Last Updated on December 1, 2025 by Bilal Hasdemir

Neuroblastoma is a cancer that starts in nerve tissue. It’s the most common solid tumor outside the brain in kids. It makes up around 6% of all childhood cancers. It often grows in the adrenal glands but can also appear in other parts of the abdomen Pediatric Abdominal Tumor.
Neuroblastoma has a big impact on research into childhood cancer. Studies are working hard to better understand and treat it. Knowing about neuroblastoma is key to moving forward in childhood cancer research.
Key Takeaways
- Neuroblastoma is the most common extracranial solid tumor in children.
- It mainly affects the adrenal glands and other areas in the abdomen.
- Research is ongoing to find better ways to diagnose and treat it.
- Understanding neuroblastoma is vital for advancing childhood cancer research.
- Neuroblastoma makes up about 6% of all childhood cancers.
Understanding Pediatric Abdominal Tumors: An Overview

Childhood abdominal tumors are a big challenge in pediatric oncology. We need to know a lot about them to help kids. It’s important to understand how common they are and why they matter for better treatment.
Prevalence and Significance in Childhood Cancer
Pediatric abdominal tumors are common outside the brain in kids. Neuroblastoma is the most common one. These tumors can really affect a child’s life and chances of survival. So, finding them early and treating them well is key.
Studies show that how often these tumors happen changes with age. For example, neuroblastoma often shows up in kids under five.
| Type of Tumor | Typical Age Group | Relative Frequency |
| Neuroblastoma | 0-5 years | High |
| Wilms Tumor | 3-6 years | Moderate |
| Hepatoblastoma | 0-3 years | Low to Moderate |
Classification of Abdominal Masses in Children
We sort abdominal masses in kids by where they come from, what they look like under a microscope, and how they act. The main groups are:
- Neurogenic tumors (e.g., neuroblastoma, ganglioneuroma)
- Renal tumors (e.g., Wilms tumor)
- Hepatic tumors (e.g., hepatoblastoma, hepatocellular carcinoma)
- Lymphatic and other rare tumors
Knowing the exact type of tumor is very important. It helps doctors guess how well a child will do and what treatment to use.
By learning about the different kinds of pediatric abdominal tumors, doctors can make better plans to help kids. This can lead to better results for kids with these tumors.
Neuroblastoma: The Most Common Pediatric Abdominal Tumor
Neuroblastoma poses a significant challenge in terms of diagnosis and treatment. It’s the most common tumor in kids’ bellies. We’ll look into how it starts, grows, and where it usually shows up.
Origin and Development of Neuroblastoma
Neuroblastoma comes from cells called neural crest cells. These cells are the early stages of the sympathetic nervous system. The developmental patterns of neuroblastoma are complex. They involve changes in genes and molecules that cause tumors.
The tumor can start anywhere in the sympathetic nervous system, from the neck to the pelvis. But most often, it happens in the belly. This makes it a big worry for kids’ tumors in the abdomen.
Anatomical Distribution and Common Sites
Neuroblastoma can show up in different places, but it often hits the adrenal glands. These glands sit on top of the kidneys. A tumor in the belly can cause swelling, pain, and discomfort.
The places where neuroblastoma usually appears are:
- Adrenal glands: Most common site
- Paravertebral sympathetic ganglia: Frequent site
- Other sites: Neck, chest, pelvis
Knowing where neuroblastoma often shows up is key for finding it right and planning treatment. We’ll keep looking into its causes and genetics in the next parts.
Epidemiology of Neuroblastoma
Understanding neuroblastoma’s spread is key to better treatments. We look at how old kids are when they get it, how often it happens, and where. This helps us learn more about the disease and how to fight it.
Age Distribution and Incidence Rates
Most kids with neuroblastoma are under five. It happens in about 10 out of a million kids each year. Knowing how old a child is helps doctors figure out the best treatment.
Infants get it more often because it can sometimes go away on its own. Below is a table showing how age affects who gets neuroblastoma and how often.
| Age Group | Incidence Rate (per million) |
| <1 year | 30-40 |
| 1-4 years | 10-20 |
| 5-9 years | 5-10 |
| 10+ years | <5 |
Geographic and Demographic Variations
Neuroblastoma is not the same everywhere. It’s more common in North America and Europe than in other places. This shows that where you live can affect your chances of getting it.
Who you are can also change your chances of getting neuroblastoma. Things like your race and how much money your family makes can play a part. Studying these differences helps us find new ways to help kids.
By knowing more about neuroblastoma, we can make treatments better. This means more kids can survive and live healthier lives. It’s all thanks to research and new ways to diagnose and treat the disease.
Genetic and Molecular Basis of Neuroblastoma
Understanding the genetic basis of neuroblastoma is key for effective pediatric treatment strategies. Recent medical research insights have greatly improved our knowledge of this complex disease.
Key Genetic Alterations and Mutations
Neuroblastoma has specific cancer genetic variations and mutations that are vital for tumor growth. Key changes include amplifications, deletions, and mutations in genes that control cell growth and survival. For example, MYCN amplificationis linked to high-risk neuroblastoma.
Identifying these genetic changes helps us understand neuroblastoma’s pathogenesis. It also guides the creation of cancer genetic markers for diagnosis and prognosis. These insights are essential for developing targeted therapies that tackle the disease’s molecular roots.
Molecular Pathways in Tumor Development
Neuroblastoma’s development involves complex molecular pathways. When these pathways are disrupted, they lead to tumor growth and progression. Knowing these molecular pathways is vital for finding new treatments.
Research shows that cell proliferation, differentiation, and apoptosis pathways are key in neuroblastoma. For instance, changes in the ALK gene and the MAPK signaling pathway are involved. Uncovering these pathways offers valuable medical research insights for innovative treatments.
Clinical Presentation and Symptoms
It’s key to know the signs of neuroblastoma early for better treatment. This cancer can show up differently, based on where the tumor is and the child’s age.
Common Presenting Signs in Infants and Children
Children with neuroblastoma might show various symptoms. Some common ones are:
- Abdominal mass or swelling
- Proptosis (bulging eyes)
- Periorbital ecchymoses (bruising around the eyes)
- Bone pain or limping
- Spinal cord compression symptoms, such as weakness or paralysis
These signs can be vague, so doctors must think of neuroblastoma when diagnosing.
Paraneoplastic Syndromes Associated with Neuroblastoma
Neuroblastoma can also lead to rare but serious conditions. These are caused by substances the tumor makes. For example:
- Opsoclonus-myoclonus syndrome (OMS), with rapid eye movements and muscle twitches
- Ceroid-induced neurotoxicity
Spotting these conditions is important. They can be the first sign of neuroblastoma and need special care.
Screening and Early Detection of Pediatric Abdominal Tumor
Screening for pediatric abdominal tumors is key in treating childhood cancer. There’s a debate on the best methods. Early detection through screening can greatly improve treatment results for kids with these tumors.
Current Screening Recommendations and Controversies
Screening for pediatric abdominal tumors, like neuroblastoma, uses imaging and biomarkers. But, there’s a debate on mass screening. This is because of worries about medical screening sensitivity and false positives.
Some research shows mass screening for neuroblastoma might find tumors that wouldn’t cause symptoms. This could lead to unnecessary treatment and harm. Yet, targeted screening for high-risk groups might help detect cancer early and improve survival rates.
Risk-Based Screening Approaches
Risk-based screening focuses on kids at high risk for abdominal tumors. This includes those with genetic predispositions or family history. This method makes medical screening protocols more effective by targeting those most likely to benefit.
For example, kids with a family history of neuroblastoma or certain genetic mutations might get regular screenings. This helps in childhood cancer treatment planning and research into tumor genetics.
Using a risk-based screening strategy helps balance early detection benefits with screening risks and costs. This approach is vital for improving cancer early detection and outcomes for kids with abdominal tumors.
Diagnostic Approaches for Neuroblastoma
Healthcare professionals use many tools to diagnose neuroblastoma. They use imaging studies and lab tests to find out about the tumor. This helps them understand how big it is and where it is.
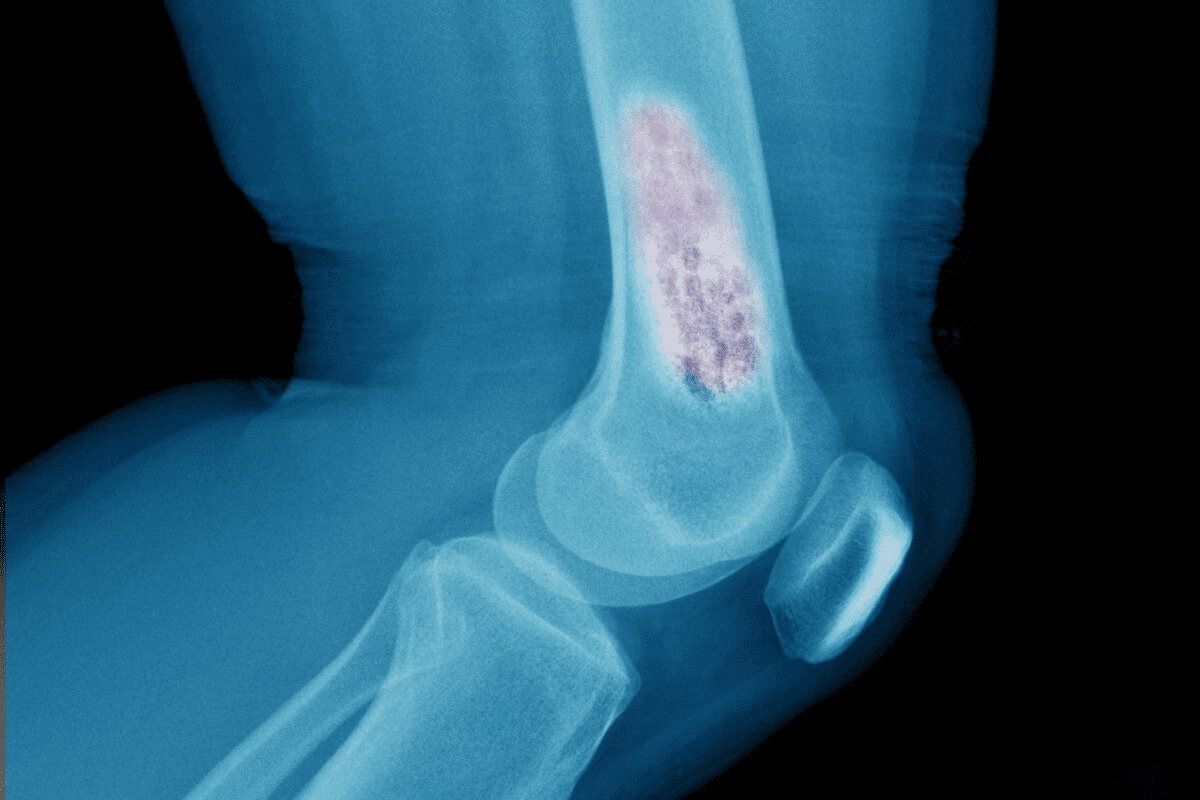
Imaging Techniques and Their Applications
Imaging is key in diagnosing and staging neuroblastoma. Different imaging methods are used, each with its own benefits.
- Ultrasound: It’s often the first test used, mainly in kids. It’s safe and doesn’t use radiation.
- Computed Tomography (CT) Scan: It gives detailed pictures of the tumor. This helps doctors see its size and where it is.
- Magnetic Resonance Imaging (MRI): It shows detailed images without radiation. This is great for seeing how far the tumor has spread.
- Metaiodobenzylguanidine (MIBG) Scan: This scan is special because it finds neuroblastoma cells well. It’s very useful for this type of cancer.
Laboratory Tests and Biomarkers
Laboratory tests are vital for diagnosing neuroblastoma. They help understand the tumor’s biology. Key tests include:
- Biochemical Markers: High levels of certain chemicals in urine or blood point to neuroblastoma.
- Genetic Testing: Looking at tumor DNA for specific changes helps predict the cancer’s behavior.
- Histopathological Examination: Examining tumor tissue from a biopsy is key. It confirms the diagnosis and looks at the tumor’s features.
By using imaging and lab tests together, we get a full picture of neuroblastoma. This helps doctors make the right treatment plan.
Biopsy and Histopathological Evaluation
Getting the right treatment for neuroblastoma starts with a precise biopsy and histopathological evaluation. A biopsy lets us look at the tumor tissue directly. This gives us clues about its nature and how it might behave.
Biopsy Techniques and Considerations
There are many biopsy methods for diagnosing neuroblastoma, each with its own benefits and challenges. Fine-needle aspiration biopsy is a gentle method that can give a quick diagnosis. But core needle biopsy is usually better because it gives more tissue for detailed study.
Choosing the right biopsy method depends on the tumor’s location, size, and the patient’s health. We must think carefully about these factors to make sure the biopsy is done safely and effectively.
Histological Classification and Grading
Looking closely at the biopsy sample is key to diagnosing neuroblastoma and predicting its outcome. The International Neuroblastoma Pathology Classification (INPC) helps us sort neuroblastoma into different types based on its appearance under the microscope.
| Histological Feature | Description | Prognostic Implication |
| Mitotic Rate | Number of mitoses per high-power field | High mitotic rate indicates a more aggressive tumor |
| Cellular Differentiation | Degree of cellular maturation | Poorly differentiated tumors have a worse prognosis |
| Stroma Composition | Presence and amount of stromal tissue | Stroma-rich tumors may have a better prognosis |
Understanding the histological classification and grading of neuroblastoma helps us plan treatment better. By studying the tumor’s microscopic features, we can tailor our treatment to match the tumor’s behavior.
Accurate histopathological evaluation is essential for giving patients the right treatment for their neuroblastoma. By combining biopsy results with other diagnostic tools, we can create a treatment plan that meets each patient’s unique needs.
Staging Systems for Neuroblastoma
Staging neuroblastoma is key to knowing how far the disease has spread. It helps doctors plan the best treatment. Accurate staging is vital for predicting outcomes and creating effective treatment plans.
Two main staging systems are used: the International Neuroblastoma Staging System (INSS) and the International Neuroblastoma Risk Group (INRG) Classification. Knowing these systems is important for pediatric oncology insightsand medical research insights.
International Neuroblastoma Staging System (INSS)
The INSS classifies neuroblastoma based on how far the tumor has spread and if it can be removed surgically. It divides the disease into stages, from local to widespread.
| Stage | Description |
| 1 | Localized tumor with complete gross excision |
| 2A | Localized tumor with incomplete gross excision |
| 2B | Localized tumor with or without complete gross excision, with ipsilateral lymph node involvement |
| 3 | Unresectable unilateral tumor infiltrating across the midline or localized unilateral tumor with contralateral lymph node involvement |
| 4 | Any primary tumor with dissemination to distant lymph nodes, bone, bone marrow, liver, or other organs |
| 4S | Localized primary tumor with dissemination limited to skin, liver, or bone marrow in infants |
International Neuroblastoma Risk Group (INRG) Classification
The INRG Classification is a newer system. It aims to better predict outcomes by adding more factors, like imaging results. It stages neuroblastoma based on imaging-defined risk factors.
The INRG Classification puts patients into risk groups. This helps doctors tailor treatments to each patient’s risk. It leads to more personalized and effective care.
Understanding and using these staging systems is key to better patient outcomes in neuroblastoma. Accurate staging helps doctors plan treatments that improve survival and quality of life.
Risk Stratification and Prognostic Factors
Risk stratification and prognostic factors are key in treating neuroblastoma in kids. They help doctors predict how the disease will progress. This way, they can create treatment plans that fit each child’s needs.
Age-Related Prognostic Implications
Age at diagnosis is a big factor in neuroblastoma. Babies under one usually do better than older kids. We’ll look at how age affects treatment and what it means for risk stratification.
Age Distribution and Prognosis
| Age Group | Prognosis | Typical Treatment Approach |
| Infants ( | Favorable | Observation or reduced-intensity treatment |
| Children (1-5 years) | Variable | Standard chemotherapy and surgery |
| Older Children (>5 years) | Poor | Aggressive chemotherapy and intensive therapy |
Biological and Genetic Prognostic Markers
Biological and genetic factors are very important in neuroblastoma. We’ll talk about MYCN amplification, tumor ploidy, and genetic changes. These factors help decide treatment.
Knowing these factors helps doctors tailor treatments better. By using age and genetic markers, we can make treatments more effective. This improves outcomes for kids and helps in finding better ways to treat neuroblastoma.
Treatment Strategies for Neuroblastoma
Neuroblastoma treatment uses many methods to help patients. It’s a big part of research into childhood cancer. Finding the best ways to treat it is key.
Surgical Approaches and Considerations
Surgery is very important for treating neuroblastoma, mainly for tumors that are in one place. Complete resection is the main goal. But, it’s hard because of where the tumor is and how close it is to important parts of the body.
We look at the tumor’s size, where it is, and the patient’s health when planning surgery.
“Surgery is a cornerstone in the treatment of neuroblastoma, often leading to a cure for those with localized disease.” –
A leading pediatric oncologist
Chemotherapy Protocols and Regimens
Chemotherapy is a big part of treating neuroblastoma, mainly for those with high-risk or spread-out disease. Different treatments are used, like cyclophosphamide, doxorubicin, and cisplatin. The treatment plan depends on how high the risk is and how well the patient responds.
- Chemotherapy plans are made for each patient based on their risk level.
- Using more than one treatment at a time is often better than one alone.
- It’s important to watch how the patient is doing and change the treatment if needed.
Radiation Therapy Applications
Radiation therapy is used for neuroblastoma, mainly for those at high risk or with leftover tumor after surgery. Intensity-modulated radiation therapy (IMRT) and proton therapy are new ways to target the tumor well and protect other areas.
Studies show that “Radiation therapy is key for treating high-risk neuroblastoma. It helps control the tumor better and might improve survival chances.” We keep working to make radiation therapy safer and more effective.
Advanced and Emerging Therapies
New hope is coming for kids with neuroblastoma, a common tumor. Medical research is moving fast, bringing new treatments to help patients.
Immunotherapy and Targeted Biological Agents
Immunotherapy is showing promise in fighting neuroblastoma. It uses the immune system to attack cancer cells. Monoclonal antibodies and checkpoint inhibitors are being studied for their benefits.
Targeted biological agents are also showing great promise. They aim at specific genetic markers in neuroblastoma. ALK inhibitors and MYCN-targeting therapies are being looked into.
Stem Cell Transplantation and MIBG Therapy
Stem cell transplantation is a new therapy for neuroblastoma. It uses high-dose chemotherapy and stem cells to rebuild the bone marrow. Autologous stem cell transplantation is common, using the patient’s own stem cells.
MIBG (Metaiodobenzylguanidine) therapy targets neuroblastoma cells with radioactive MIBG. It’s helpful for high-risk or resistant cases.
| Therapy Type | Description | Potential Benefits |
| Immunotherapy | Utilizes the immune system to fight cancer | Targeted approach with potentially fewer side effects |
| Targeted Biological Agents | Targets specific genetic markers of neuroblastoma | Personalized treatment approach |
| Stem Cell Transplantation | High-dose chemotherapy followed by stem cell infusion | Effective for high-risk or refractory neuroblastoma |
| MIBG Therapy | Radioactive MIBG targets neuroblastoma cells | Selective destruction of cancer cells |
These new therapies are changing how we treat neuroblastoma. They use the latest research and genetic markers to improve treatment for kids.
Multidisciplinary Care Approaches
Managing neuroblastoma needs a team effort. A group of healthcare experts work together. They aim to give the best care to kids with this disease.
Pediatric Oncology Team Composition
A team for pediatric oncology has many specialists. They are key in diagnosing, treating, and managing neuroblastoma. The team includes:
- Pediatric oncologists who lead the treatment plan
- Surgical oncologists who do surgeries
- Radiation oncologists who give radiation therapy
- Pathologists who check tissue samples
- Nurses and nurse practitioners who care for patients
- Social workers and psychologists who help with emotional and social needs
The team’s makeup changes based on the patient’s needs and disease stage. It’s important for these experts to work together. They create a treatment plan that fits each child’s needs.
Supportive Care and Symptom Management
Supportive care is key in managing neuroblastoma. It focuses on easing symptoms, preventing problems, and improving life quality. This includes:
| Supportive Care Measure | Description | Benefits |
| Pain management | Medications and other methods to control pain | More comfort and less distress |
| Nutritional support | Helping patients get enough nutrition | Better recovery and less malnutrition risk |
| Infection prevention | Using antibiotics and other ways to stop infections | Less chance of complications and better results |
Adding supportive care to treatment plans can greatly improve outcomes. It makes patients’ lives better overall.
Differential Diagnosis: Other Pediatric Abdominal Tumors
Other than neuroblastoma, kids can get Wilms tumor, hepatoblastoma, and rare cancers. It’s key to diagnose these right for the best treatment.
Wilms Tumor and Renal Neoplasms
Wilms tumor, or nephroblastoma, starts in the kidneys. It’s the top kidney cancer in kids. Early treatment has made Wilms tumor more treatable.
- It shows up as a big, feelable belly mass
- It might link to genetic issues like WAGR or Denys-Drash syndrome
- Treatment includes surgery, chemo, and sometimes radiation
| Characteristics | Wilms Tumor | Neuroblastoma |
| Origin | Kidney | Neural crest cells |
| Age of Presentation | Typically under 5 years | Can occur at any age, often under 5 years |
| Common Symptoms | Abdominal mass, hypertension | Abdominal mass, bone pain, opsoclonus-myoclonus syndrome |
Hepatoblastoma and Liver Tumors
Hepatoblastoma is the main liver cancer in kids, hitting those under 3 hard. Thanks to better chemo and surgery, more kids survive hepatoblastoma.
“The treatment of hepatoblastoma involves a combination of chemotherapy and surgery, with liver transplantation considered in some cases.”
– Current Pediatric Oncology Guidelines
Rare Abdominal Malignancies in Children
Children can also get rare cancers like desmoplastic small round cell tumors (DSRCT) and primitive neuroectodermal tumors (PNET). These are hard to diagnose because they’re rare and symptoms are not clear.
- Desmoplastic small round cell tumors (DSRCT)
- Primitive neuroectodermal tumors (PNET)
- Rhabdomyosarcoma
Knowing about these tumors is key for the right diagnosis and care. This shows why a team effort is needed in treating kids with cancer.
Conclusion
Neuroblastoma is a complex disease that needs a full care plan. Thanks to pediatric oncology insights, doctors now know more about it. This knowledge helps them find better ways to treat childhood cancer.
Keeping up with medical research insights is key to better cancer survival rates in kids. By always looking at new research and treatments, we make sure kids get the best care.
We’ve seen how important it is to treat children with neuroblastoma and other tumors as a team. We must keep working together. This way, we can learn more and find better ways to treat these diseases.
FAQ
What is neuroblastoma, and how does it develop?
Neuroblastoma is a cancer that starts in nerve cells. It often grows in the adrenal glands, neck, chest, or spinal cord. It’s the most common solid tumor outside the brain in kids.
What are the common symptoms of neuroblastoma in children?
Symptoms vary based on where the tumor is. They can include a swollen belly, bone pain, feeling tired, losing weight, and diarrhea. Babies might have eye and muscle movements they can’t control.
How is neuroblastoma diagnosed?
Doctors use scans like ultrasound, CT, or MRI to find the tumor. They also check urine levels and do biopsies. A biopsy is key to confirm the diagnosis and learn about the tumor.
What are the different staging systems used for neuroblastoma?
There are two main systems: the International Neuroblastoma Staging System (INSS) and the International Neuroblastoma Risk Group (INRG) Classification. These help figure out how far the disease has spread and guide treatment.
What are the treatment options for neuroblastoma?
Treatments include surgery, chemotherapy, radiation, immunotherapy, and targeted biological agents. The choice depends on the tumor, its stage, and the child’s health.
What is the role of genetic testing in neuroblastoma diagnosis and treatment?
Genetic testing finds important changes in genes that affect treatment and outlook. It’s a key part of managing neuroblastoma.
How does risk stratification impact treatment planning for neuroblastoma?
Risk stratification uses age, stage, and biological markers to predict outcomes. It helps tailor treatments to each patient, ensuring they get the best care.
What are some of the emerging therapies for neuroblastoma?
New therapies include immunotherapy, targeted agents, stem cell transplants, and MIBG therapy. These offer hope for better treatment results for kids with neuroblastoma.
How does multidisciplinary care impact the management of neuroblastoma?
A team approach, with specialists like oncologists and surgeons, is vital. It ensures a complete care plan and better outcomes for kids with neuroblastoma.
What are some other pediatric abdominal tumors that may be considered in the differential diagnosis of neuroblastoma?
Other tumors like Wilms tumor, hepatoblastoma, and rare cancers might be considered. Accurate diagnosis is key for proper treatment.
What is the significance of early detection in pediatric abdominal tumors?
Finding tumors early is critical for better treatment results. Screening and risk-based approaches are being explored to help catch tumors early.
How do pediatric oncology teams manage supportive care and symptom management?
Teams focus on supportive care and managing symptoms. They aim to improve the quality of life for kids with neuroblastoma and other tumors, addressing their physical, emotional, and psychological needs.
Reference
LaQuaglia, M. P. (2019). Advances in the treatment of pediatric solid tumors. Seminars in Pediatric Surgery, 28(6), 150939. https://pmc.ncbi.nlm.nih.gov/articles/PMC9473291/