Last Updated on December 1, 2025 by Bilal Hasdemir

Wilms tumor is a rare kidney cancer that affects about 4-10 kids per million each year. The prognosis for Wilms tumor has gotten much better over time.
Today, more than 90% of kids with early-stage Wilms tumor survive. This news brings hope to families dealing with this disease. Knowing about Wilms tumor treatment is key to better results.
Looking into Wilms tumor shows how vital early detection and good treatment plans are. They help a lot in improving wilms tumor prognosis.
Learn about the prognosis and high survival rate for wilm’s tumor and its modern treatment protocols.
Key Takeaways
- Wilms tumor is a rare childhood kidney cancer.
- The survival rate for Wilms tumor has improved significantly.
- Early-stage Wilms tumor has a survival rate exceeding 90%.
- Understanding treatment options is key to improving outcomes.
- Early detection is vital for better prognosis.
What is Wilms Tumor?
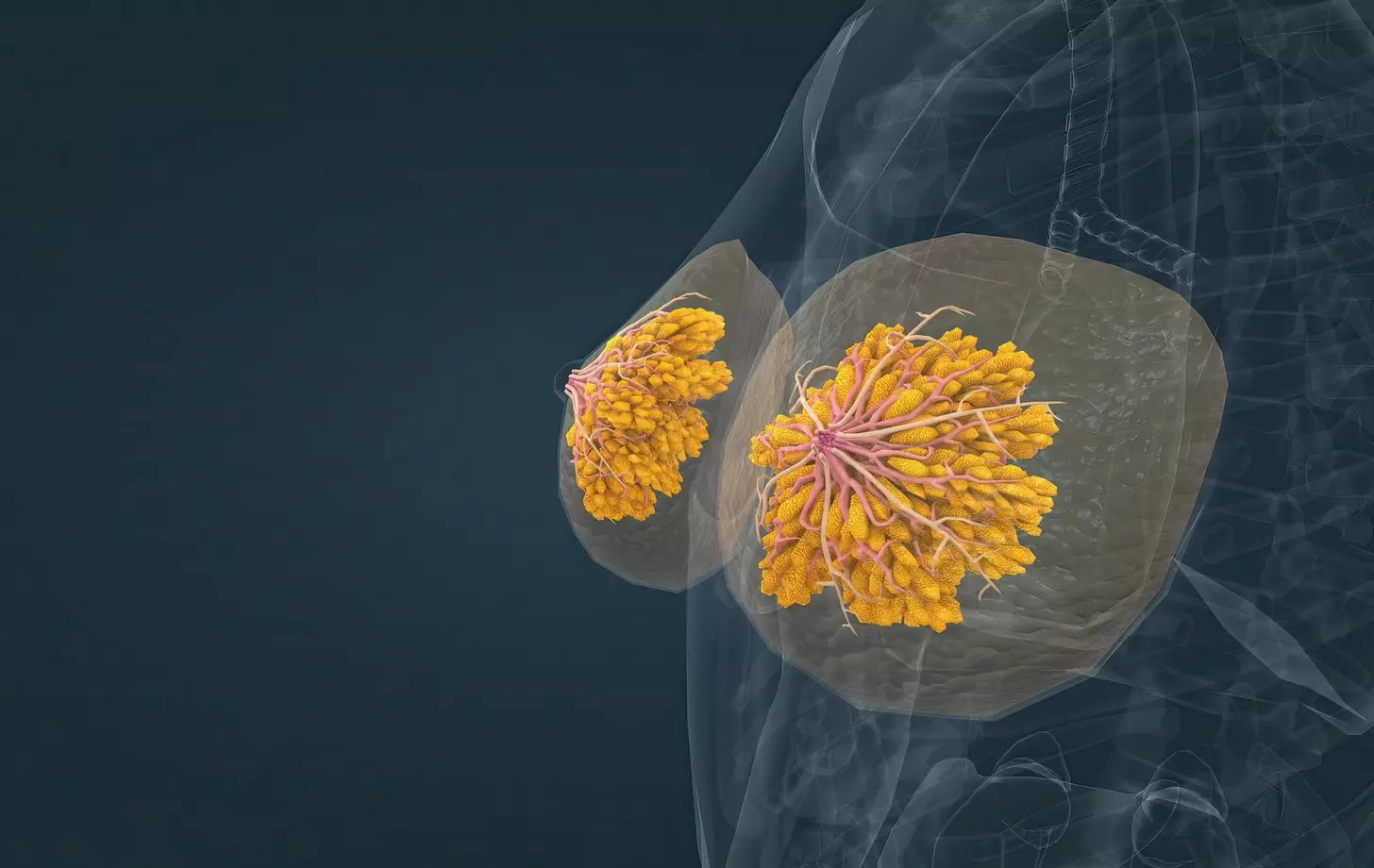
Wilms tumor, also known as nephroblastoma, is a cancer that starts in the kidneys. It mainly affects young children. A tumor forms in one or both kidneys, which can spread to other parts of the body if not treated quickly.
Definition and Medical Classification
Wilms tumor is a type of renal cancer that starts in the metanephric blastema. This is the cells that form the kidney. It’s called pediatric kidney cancer because it mostly affects kids. The medical classification of Wilms tumor involves understanding its histology.
Doctors classify Wilms tumor as either favorable or unfavorable based on its cells. Favorable histology means the tumor has a better chance of recovery. Unfavorable histology means the tumor is more aggressive and needs more intense treatment.
“The classification of Wilms tumor into favorable and unfavorable histology has significantly improved the prognostication and treatment stratification for patients.” –
A leading pediatric oncologist
Prevalence in Children
Wilms tumor is the most common kidney cancer in kids, making up about 90% of cases. It usually affects children between 3 and 4 years old. It can happen at any age, but it’s slightly more common in girls than boys.
| Age Group | Incidence Rate |
| 0-4 years | 8.1 per million |
| 5-9 years | 2.2 per million |
| 10-14 years | 0.7 per million |
Knowing about Wilms tumor’s prevalence and characteristics is key for early detection and treatment. We’ll look into its causes, symptoms, and treatment options in the next sections.
Understanding Wilm’s Tumor: The Basics

Learning about Wilms tumor is key for patients and their families. We will look into how it develops and how it differs from other kidney cancers.
How Wilms Tumor Develops
Wilms tumor starts with genetic changes in kidney cells. These changes cause cells to grow out of control, forming a tumor. The exact reason for these changes is not always known, but they often happen during fetal development.
Genetic syndromes like WAGR syndrome and Denys-Drash syndrome are linked to Wilms tumor. These syndromes show how genetics play a role in the tumor’s development.
Difference Between Wilms Tumor and Other Kidney Cancers
Wilms tumor is different from other kidney cancers, like renal cell carcinoma, which affects adults more. Wilms tumor involves immature kidney cells and is mainly found in children.
Unlike renal cell carcinoma, Wilms tumor is treated with surgery, chemotherapy, and sometimes radiation. Children often respond better to these treatments because of the tumor’s nature.
Knowing the differences between kidney cancers is important for the right treatment. Focusing on Wilms tumor’s unique traits helps doctors provide better care and improve patient outcomes.
Causes and Risk Factors
The exact cause of Wilms tumor is not known. But, research has found some genetic and environmental risk factors. Knowing these factors helps us understand the risk and how to lower it.
Genetic Predisposition
Genetics play a big role in Wilms tumor. Some genetic syndromes raise the risk. These include:
- WAGR syndrome (Wilms tumor, Aniridia, Genitourinary anomalies, and mental Retardation)
- Beckwith-Wiedemann syndrome
- Denys-Drash syndrome
These syndromes have genes linked to kidney development. Kids with these syndromes need regular checks for Wilms tumor.
Environmental Factors
Environmental factors might also play a part. Some studies hint at a link between toxins and Wilms tumor risk. But, more research is needed to confirm this.
We’ve made a table to summarize what we know about risk factors:
| Risk Factor | Description | Impact on Wilms Tumor Risk |
| Genetic Syndromes | WAGR, Beckwith-Wiedemann, Denys-Drash syndromes | Increased risk due to genetic mutations |
| Family History | Presence of Wilms tumor in family members | Potential increase in risk, more so with first-degree relatives |
| Environmental Toxins | Exposure to certain chemicals and pollutants | Possible increase in risk, more research needed |
Knowing about these risk factors helps in early detection and management of Wilms tumor. Regular check-ups are advised for kids with genetic predispositions.
Signs and Symptoms
It’s important to know the signs of Wilms tumor to get help quickly. This kidney cancer mainly hits kids. It shows in different ways that need fast action.
Common Physical Manifestations
The signs of Wilms tumor include:
- Abdominal swelling or mass
- Abdominal pain
- Hematuria (blood in the urine)
- Hypertension (high blood pressure)
- Fever
- Loss of appetite
- Weight loss
These signs mean the disease might be getting worse. Getting help early is key to better treatment.
When to Seek Medical Attention
If your child shows any of these signs, see a doctor right away:
| Symptom | Description | Action |
| Abdominal Swelling | Noticeable swelling or enlargement of the abdomen | Consult a pediatrician |
| Hematuria | Blood visible in the urine | Seek immediate medical attention |
| Abdominal Pain | Persistent or severe pain in the abdominal region | Schedule an urgent appointment |
Knowing these signs can help with Wilms tumor diagnosis and treatment. If you think something’s wrong, talk to a doctor.
Diagnosis Process
Diagnosing Wilms tumor is a detailed process. It involves imaging studies and looking at tissue samples. We use many tools to find and understand the tumor accurately.
Initial Screening Methods
When a child shows signs of Wilms tumor, we start with non-invasive tests. Ultrasound is often the first tool we use. It shows the tumor’s size, where it is, and if it has spread.
Ultrasound is great because it’s easy to get and doesn’t use harmful radiation. But, we might need more tests for a clearer picture.
Confirmatory Tests
To confirm the diagnosis, we use more detailed tests. Computed Tomography (CT) scans give us detailed images of the tumor and if it has spread. Magnetic Resonance Imaging (MRI) helps us see how big the tumor is and its relation to important areas.
After these tests, we do a biopsy to confirm the diagnosis. Looking at the biopsy helps us know the tumor’s type and what it’s like. This is key for planning treatment.
| Diagnostic Test | Purpose | Key Benefits |
| Ultrasound | Initial assessment of tumor size and location | Non-invasive, no radiation exposure |
| CT Scan | Detailed imaging of tumor and possible spread | High-resolution images, helps in staging |
| MRI | Further check of tumor size and how it affects nearby areas | No radiation, excellent soft tissue detail |
| Biopsy | Confirmation of tumor type and characteristics | Definitive diagnosis, guides treatment planning |
Getting the diagnosis right is key to making a good treatment plan. We make sure all tests are done carefully. This helps us understand the tumor well.
Wilms Tumor Staging System
The Wilms tumor staging system is key in figuring out how far the tumor has spread. It guides doctors in choosing the right treatment. This system helps doctors understand how serious the disease is and plan the best treatment.
Stage I through V Explained
The disease is divided into five stages, from Stage I to Stage V. These stages are based on how far the tumor has spread and if it has touched nearby tissues.
- Stage I: The tumor is only in the kidney and is fully removed.
- Stage II: The tumor has grown beyond the kidney but is fully removed.
- Stage III: The tumor can’t be fully removed or has spread to lymph nodes in the abdomen.
- Stage IV: The tumor has spread to distant places like the lungs, liver, or brain.
- Stage V: The tumor is in both kidneys.
Knowing these stages is key to understanding the prognosis and picking the best treatment.
Importance of Accurate Staging
Getting the right stage for Wilms tumor is vital. It makes sure patients get the best treatment for their case. It helps find out who needs stronger treatment and who can avoid harmful side effects.
Accurate staging of Wilms tumor leads to better treatment results. It also improves the quality of life for patients.
Treatment Approaches
The treatment for Wilms tumor has changed a lot. Now, we use many different ways to fight this childhood cancer. Each child gets a treatment plan that fits their needs best.
Surgical Interventions
Surgery is very important in treating Wilms tumor. Our goal is to take out the tumor and sometimes the whole kidney. We look at the tumor’s stage and type to decide how to operate.
Surgical options may include:
- Radical nephrectomy (removal of the kidney)
- Partial nephrectomy (removal of the tumor while preserving kidney function)
- Lymph node sampling to assess the spread of the disease
Chemotherapy Protocols
Chemotherapy is key in treating Wilms tumor. It helps shrink the tumor before surgery or kills any cancer cells left after surgery. We adjust the chemotherapy based on the tumor’s stage, type, and the child’s health.
Common chemotherapy agents used include:
| Drug | Role |
| Vincristine | Interferes with cell division |
| Dactinomycin | Binds to DNA, inhibiting tumor growth |
| Doxorubicin | Intercalates DNA strands, preventing cancer cell proliferation |
Radiation Therapy Options
In some cases, we use radiation therapy. This is for tumors that are harder to treat or have spread. We use new radiation methods to protect healthy tissues.
The decision to use radiation therapy is based on:
- The stage and extent of the disease
- The child’s age and overall health
- The tumor’s response to initial chemotherapy
Survival Rates and Prognosis
It’s important to know about survival rates and prognosis for Wilms Tumor. This knowledge helps patients and their families. The survival rate for Wilms Tumor has greatly improved. Now, over 90% of early-stage cases survive.
Overall Survival Statistics
The overall survival statistics for Wilms Tumor have greatly improved. Studies show that more children with Wilms Tumor are surviving. This is due to better treatments and early detection.
“The five-year survival rate for children with Wilms Tumor is now over 90% in many countries,” a medical report states. This shows a positive trend in fighting this disease.
Factors Affecting Prognosis
Several factors affect the prognosis of Wilms Tumor. These include the stage at diagnosis, the patient’s age, and genetic mutations. Being diagnosed early greatly improves the chances of survival.
- Stage at diagnosis
- Age of the patient
- Presence of genetic mutations
- Response to initial treatment
The prognosis also depends on how well the tumor responds to treatment. Patients who do well with chemotherapy and surgery have a better outlook.
“Advances in genetic research and personalized medicine are expected to further improve the survival rates and prognosis for Wilms Tumor patients,” said a leading oncologist.
We keep learning more about Wilms Tumor prognosis. Our goal is to give the best care to our patients.
Stage 4 Wilms Tumor Life Expectancy
Knowing the life expectancy for stage 4 Wilms tumor patients is key for families. This stage means the cancer has spread to other parts of the body, like the lungs or liver. It’s a tough diagnosis to face.
Advanced Stage Challenges
Dealing with stage 4 Wilms tumor is tough. The cancer’s spread makes treatment harder. Treatment often includes surgery, chemotherapy, and radiation, based on the patient’s needs.
One big challenge is making sure treatment hits the cancer cells right. It’s vital to have a team of specialists to help with this.
Treatment Success Rates
Despite the hurdles, treatment for stage 4 Wilms tumor is getting better. Success depends on the patient’s age, health, and how well they respond to treatment. New studies show good results with intense chemotherapy and radiation.
Survival rates for kids with stage 4 Wilms tumor are going up. It’s important for families to work with their healthcare team to understand the prognosis and plan treatment.
By knowing what affects life expectancy and treatment success, families can better prepare. Our aim is to give full care and support to improve outcomes for kids with stage 4 Wilms tumor.
Recent Advances in Wilms Tumor Treatment
Wilms tumor treatment has seen big changes with new targeted and immunotherapies. These new methods are changing how we treat this disease. They offer better results and fewer side effects.
Innovative Therapeutic Approaches
New targeted therapies focus on specific parts of the tumor. They aim to be more precise, harming fewer healthy cells and causing less side effects.
Immunotherapy is also a promising area. It uses the body’s immune system to fight cancer. Agents like checkpoint inhibitors are being tested to see if they can help the body fight cancer cells better.
- Targeted therapy agents that inhibit specific pathways involved in Wilms tumor progression.
- Immunotherapies that stimulate the immune system to recognize and attack cancer cells.
- Combination regimens that integrate traditional chemotherapy with newer targeted therapies.
Impact on Survival Outcomes
These new treatments are making a big difference in survival rates for Wilms tumor patients. They offer more effective and less harmful options. This means better survival rates and a better quality of life for survivors.
| Treatment Approach | Impact on Survival | Key Benefits |
| Targeted Therapies | Improved overall survival rates | Reduced side effects, precision medicine |
| Immunotherapies | Enhanced response rates | Harnesses the immune system, potentially durable responses |
| Combination Regimens | Better disease control | Synergistic effects, improved efficacy |
As we keep moving forward in Wilms tumor treatment, it’s key to keep researching and innovating. This way, we can make sure patients get the best care possible.
Long-term Effects and Follow-up Care
Long-term care is key for Wilms tumor survivors. It helps manage treatment side effects. As treatments get better, more survivors are living longer. This means we need to focus on their physical and mental health.
Physical Health Monitoring
Survivors may face health issues like kidney problems and scoliosis. Regular check-ups help catch these problems early. A good follow-up plan includes:
- Regular visits to the doctor to check overall health
- Tests to find late effects of treatment
- Advice on healthy living to prevent future problems
Key aspects of physical health monitoring include:
- Checking kidney function for damage
- Screening for scoliosis and other bone issues
- Watching for secondary cancers
Psychological Support and Quality of Life
Survivors may also deal with mental health issues like anxiety and depression. It’s vital to offer psychological support. A team approach is best, including:
- Therapy to help with emotional and mental health
- Support groups for sharing experiences
- Help for families to understand and support survivors
By caring for both physical and mental health, we can greatly improve survivors’ lives.
Success Stories and Survivor Experiences
Surviving Wilms tumor is a remarkable achievement. The stories of these survivors are truly inspiring. We get to share some of these journeys, showing the courage and resilience of Wilms tumor survivors.
Notable Survival Cases
Many people have overcome Wilms tumor, each with their own story. For example, a child diagnosed at 4 is now a thriving teenager. He participates in sports and lives a normal life. These stories show how far medical care has come and the strength of these young survivors.
Emily was diagnosed with Wilms tumor at 6. After surgery and chemotherapy, she fully recovered. Now, she advocates for childhood cancer awareness, helping others facing similar challenges.
Life After Wilms Tumor
Life after Wilms tumor means ongoing medical check-ups. Survivors often need to watch for long-term effects, like kidney issues or secondary cancers. Despite these challenges, many lead active, fulfilling lives.
To understand the journey of Wilms tumor survivors, let’s look at some statistics and outcomes in the table below:
| Survival Aspect | Statistic | Implication |
| Overall Survival Rate | 85-90% | High survival rates reflect advancements in treatment protocols. |
| Long-term Health Issues | 20-30% | Some survivors experience long-term health issues, necessitating ongoing care. |
| Quality of Life | Majority report good QOL | Most survivors enjoy a good quality of life, participating in various activities. |
These statistics show the positive outcomes for many Wilms tumor survivors. They also highlight the need for continued support and medical care.
In conclusion, the stories of Wilms tumor survivors remind us of our ability to overcome challenges. By sharing these experiences, we aim to inspire and inform others about living with and overcoming Wilms tumor.
Conclusion
Wilms tumor is a complex condition that needs careful care and attention. Finding it early and treating it well are key to better survival chances and outcomes.We’ve looked at many parts of Wilms tumor, like what it is and how it’s treated today. Knowing its causes, signs, and symptoms helps patients and families deal with the diagnosis better.In short, treating Wilms tumor requires a team effort. By focusing on early detection, effective treatment, and support, we can help patients live better lives. This summary wraps up the importance of ongoing research and new treatments in fighting Wilms tumor.
FAQ
What is Wilms tumor?
Wilms tumor, also known as nephroblastoma, is a rare kidney cancer in kids. It needs careful treatment and care.
What are the common symptoms of Wilms tumor?
Signs include an abdomen lump, pain, and fever. Seeing a doctor is key if you notice these.
How is Wilms tumor diagnosed?
First, doctors use ultrasound and CT scans. Then, a biopsy confirms it.
What is the Wilms tumor staging system?
It shows how far the cancer has spread. Stages range from I to V, with I being the least severe.
What are the treatment options for Wilms tumor?
Treatments include surgery, chemotherapy, and radiation. The choice depends on the tumor’s stage and type.
What is the survival rate for Wilms tumor?
Most kids with Wilms tumor are cured. Survival rates depend on the tumor’s stage and type.
What is the life expectancy for stage 4 Wilms tumor?
Stage 4 is advanced. Life expectancy varies based on treatment response and other factors. Recent treatments have improved outcomes.
What are the long-term effects of Wilms tumor treatment?
Survivors may face health and mental challenges. Ongoing care is vital to manage these effects.
How can I support a child with Wilms tumor?
Emotional support and access to care are key. This includes health checks and mental health support.
What are the recent advances in Wilms tumor treatment?
New treatments like targeted and immunotherapy have boosted survival rates.
Can Wilms tumor be prevented?
Prevention is not guaranteed. But knowing risk factors can help spot high-risk kids.
References
- Children’s Oncology Group. (2024). Wilms Tumor and Other Childhood Kidney Tumors Treatment (PDQ®)–Health Professional Version. National Cancer Institute. https://www.cancer.gov/types/kidney/hp/wilms-treatment-pdq
- Ehrlich, P. F., Ferrer, F. A., Ritchey, M. L., et al. (2022). Evidence-based surgical guidelines for treating children with Wilms tumour. Pediatric Blood & Cancer, 69(12), e30135. https://pubmed.ncbi.nlm.nih.gov/35929184/
- Theilen, T. M., Keenan, H. M., & Chintagumpala, M. (2022). Multidisciplinary treatment strategies for Wilms tumor. Frontiers in Pediatrics, 10, 852185. https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2022.852185/full