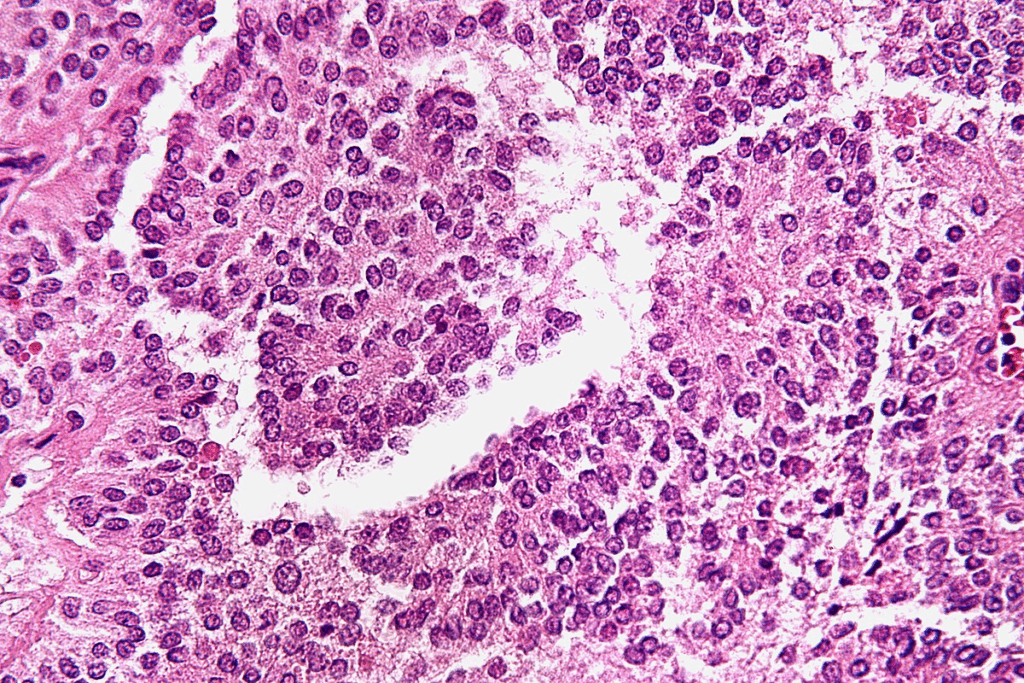
Histopathological Examination
After getting a tissue sample, it’s examined under a microscope. This checks for abnormal cells or tumor signs. It’s key for cancer diagnosis and understanding how aggressive it is.
Pathologists look at the sample to find out the tumor’s type, grade, and other details. They use advanced methods like immunohistochemistry to classify the tumor and find treatment targets.
Molecular and Genetic Analysis
Molecular and genetic tests are also vital in diagnosing and treating pediatric cancers. These tests find specific genetic changes linked to the tumor.
New tools like MARQO help analyze cancer tissues. They give deep insights into tumor genetics and molecular features. This helps in diagnosis and finding new treatments.
By combining biopsy results with pathological and molecular analysis, we get a full picture of each patient’s cancer. This detailed understanding is key to creating personalized treatment plans. It helps improve outcomes in pediatric oncology.
Staging Systems and Risk Stratification
In pediatric oncology, staging systems and risk stratification are key. They help tailor treatments to each patient’s needs. Accurate staging and risk assessment are vital for predicting outcomes and making treatment plans.
Tumor-Specific Staging Protocols
Each type of pediatric cancer has its own staging protocols. For example, neuroblastoma staging looks at how far the tumor has spread. It considers the patient’s age, the tumor’s type, and genetic factors like MYCN amplification.
- Neuroblastoma Staging: The International Neuroblastoma Risk Group (INRG) system is used. It looks at age, tumor type, and genetics.
- Wilms Tumor Staging: The Children’s Oncology Group (COG) system is used. It focuses on how big the tumor is and if it has anaplasia.
- Rhabdomyosarcoma Staging: Staging looks at the tumor’s size, location, and if it has spread.
Prognostic Indicators and Risk Groups
Prognostic indicators help find risk groups in pediatric cancer patients. These include the tumor’s biology, the patient’s age, and how well they respond to treatment.
- Tumor Biology: Genetic traits, like mutations or translocations, greatly affect prognosis.
- Patient Age: Age at diagnosis is very important. Younger patients often have different outcomes than older ones.
- Response to Treatment: How well a patient responds to treatment early on is a big predictor of their outcome.
Impact on Treatment Planning
Staging and risk stratification shape treatment plans. They help doctors decide how intense the treatment should be. This balances how well it works with the risk of long-term side effects.
For instance, low-risk patients might get less intense treatment to reduce side effects. High-risk patients might get more intense treatments, like new therapies or clinical trials.
Accurate staging and risk stratification are key for effective treatment planning in pediatric solid tumors. They help find the best treatment approach. This improves patient outcomes and quality of life.
Multimodal Treatment Strategies
Multimodal treatment strategies have changed the game in pediatric oncology. They bring new hope to kids with solid tumors. The complexity of these cancers needs a mix of treatments for the best results.
Surgical Management Principles
Surgery is key in treating pediatric solid tumors. Complete resection of the tumor is the main goal, if possible, to boost survival chances. We use advanced techniques like minimally invasive surgery to lessen side effects and speed up recovery.
Deciding on surgery depends on the tumor’s location, size, and the child’s health. Sometimes, neoadjuvant chemotherapyis used to make the tumor smaller before surgery.
Radiation Therapy Approaches
Radiation therapy is vital in treating pediatric solid tumors, mainly for tumors that respond well to it. We use intensity-modulated radiation therapy (IMRT) and proton therapy to target the tumor accurately while protecting healthy tissues.
The type of radiation therapy chosen depends on the tumor, its location, and the child’s age. For younger patients, we weigh the long-term effects of radiation on growing tissues carefully.
Chemotherapy Regimens and Protocols
Chemotherapy is a core part of treating pediatric solid tumors. We create personalized chemotherapy regimens based on the tumor and the child’s health.
Our method involves combination chemotherapy, using multiple drugs to attack the tumor from different sides. This approach boosts effectiveness and lowers the chance of resistance.
Novel Targeted Therapies
The introduction of targeted therapies has brought new hope to pediatric solid tumors. These therapies aim at specific molecular targets in tumor growth and spread.
We are dedicated to keeping up with the latest medical research. We incorporate new treatments into our practice to better outcomes for kids with solid tumors.
Conclusion: The Future of Pediatric Solid Tumor Management
Exploring pediatric solid tumors shows us how vital childhood cancer research is. Knowing the different types and their classifications helps us find better treatments. This knowledge is key to saving more lives.
Recent advances in pediatric oncology have greatly improved tumor management. We now use a mix of treatments like surgery, radiation, and chemotherapy. These are chosen based on the patient’s tumor and risk factors.
Looking ahead, more research and better treatments are needed. We must keep learning about these tumors and try new methods. This will help us save more children and give them the best care possible.
FAQ
What is the most common type of solid tumor in children?
Neuroblastoma is the most common solid tumor outside the brain in kids. It makes up a big part of childhood cancercases.
What are the typical characteristics of childhood solid tumors?
Childhood solid tumors are abnormal tissue masses. They can happen in many body parts, like organs and soft tissues. These tumors can be harmless or dangerous and vary based on where they start.
How is neuroblastoma diagnosed and what are its symptoms?
Doctors use CT scans and MRI to find neuroblastoma. They also check urine levels. Symptoms depend on where the tumor is. They might include a big belly, bone pain, or problems with nerves.
What is Wilms tumor, and how is it treated?
Wilms tumor is a kidney cancer in kids. Treatment includes surgery, chemotherapy, and sometimes radiation. The goal is to remove the tumor and help the child live a long life.
What are the different types of brain tumors that occur in children?
Kids can get many brain tumors, like medulloblastoma and astrocytomas. Each type needs its own treatment plan because of its unique features.
How are pediatric solid tumors staged, and what is the significance of staging?
Staging helps classify tumors by how far they’ve spread. Knowing the stage is key for planning treatment and predicting outcomes. It helps doctors talk about a child’s cancer clearly.
What are the treatment options for rhabdomyosarcoma and other soft tissue sarcomas?
Rhabdomyosarcoma and other soft tissue tumors are treated with surgery, chemotherapy, and radiation. The best plan depends on the tumor type, stage, and the child’s health.
What is the role of biopsy in diagnosing childhood cancers?
Biopsy is very important in finding out what kind of cancer a child has. It lets doctors look at tumor tissue to decide the best treatment.
What are the current advancements in the treatment of pediatric solid tumors?
New treatments like targeted therapies and better chemotherapy are helping kids with solid tumors. Surgery has also improved, leading to better survival rates.
How do genetic factors contribute to the development of pediatric solid tumors?
Genetic changes can cause many childhood cancers, including neuroblastoma and Wilms tumor. Knowing these genetic factors helps doctors diagnose and treat the cancer better.
Reference
- Tian, J., et al. (2023). Advances in the treatment of solid tumors in children and adolescents. Pediatric Oncology Reports. https://pmc.ncbi.nlm.nih.gov/articles/PMC10686120/