Preimplantation genetic testing for aneuploidy (PGT-A) is key in fertility treatments. It helps find euploid embryos with the right number of chromosomes. Prospective parents often ask how many embryos will pass genetic testing and be ready for transfer. Data analysis on how many embryos pass pgt testing (Euploid rate) based on maternal age.
Studies show that euploid embryo rates change a lot with age and embryo quality. A big study looked at 1809 embryos and found 69.8 percent were euploid. Knowing these numbers helps patients understand what to expect and make better choices about their fertility journey.
Key Takeaways
- PGT-A testing screens embryos for chromosomal abnormalities before transfer.
- Euploid embryo rates vary significantly based on maternal age and embryo quality.
- A major trial found 69.8 percent of analyzed embryos to be euploid.
- Understanding PGT-A outcomes helps patients make informed decisions.
- PGT-A is a key tool in fertility treatments, boosting IVF success rates.
Understanding PGT Testing in Fertility Treatments

PGT testing is key in modern fertility treatments. It helps us understand embryo genetics better. Knowing about the different PGT types and their benefits is vital.
What is Preimplantation Genetic Testing?
Preimplantation Genetic Testing (PGT) is used in IVF to check embryos for genetic issues before they’re transferred. PGT-A screens for chromosomal problems. Other PGT types look for specific genetic disorders and structural issues. This helps find the best embryos for a healthy pregnancy.
Types of PGT: PGT-A, PGT-M, and PGT-SR
There are several PGT types, each with its own purpose:
- PGT-A (Preimplantation Genetic Testing for Aneuploidy): It finds chromosomal issues in embryos. This boosts the chance of a successful transfer, mainly for older women.
- PGT-M (Preimplantation Genetic Testing for Monogenic Disorders): It tests for specific genetic diseases like cystic fibrosis or sickle cell anemia. This lets couples choose embryos without these conditions.
- PGT-SR (Preimplantation Genetic Testing for Structural Rearrangements): It spots embryos with structural chromosomal problems. These can affect fertility and increase miscarriage risk.
The Purpose and Benefits of Embryo Screening
The main goal of PGT is to boost IVF success rates by picking genetically normal embryos. The advantages are:
- Higher chances of a healthy pregnancy
- Lower risk of miscarriage due to chromosomal issues
- More informed choices for couples going through IVF
By knowing about the various PGT types and their uses, couples can make better choices for their fertility treatments.
The Evolution of Embryo Genetic Testing
[Add image here]
Embryo genetic testing has changed a lot. This is thanks to new technology and a better understanding of genetics. Now, we can find and choose the best embryos for fertility treatments.
From PGS to PGT-A: Terminology Changes
The way we talk about embryo genetic testing has changed. We now use Preimplantation Genetic Testing for Aneuploidy (PGT-A) instead of Preimplantation Genetic Screening (PGS). This change shows we know more about what the test does. PGT-A is better because it clearly says the test looks for chromosomal problems.
Before, “PGS” was a catch-all term for many tests. Now, “PGT-A” is specific. It tells everyone the test is about finding aneuploidies.
Technological Advancements in Embryo Testing
New technology has been key in improving embryo genetic testing. With tools like next-generation sequencing (NGS), we can look at genetic material in more detail. This means we can spot problems that were hard to find before.
These new tools also let us work with tiny DNA samples. This is important because we only have a little DNA from an embryo biopsy. Thanks to these advances, we can pick the healthiest embryos for IVF.
Improved Accuracy in Modern Testing Methods
Today’s embryo genetic testing is much more accurate. Thanks to PGT-A and new tech, we can tell if an embryo is healthy or not. This helps avoid problems during IVF.
Research shows PGT-A leads to better IVF results. It means more successful pregnancies and fewer miscarriages. By choosing healthy embryos, we increase the chances of a successful pregnancy.
The IVF Process Leading to PGT Testing
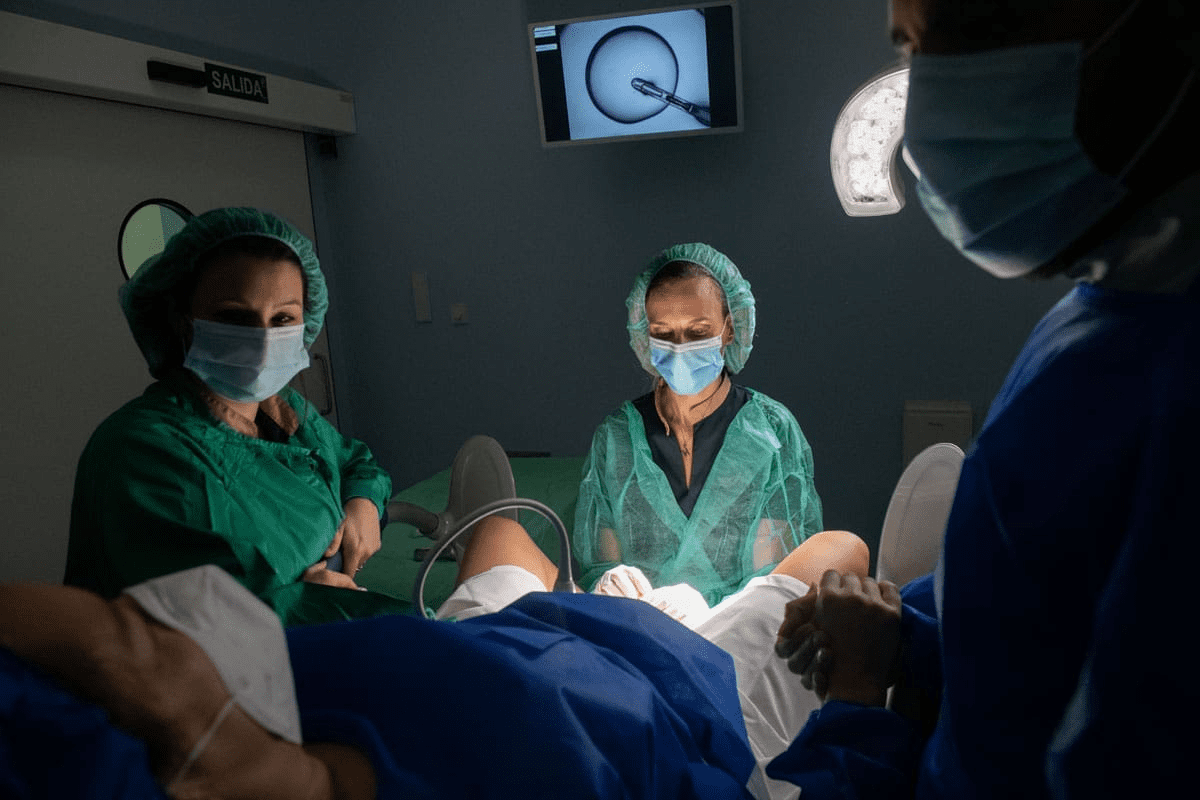
The journey to PGT testing starts with IVF. This is a series of steps that lead to genetic testing of embryos. The IVF process includes stimulation, egg retrieval, fertilization, and growth until the blastocyst stage.
Stimulation and Egg Retrieval
The first step is ovarian stimulation. Medications are used to make the ovaries produce many eggs. This increases the chance of getting multiple embryos for PGT testing. After the eggs are ready, a minor surgery is done to get them.
Fertilization and Early Embryo Development
After getting the eggs, they are fertilized in the lab. This can be through insemination or ICSI. The zygotes then grow in the lab, with embryologists checking their quality.
Blastocyst Formation and Biopsy Procedure
As embryos grow, they reach the blastocyst stage in 5-6 days. At this point, they have two cell groups: the inner cell mass and the trophectoderm. For PGT testing, cells from the trophectoderm are removed for genetic analysis.
The IVF process is complex, with many steps before PGT-A testing. Knowing these steps helps understand the importance of PGT-A testing in finding genetically normal embryos.
| Stage | Description | Timeline |
|---|---|---|
| Stimulation | Medications stimulate ovaries to produce multiple eggs | Several days to 2 weeks |
| Egg Retrieval | Minor surgical procedure to retrieve eggs | Day of retrieval |
| Fertilization | Eggs are fertilized with sperm | Day of retrieval |
| Embryo Culture | Embryos are cultured and monitored | 5-6 days |
| Blastocyst Biopsy | Trophectoderm cells are biopsied for PGT testing | Day 5-6 |
How Many Embryos Pass PGT Testing: A Look at the Numbers
Clinical trials have given us a clear picture of embryo types after PGT-A testing. Preimplantation Genetic Testing for aneuploidy (PGT-A) is key in IVF. It tells us about the genetic health of embryos.
The 69.8% Euploid Rate in Major Clinical Trials
Studies show that 69.8% of embryos are euploid. This is good news because it means these embryos have the right number of chromosomes. They could be viable for IVF transfer.
Aneuploid Embryo Rates (17.2%)
On the other hand, 17.2% of embryos are aneuploid. This means they have too many or too few chromosomes. Aneuploidy can lead to failed implantation, miscarriage, and chromosomal disorders.
Mosaic Embryo Prevalence (11.7%)
Mosaic embryos, with both normal and abnormal cells, make up 11.7% of cases. Mosaicism can make it hard to understand PGT-A results. It’s not always clear if the whole embryo is affected.
Questionable or No Result Cases (1.4%)
1.4% of PGT-A tests are unclear or show no results. This can happen for many reasons. It might be due to poor biopsy quality or technical problems during testing.
Here’s a table summarizing the types of embryos based on PGT-A results:
| Embryo Type | Percentage |
|---|---|
| Euploid | 69.8% |
| Aneuploid | 17.2% |
| Mosaic | 11.7% |
| Questionable/No Result | 1.4% |
Knowing these numbers is important for both patients and doctors. It helps in making decisions about embryo transfer and whether more testing or treatment cycles are needed.
Age-Related Factors Affecting PGT Success Rates
Age is key in PGT success, a big part of modern fertility treatments. Looking into PGT success, age stands out as a major factor.
Maternal Age and Chromosomal Abnormalities
Maternal age greatly affects PGT success. As women get older, the chance of chromosomal issues in embryos goes up. This means fewer healthy embryos for transfer. Studies show that the number of healthy embryos drops with age, making age a big deal in planning for a family.
Chromosomal abnormalities are a big worry with older mothers. They can cause failed implantation, miscarriage, or birth defects. PGT-A testing spots these issues, letting doctors pick the healthiest embryos.
Success Rates by Age Group
PGT success rates change a lot with age. Younger women tend to have better success rates because they have fewer chromosomal problems. But, as age goes up, success rates go down, showing more aneuploidy.
- Women under 35 usually have the best PGT success rates.
- Success rates start to drop after age 35.
- By the early 40s, PGT success rates are much lower.
Paternal Age Considerations
While maternal age is more important, paternal age also matters in PGT success. Older dads face higher risks of genetic mutations, though it’s less than maternal age.
Studies on paternal age are ongoing. But, it’s clear that both mom’s and dad’s ages affect fertility treatment success.
Embryo Quality and Its Impact on PGT Results
Knowing about embryo quality is key to understanding PGT results. The quality of an embryo affects how well PGT-A works. Grading embryos helps predict their chances of success and genetic health.
Grading Systems for Embryo Quality
Grading systems help check how good an embryo is. They look at how the embryo is growing and its shape. This helps pick the best embryos for transfer.
Key components of embryo grading:
- Blastocyst expansion
- Inner Cell Mass (ICM) quality
- Trophectoderm (TE) quality
The 20-30% Normal Development Rate at Blastocyst Stage
About 20-30% of blastocyst-stage embryos are genetically normal. This shows why picking the right embryos is so important. PGT-A helps find these good embryos.
The number of normal embryos can change. This depends on things like the mother’s age and the embryo’s quality.
Correlation Between Embryo Grade and Genetic Normalcy
Research links embryo grade to genetic health. Better-grade embryos are more likely to be healthy. Lower-grade ones might not be.
| Embryo Grade | Euploid Rate (%) |
|---|---|
| A | 40 |
| B | 25 |
| C | 15 |
Understanding how embryo quality relates to genetic health helps us make better choices. This is important for PGT-A results and deciding on embryo transfer.
From Oocyte to Euploid Embryo: The Complete Picture
The journey from getting an oocyte to finding a euploid embryo is complex. It involves many steps and careful planning. We will look at each stage and what affects success rates.
The 30% Rate: From Retrieved Oocytes to Testable Embryos
The first step in making an embryo is key. About 30% of oocytes become testable embryos. This depends on the quality of the oocytes and the skill of the lab.
The 40% Rate: Day 3 to Blastocyst Development
Not every embryo at Day 3 turns into a blastocyst. The development rate to blastocyst is about 40%. This stage is important because it affects how many embryos can be tested.
The 18.1% Final Yield: Multicenter Analysis Findings
A study found that only 18.1% of embryos were good enough for transfer. This shows how hard the process is.
Factors Contributing to Embryo Attrition
Many things can cause embryos to not make it, like genetic issues, environment, and lab conditions. Knowing these helps improve the chances of success.
In summary, the path from oocyte to euploid embryo is complex. It has many stages and different success rates. By understanding these, we can help patients have better outcomes in fertility treatments.
Limitations and Controversies in PGT Testing
PGT-A testing has many benefits but also faces challenges. It has greatly improved fertility treatments. It’s important for patients and doctors to understand its limits.
Technical Limitations and False Results
One big issue with PGT-A testing is its technical limits. This can cause false results. The quality of the biopsy sample and the technology used for analysis are key factors.
False negatives or false positives can happen. This can lead to wrong embryo classifications.
- Inadequate biopsy samples can result in inconclusive or inaccurate results.
- The sensitivity of genetic testing technology can impact the detection of chromosomal abnormalities.
- Laboratory protocols and expertise play a critical role in the accuracy of PGT-A results.
Mosaicism Detection Challenges
Mosaicism, where an embryo has both normal and abnormal cells, is a big challenge. It’s hard to detect mosaicism accurately because of the limited cells that can be biopsied.
The complexity of mosaicism makes it hard to predict an embryo’s developmental chances. We are learning how to deal with mosaic PGT-A results.
Ethical Considerations in Embryo Selection
PGT-A testing also raises ethical questions, mainly about choosing embryos. The ability to screen embryos for genetic issues can lead to tough decisions.
Some ethical issues include:
- Deciding which genetic conditions are worth selecting for.
- Considering the moral implications of choosing or discarding embryos.
- Thinking about the emotional impact of these choices on patients.
Ongoing Debates in the Scientific Community
The scientific community is debating PGT-A testing’s technical and ethical aspects. Research is ongoing to improve its accuracy and address ethical concerns.
As we progress, it’s vital to consider different views. We need to keep talking about how to use PGT-A testing wisely in fertility treatments.
Cost-Benefit Analysis of PGT Testing
IVF treatments are getting better, and PGT is playing a big role in this. But, the cost of PGT is a big deal. Couples looking into IVF want success and are worried about the money too.
Financial Costs of Adding PGT to IVF
PGT testing costs can change a lot. It depends on the clinic, where you are, and what tests you need. On average, it can add $1,500 to $3,000 to your IVF bill. This is a big thought for many couples.
Key factors influencing PGT costs include:
- The number of embryos being tested
- The type of PGT testing required (PGT-A, PGT-M, or PGT-SR)
- Any additional services or packages offered by the fertility clinic
Potential Benefits: Improved Success Rates and Reduced Miscarriages
Research shows PGT-A can make IVF more successful. It helps pick the best embryos for transfer. This means a better chance of a healthy pregnancy.
The benefits of PGT-A include:
- Improved implantation rates
- Reduced risk of miscarriage
- Enhanced overall IVF success rates
Who Benefits Most from PGT Testing?
PGT testing helps many, but some get more benefits. This includes older women, those who keep having miscarriages, and those who haven’t succeeded with IVF before.
Insurance Coverage Considerations
Insurance for PGT testing varies a lot. Some plans cover it, while others don’t. It’s key to know what your insurance does and doesn’t cover.
Talking to your fertility specialist about insurance and PGT costs is smart. This way, you can make a choice that fits your needs and budget.
Beyond Testing: Transfer Success with PGT-Tested Embryos
The goal of PGT-A testing is to get a successful pregnancy with a healthy embryo. Now, thanks to PGT-A, it’s easier to pick and transfer embryos that are genetically normal. This has made IVF cycles more successful.
Implantation Rates with Euploid Embryos
Research shows that euploid embryos have better implantation rates than aneuploid ones. This is because they are genetically normal. This means they have a lower chance of failing to implant.
Live Birth Rates After PGT
Live birth rates after PGT-A tested embryo transfers are promising. Studies show that transferring euploid embryos leads to more live births. These embryos are more likely to grow into healthy babies.
Comparing Outcomes: PGT vs. Conventional IVF
PGT-A tested embryo transfers often have better outcomes than traditional IVF. They have higher live birth rates and fewer miscarriages. This is because they choose embryos that are genetically normal for transfer.
Multiple Cycle Planning with PGT Results
PGT-A results help not just in one IVF cycle but also in planning future cycles. Knowing the genetic makeup of embryos from previous cycles helps doctors plan better for the next ones. This can lead to higher success rates overall.
Conclusion: Making Informed Decisions About PGT Testing
Understanding Preimplantation Genetic Testing (PGT) is key in the world of fertility treatments. Our research shows PGT can greatly boost IVF success and lower miscarriage rates. We’ve looked into PGT’s types, advantages, and downsides.
Deciding on PGT testing needs a full grasp of what it involves and its effects. People trying IVF should think about their own situation. This includes their age, embryo quality, and health history.
By looking at PGT’s pros and cons, people can choose wisely for their reproductive goals. We suggest talking to fertility experts to find the right treatment for them.
FAQ
What is Preimplantation Genetic Testing (PGT) and how does it work?
PGT is a method used during IVF to check embryos for genetic problems. It takes a few cells from the embryo to analyze its genetic material. This helps identify any chromosomal or genetic issues.
What percentage of embryos pass PGT-A testing?
The success rate of PGT-A testing varies. Major studies show an average of 69.8% of embryos are euploid. But, this rate can change based on the mother’s age and the embryo’s quality.
How does maternal age affect PGT-A success rates?
Maternal age greatly affects PGT-A success. As women get older, the chance of chromosomal problems increases. This lowers the number of euploid embryos. Women under 35 usually have better results than older women.
What is the difference between PGT-A, PGT-M, and PGT-SR?
PGT-A checks for chromosomal issues. PGT-M looks for single-gene defects. PGT-SR finds structural rearrangements. Each type is used for different genetic problems.
How does embryo quality impact PGT results?
The quality of an embryo is linked to its genetics. Better embryos are more likely to be genetically normal. Grading systems help predict the genetic health of an embryo.
What are the limitations and controversies surrounding PGT testing?
PGT testing faces technical challenges like false results and detecting mosaicism. There are also debates about choosing embryos. Scientists are working to solve these issues.
How do PGT test results impact IVF success rates?
PGT testing can greatly improve IVF success. It helps choose embryos with the best genetic makeup. Studies show better implantation and birth rates with these embryos.
What are the financial costs associated with PGT testing, and is it worth it?
PGT testing adds to the cost of IVF. But, it can save money in the long run. It reduces the need for multiple transfers and lowers miscarriage rates.
Does insurance typically cover PGT testing?
Insurance coverage for PGT testing varies. Some plans cover it for certain reasons, while others don’t.
How many embryos typically develop to the blastocyst stage?
Not all embryos make it to the blastocyst stage. About 20-30% do. Of those, a certain percentage will be genetically normal based on PGT-A testing.
What is the rate of aneuploid embryos, and how does it relate to age?
Studies show about 17.2% of embryos are aneuploid. This rate goes up with the mother’s age. Age is a key factor in chromosomal abnormalities.
What is mosaicism in embryos, and how is it detected?
Mosaicism means an embryo has both normal and abnormal cells. It’s found in about 11.7% of cases. Detecting mosaicism is tricky and can make interpreting PGT results hard.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/39349118/