Last Updated on December 1, 2025 by Bilal Hasdemir

Wilms tumor, or nephroblastoma, is a rare kidney cancer that primarily affects children. About 1 in 500 children will get Wilms tumor before they turn 15. This makes it a big worry for parents and doctors most common solid renal tumor childhood.
Getting a Wilms tumor diagnosis can feel scary. We’re here to help families through this tough time. We offer top-notch medical care and support. Kids with Wilms tumor often get better with surgery, chemo, and radiation.
Key Takeaways
- Wilms tumor is a rare kidney cancer that mainly affects kids.
- The condition is usually found in children under 7.
- Treatment options include surgery, chemotherapy, and radiation therapy.
- How well a child does depends on the tumor’s stage and type.
- Early detection and full care are key for good results.
Understanding Wilms Tumor: The Most Common Solid Renal Tumor of Childhood
Wilms tumor is a kidney cancer that mainly hits kids. It’s a big deal in the field of pediatric oncology. We’ll dive into what it is, its history, and why it matters.
Definition and Overview of Wilms Tumor

Wilms tumor, or nephroblastoma, is a rare kidney cancer that primarily affects children.
Doctors figure out if it’s Wilms tumor by looking at it under a microscope. They see three main parts: blastemal, epithelial, and stromal. How much of each part affects how the tumor acts and how it’s treated.
Historical Perspective and Naming
Max Wilms, a German surgeon, first talked about this tumor in 1899. His work helped us understand it better. Today, thanks to new treatments, Wilms tumor is much more treatable.
Looking back, we see how far we’ve come in treating Wilms tumor. What used to be almost always deadly is now often curable. This is thanks to better treatments that include surgery, chemo, and sometimes radiation.
| Characteristic | Description | Clinical Significance |
| Age of Onset | Typically under 5 years | Early detection is key |
| Presentation | Abdominal mass, sometimes with pain or blood in urine | Quick check-ups are important |
| Treatment Approach | Surgery, chemo, and sometimes radiation therapy | Combining treatments helps more |
| Prognosis | Varies based on stage and type | Knowing the stage is vital |
Epidemiology and Incidence of Wilms Tumor
Looking into Wilms tumor, we see age, location, and ethnicity matter a lot. It’s the top kidney cancer in kids, making up 6% of all childhood cancers.
Age Distribution and Demographics
Most kids get Wilms tumor between 3 and 4 years old. It’s rare in kids under 6 months or over 6 years. This shows a link to how the kidney develops.
Demographically, who gets Wilms tumor varies. For example, African kids get it more often than Caucasian kids.
Geographical and Ethnic Variations
Where you live and who you are affects Wilms tumor rates. Some groups and places have more cases. For example, African kids get it more than Asian or European kids.
Epidemiological studies show different rates in different countries. This might be due to environment or genes.
Gender Differences in Occurrence
Some studies say girls might get Wilms tumor a bit more. But, not all studies agree. It depends on the group being studied.
Knowing about Wilms tumor’s patterns helps catch it early. More research can lead to better screening and care for kids with Wilms tumor.
Etiology and Risk Factors for Pediatric Renal Tumors
The exact causes of Wilms tumor are not fully understood. But, research has found several risk factors. Knowing these helps in early detection and treatment.
Genetic Predisposition and Syndromes
Genetics play a big role in Wilms tumor. Some genetic syndromes raise the risk of getting this disease. These include:
- WAGR Syndrome: A rare disorder with Wilms tumor, Aniridia, Genitourinary anomalies, and mental Retardation.
- Beckwith-Wiedemann Syndrome: A growth disorder that increases the risk of several types of tumors, including Wilms tumor.
- Denys-Drash Syndrome: A rare disorder associated with Wilms tumor, kidney disease, and genital abnormalities.
These syndromes often come from specific gene mutations. The WT1 gene is key for normal kidney development.
Environmental Risk Factors
Genetics are important, but environment also plays a part. Some environmental factors include:
- Maternal Exposure to Certain Chemicals: Exposure to certain chemicals during pregnancy may increase the risk of Wilms tumor in children.
- Parental Occupational Exposure: Certain occupational exposures, such as to hydrocarbons, have been suggested as possible risk factors.
But, more research is needed to understand environmental factors in Wilms tumor.
Sporadic vs. Hereditary Cases
Most Wilms tumors are sporadic, with no family history. But, some cases are hereditary, caused by inherited genetic mutations. Knowing the difference is key for genetic counseling and risk assessment.
Families with Wilms tumor history should get genetic counseling. This helps understand risks and implications for their children.
Pathophysiology and Molecular Biology of Wilms Tumor
Wilms tumor starts with genetic changes and problems in kidney growth. It’s the top kidney cancer in kids. It comes from cells that don’t grow right.
Genetic Alterations in Wilms Tumor
Genetic changes are key in Wilms tumor. The WT1 gene on chromosome 11p13 is a big player. It helps stop tumors but often gets mutated.
Other genes like CTNNB1 and WTX also play a part. They help tumors grow by turning on bad pathways.
Tumor Suppressor Genes and Oncogenes
Tumor suppressors and oncogenes control cell growth. In Wilms tumor, they get messed up. For example, MYC and MYCN help cells grow too much.
“The interplay between tumor suppressor genes and oncogenes in Wilms tumor highlights the complexity of its molecular pathogenesis.”
Developmental Pathways Involved
Wilms tumor is linked to kidney growth problems. The metanephric mesenchyme is key. It’s where tumors start.
Knowing these pathways helps us understand Wilms tumor. It also helps us find new treatments.
Clinical Presentation and Symptoms of Childhood Renal Tumors
It’s vital to spot the signs of childhood renal tumors early. We’ll talk about the usual signs that might mean a child has Wilms tumor. This is the most common kidney tumor in kids.
Common Presenting Signs and Symptoms
Kids with Wilms tumor often have a noticeable belly mass. This is usually the first sign. They might also have belly pain, fever, and blood in their urine. Sometimes, high blood pressure can happen because of the tumor pressing on blood vessels.
Key symptoms to watch for:
- Abdominal mass or swelling
- Abdominal pain or discomfort
- Fever
- Hematuria (blood in the urine)
- Hypertension
Abdominal Mass and Associated Findings
An abdominal mass is a big sign of Wilms tumor. Parents or doctors might find it during a check-up. Tests like ultrasound or CT scans help confirm the tumor and see how big it is.
| Clinical Finding | Frequency | Clinical Significance |
| Abdominal Mass | 80-90% | Primary presenting feature |
| Abdominal Pain | 30-40% | May indicate tumor rupture or hemorrhage |
| Hematuria | 15-25% | May indicate tumor invasion into the collecting system |
Systemic Manifestations
Some kids with Wilms tumor might feel tired, lose weight, or not want to eat. These signs can mean the tumor is growing or spreading.
“Early recognition of the clinical presentation of Wilms tumor is vital for effective management and better outcomes.”
— Pediatric Oncology Experts
Knowing the signs of pediatric kidney tumors is key to catching them early. This helps doctors treat them quickly. Understanding these signs helps improve how well kids do after treatment.
Differential Diagnosis of Solid Renal Tumors in Children
When a child has a solid renal mass, doctors must figure out what it is. They look at many possible causes to treat it right.
Other Pediatric Renal Neoplasms
Children can have different types of kidney tumors. Clear cell sarcoma grows fast and spreads to bones. Rhabdoid tumoris very aggressive and can cause high calcium levels.
Non-Neoplastic Renal Masses
Some non-cancerous issues can look like tumors. These include renal cysts, multicystic dysplastic kidney, and renal abscesses. Doctors use imaging to tell them apart from cancer.
Distinguishing Features of Various Renal Tumors
Each kidney tumor has its own signs. For example, Wilms tumor is big and noticeable. Renal cell carcinoma might cause blood in the urine. Knowing these differences helps doctors make the right call.
Getting the right diagnosis is key to the right treatment. Doctors look at all possible causes of kidney tumors in kids. This way, they can give the best care.
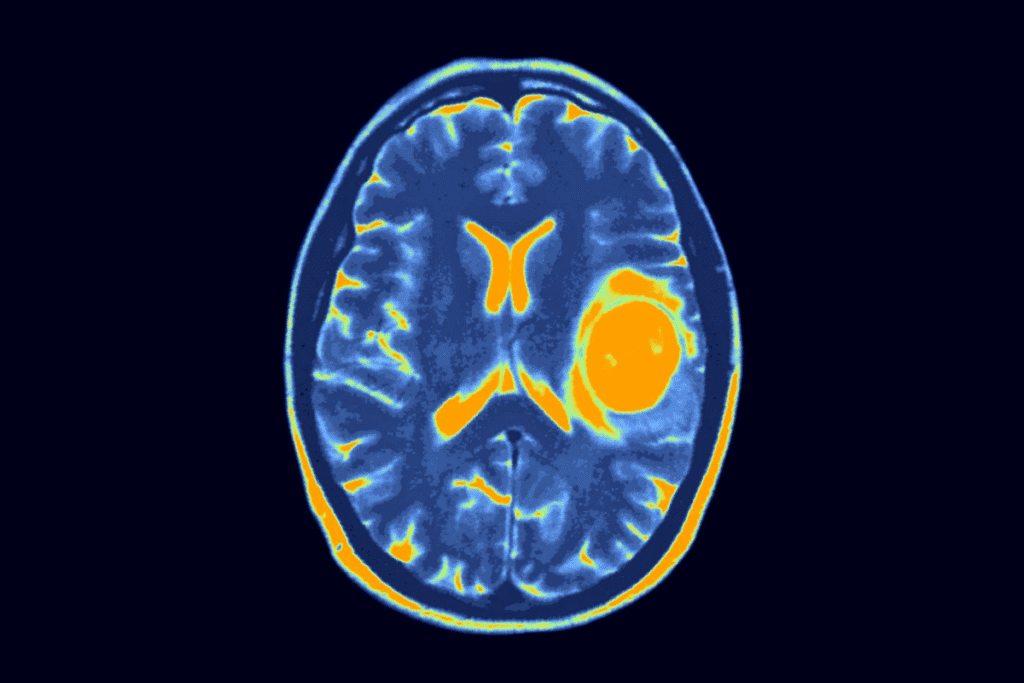
Diagnostic Approach to Pediatric Kidney Tumors
When we think Wilms tumor in kids, we need a detailed check-up. This check-up includes imaging, lab tests, and sometimes a biopsy.
Imaging Studies
Imaging is key in finding Wilms tumor. Ultrasound is often first because it’s safe and shows solid or cystic masses. Then, CT scans or MRI give more details about the tumor and nearby areas.
Choosing between CT and MRI depends on the case. MRI is great for looking at the blood vessels and avoiding radiation. It’s also good for checking the inferior vena cava for tumor thrombus.
Laboratory Investigations
Labs are important in diagnosing Wilms tumor. Blood tests can show signs like anemia or high creatinine levels. Urine analysis might show blood in the urine, a common sign.
Some tumor markers are checked too. For example, high alpha-fetoprotein (AFP) levels are more often linked to other tumors.
Biopsy Considerations
Even with imaging and lab tests, biopsy is the best way to confirm Wilms tumor. It’s usually done after imaging and before starting treatment.
The biopsy method can be fine-needle aspiration biopsy (FNAB) or core needle biopsy. The choice depends on the tumor and the hospital’s rules.
Staging and Classification Systems for Wilms Tumor
Staging and classifying Wilms tumor is key in pediatric oncology. It helps decide treatment and predict outcomes. Accurate staging is vital for knowing the disease extent and choosing the right treatment.
National Wilms Tumor Study Group Staging
The National Wilms Tumor Study Group (NWTSG) staging system is widely used. It classifies Wilms tumor based on how far the tumor has spread. The system divides tumors into five stages:
- Stage I: Tumor is only in the kidney and is completely removed.
- Stage II: Tumor is outside the kidney but is fully removed.
- Stage III: There is some tumor left in the abdomen.
- Stage IV: Tumor has spread through the blood to lungs, liver, bone, or brain.
- Stage V: Both kidneys have tumors at diagnosis.
This system helps sort patients into different risk groups. It guides how intense the treatment should be.
International Society of Pediatric Oncology Classification
The International Society of Pediatric Oncology (SIOP) classification is also important. It focuses on tumor histology after chemotherapy starts.
SIOP divides Wilms tumors into three main types:
- Low-risk: Tumors with a good histology.
- Intermediate-risk: Tumors with a non-anaplastic histology.
- High-risk: Tumors with anaplastic features.
This classification is key for knowing the prognosis and adjusting treatment after surgery.
Histopathological Risk Stratification
Histopathological risk stratification is vital in managing Wilms tumor. The presence or absence of anaplasia is a major factor in tumor behavior and prognosis.
Tumors are classified as:
- Favorable histology: No anaplasia.
- Unfavorable histology: Anaplasia is present, which can be focal or diffuse.
Anaplasia means the tumor is more aggressive. It needs more intense treatment.
Understanding these systems is critical for doctors to give the best care to children with Wilms tumor. Accurate staging and classification help create a treatment plan. This plan aims to be effective while minimizing long-term side effects.
Treatment Strategies for Childhood Renal Tumors
Childhood renal tumors, like Wilms tumor, need a detailed treatment plan. This plan uses different treatments. The goal is to increase survival rates and reduce long-term side effects.
Surgical Management
Surgery is key in treating Wilms tumor. The main aim is to remove the tumor completely. This helps check how far the disease has spread.
Radical nephrectomy is the main surgery. It often includes checking lymph nodes. This helps decide the next steps in treatment.
Chemotherapy Protocols
Chemotherapy is vital in treating Wilms tumor. It’s used before surgery to shrink the tumor. It’s also used after surgery to kill any cancer cells left behind.
Actinomycin D and vincristine are common chemotherapy drugs. Doxorubicin is added for higher-risk cases.
Radiation Therapy Indications
Radiation therapy is used for more advanced Wilms tumor or those with certain types of cancer. The choice to use radiation depends on the tumor’s stage and type. It also depends on how well the patient responds to chemotherapy.
Multidisciplinary Approach to Treatment
Treating Wilms tumor needs a team effort. This team includes pediatric oncologists, surgeons, radiologists, and radiation oncologists. Working together ensures all aspects of the disease are covered. The treatment plan is made to fit each patient’s needs.
By combining surgery, chemotherapy, and sometimes radiation, we can get the best results for kids with Wilms tumor. Improving treatment plans helps increase survival rates and improve quality of life for these young patients.
Management of Bilateral and Metastatic Wilms Tumor
Managing bilateral and metastatic Wilms tumor is a big challenge in kids’ cancer care. It needs a special treatment plan. This plan aims to control the tumor while keeping the kidney working well and avoiding long-term problems.
Approach to Bilateral Disease
Bilateral Wilms tumor affects about 5-7% of cases. It’s a tough case to handle. Our goal is to keep the kidney working and control the tumor. We start with chemotherapy to shrink the tumors.
Then, we do surgery to remove the tumors. Sometimes, we have to take out part of the kidney to save it. We use special imaging to plan the surgery.
Treatment of Pulmonary and Other Metastases
When Wilms tumor spreads, like to the lungs, we treat it all over. We use strong chemotherapy and sometimes radiation for lung spots. The treatment plan changes based on how the disease responds.
If the disease doesn’t get better with usual treatments, we try new things. This includes special medicines and joining clinical trials. We watch closely with scans to see how the treatment is working.
Special Considerations in Complex Cases
For tough cases, like bilateral disease or lots of spread, we need a team effort. We work with many experts to make a detailed plan. This team includes doctors, surgeons, and more.
It’s also important to take care of the patient’s and family’s needs. We help with their physical and emotional health during treatment.
| Treatment Aspect | Bilateral Wilms Tumor | Metastatic Wilms Tumor |
| Primary Treatment | Chemotherapy followed by surgery | Intensive chemotherapy |
| Role of Radiation Therapy | Limited, depending on tumor response | Often used for pulmonary metastases |
| Surgical Considerations | Partial nephrectomy to preserve renal function | Metastasectomy in selected cases |
Prognosis and Survival Rates for Wilms Tumor
Understanding Wilms tumor prognosis is key to managing the disease. It guides treatment choices and affects patient outcomes. Thanks to better treatments and team care, kids’ chances of beating Wilms tumor have greatly improved.
Favorable Prognostic Factors
Several factors help predict a good outcome for Wilms tumor patients. These include:
- Age at Diagnosis: Younger kids, under 2, usually have a better shot.
- Tumor Stage: Tumors caught early are more likely to be cured.
- Histopathology: Tumors that look less aggressive tend to respond well to treatment.
Long-term Survival Statistics
Survival rates for Wilms tumor have seen a big jump. In developed countries, about 90% of kids with Wilms tumor live long-term.
| Stage | Survival Rate (%) |
| I | 95-100 |
| II | 90-95 |
| III | 80-90 |
| IV | 70-80 |
| V | 50-70 |
Recurrence Patterns and Management
Wilms tumor can come back, often within two years after treatment. How to handle it depends on the first treatment and where it comes back.
Knowing about Wilms tumor prognosis and survival rates helps families make informed choices. By understanding what affects prognosis and knowing survival stats, families can face Wilms tumor challenges better.
Long-term Complications and Follow-up Care
Survivors of Wilms tumor face new challenges after treatment. They need to deal with long-term complications and ongoing care. It’s important to provide care that meets their complex needs.
Late Effects of Treatment
Treatment for Wilms tumor can affect a patient’s health long-term. Issues like growth problems, organ function, and higher cancer risk can occur. It’s key to manage these effects to improve survivors’ quality of life.
Renal Function Monitoring
Wilms tumor impacts the kidneys, so monitoring kidney function is vital. Survivors might face kidney damage or reduced function due to treatment. Tests like serum creatinine and GFR help catch and manage kidney problems early.
Surveillance for Second Malignancies
Survivors of Wilms tumor are at higher risk for new cancers, mainly if they had radiation therapy. Regular checks are needed for early cancer detection and treatment. Long-term follow-up is recommended to watch for secondary cancers.
Psychosocial Support and Quality of Life
The effects of Wilms tumor and its treatment go beyond physical health. They impact survivors’ mental and social well-being. It’s important to offer psychosocial support and improve their quality of life through holistic care.
| Aspect of Care | Recommendations | Frequency |
| Renal Function Monitoring | Serum creatinine, GFR | Annually |
| Surveillance for Second Malignancies | Imaging studies, physical exams | As per guidelines |
| Psychosocial Support | Counseling, support groups | Ongoing |
Prevention and Screening for High-Risk Children
For kids at high risk, early action is key. Wilms tumor, a common kidney tumor in kids, needs a strong plan for early catch and prevention. This is even more important for kids with genes that make them more likely to get it.
Surveillance Protocols for Genetic Syndromes
Kids with certain genetic syndromes face a higher risk of Wilms tumor. Surveillance protocols are vital for spotting it early in these groups. For example, kids with Beckwith-Wiedemann, Denys-Drash, or WAGR syndromes need regular checks.
- Ultrasound checks every 3-4 months until age 8 are advised.
- Start screening early, at birth if the condition is found before birth.
- It’s important for families to stick to the screening schedule.
Screening Recommendations
Screening for Wilms tumor uses imaging and clinical checks. Ultrasound is the first choice because it’s safe and doesn’t use radiation.
- Ultrasound should be done by skilled operators.
- How often to screen depends on the child’s risk level.
- At times, MRI might be suggested for more detailed checks.
Genetic Counseling for Families
Genetic counseling is key for families with high-risk kids. Genetic counselors explain the risk of getting it again, passing it to future kids, and what genetic tests mean.
Understanding their child’s condition and options helps families. We suggest families with Wilms tumor or related syndromes get genetic counseling. This way, they can make smart choices about their child’s care and future family planning.
Conclusion
Wilms tumor is the most common kidney cancer in kids. It needs a detailed approach for diagnosis and treatment. Knowing about its causes and how it works is key for early detection and treatment.
New imaging, chemotherapy, and surgery methods have made treatment better. A team effort is vital for treating Wilms tumor. This includes handling cases where the tumor is in both kidneys or has spread.
It’s important to keep an eye on kids after treatment for Wilms tumor. This helps catch any late effects or if the cancer comes back. By learning more about Wilms tumor, we can help kids live better lives with this cancer.
FAQ
What is Wilms tumor, and how common is it in children?
Wilms tumor, or nephroblastoma, is a rare kidney cancer that primarily affects children. about 90% of all kidney tumors in children. It usually happens in kids aged 3 to 4.
What are the symptoms of Wilms tumor?
Symptoms include a big belly mass, pain, fever, and blood in the urine. Kids might also have high blood pressure, lose their appetite, or lose weight.
How is Wilms tumor diagnosed?
Doctors use ultrasound, CT scans, or MRI to see the tumor. They also do blood and urine tests. A biopsy might be needed to confirm it.
What are the risk factors for developing Wilms tumor?
Kids with WAGR syndrome or Beckwith-Wiedemann syndrome are at higher risk. Family history also plays a role in some cases.
How is Wilms tumor staged?
The NWTS staging system is used. It looks at how big the tumor is and if it has spread.
What are the treatment options for Wilms tumor?
Treatment includes surgery, chemotherapy, and sometimes radiation. A team of doctors works together to plan the treatment.
What is the prognosis for children with Wilms tumor?
Over 90% of kids with Wilms tumor are cured. The chance of survival depends on the tumor’s stage, type, and how well it responds to treatment.
Are there any long-term complications associated with Wilms tumor treatment?
Yes, kids might face kidney damage, scoliosis, and a higher risk of other cancers. They need ongoing care to watch for these issues.
Can Wilms tumor be prevented?
There’s no sure way to prevent Wilms tumor. But, kids with certain genetic syndromes might get regular checks to catch it early.
What is the role of genetic counseling in Wilms tumor?
Genetic counseling helps families understand the risks and genetic links of Wilms tumor, mainly in genetic syndromes.
How does bilateral Wilms tumor affect treatment and prognosis?
Bilateral Wilms tumor needs a complex treatment plan. It often includes surgery, chemotherapy, and sometimes radiation. This helps keep the kidneys working while fighting the tumor.
References:
- Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. (2024). Childhood solid tumor types and programs. https://www.dana-farber.org/cancer-care/treatment/childhood-solid-tumors/programs