
Polycystic ovary syndrome (PCOS) is a common condition in women of childbearing age. It’s marked by many small ovarian follicles. This can affect fertility and overall health sex after iui is good or bad.
Women with PCOS often have 12 or more small follicles. These follicles are 2-9 mm in diameter. This condition can cause many health problems, including reproductive and metabolic issues. At Liv Hospital, we offer expert care to help you understand your condition and create a treatment plan just for you.
Our team of specialists will help you with both reproductive and metabolic health. We use the latest medical evidence and innovative healthcare practices.
Key Takeaways
- PCOS is a common endocrine disorder affecting reproductive-aged women.
- The presence of multiple small ovarian follicles is a hallmark characteristic of PCOS.
- PCOS can impact fertility and overall well-being.
- A personalized treatment plan can help address reproductive and metabolic health issues.
- Liv Hospital provides expert, patient-centered care for women with PCOS.
Understanding PCOS and Ovarian Follicles
Ovarian follicles are key in the female body, and PCOS messes with them. Knowing how they work and how PCOS affects them is important.
What Are Ovarian Follicles?
Ovarian follicles are tiny, fluid-filled spots in the ovaries with immature eggs. They help eggs grow and are vital for reproduction. Usually, many start growing each month, but only one egg is released during ovulation.
How PCOS Affects Follicle Development
PCOS messes with how ovarian follicles grow. Instead of getting ready to release an egg, many stay small. This leads to many small follicles, a sign of PCOS.
The Role of Immature Follicles
Immature follicles are a big problem in PCOS. They can’t release an egg, causing fertility issues. They also mess with hormone levels, adding to PCOS symptoms.
Knowing how PCOS affects follicles helps doctors treat it better. It also helps women with PCOS understand and manage their fertility.
Many Follicles on Ovaries: The Hallmark of PCOS
PCOS is often marked by many ovarian follicles seen on ultrasound. This is a key sign used to diagnose PCOS.
Normal ovaries have a few follicles at different stages. But, ovaries with PCOS have lots of small follicles. This gives them a “string of pearls” look on ultrasound.
Normal vs. Polycystic Ovarian Morphology
Normal ovaries have a few follicles at different stages. But, PCOS ovaries have lots of small follicles, more than 20 in each ovary. This is key for diagnosing PCOS.
The Androgen Excess and PCOS Society says polycystic ovaries are common in PCOS. But, they note it’s not enough to diagnose PCOS alone. Other symptoms and criteria are also important.
What Constitutes “Many Follicles”
Ultrasound can count “many follicles.” New guidelines use ultrasound, mainly transvaginal, to define polycystic ovaries. More than 20 follicles in each ovary is now the standard.
- Multiple small follicles, typically 2-9 mm in diameter
- Increased ovarian volume (>10 mL)
- Presence of follicles in both ovaries (bilateral ovarian follicles)
Bilateral Ovarian Follicles Explained
Bilateral ovarian follicles mean many follicles in both ovaries. This is common in PCOS and linked to hormonal and ovulation issues. It can affect fertility and menstrual cycles.
“The presence of multiple bilateral ovarian follicles is a characteristic ultrasound finding in women with PCOS, reflecting the underlying hormonal and metabolic disturbances.”
Knowing about many follicles on ovaries is key for diagnosing and treating PCOS. Healthcare providers can then tailor treatments to each patient’s needs.
PCOS Prevalence and Risk Factors
Studies show that PCOS affects about 1 in 10 women. It’s a complex condition with many factors at play.
Statistical Overview
PCOS affects between 5% and 26% of women, depending on how it’s diagnosed. This range shows the difficulty in diagnosing PCOS and the need for clear criteria.
| Diagnostic Criteria | Prevalence Rate |
|---|---|
| Rotterdam Criteria | 15%-20% |
| NIH Criteria | 5%-10% |
| Androgen Excess Society Criteria | 10%-15% |
The table shows how different criteria lead to varying prevalence rates. This highlights the need for accurate diagnosis.
Genetic and Environmental Risk Factors
PCOS often runs in families, showing a strong genetic link. Genetic predisposition is key, along with lifestyle and exposure to endocrine disruptors.
“The genetic basis of PCOS is complex, involving multiple genes that influence insulin resistance, androgen production, and follicular development.”
Environmental factors like diet and exercise also play a role. A healthy lifestyle can help reduce risk.
Age and Ethnicity Considerations
PCOS affects women of all ages and ethnicities. Age and ethnicity can change how symptoms appear and how common PCOS is. Some groups face higher risks of insulin resistance and metabolic issues.
Knowing these factors is key to early detection and management of PCOS. By understanding risks and taking action, women can lower their chance of complications.
Hormonal Imbalances in PCOS
Understanding hormonal imbalances in PCOS is key to managing the condition. PCOS involves complex hormonal disturbances that affect the body in many ways.
Elevated Androgens and Their Effects
One major hormonal imbalance in PCOS is high androgen levels. Androgens are male hormones found in both men and women. In women with PCOS, these levels are too high. This can cause symptoms like hirsutism, acne, and male-pattern baldness.
High androgens also have serious health effects. They can stop ovulation, leading to fertility problems common in PCOS.
Insulin Resistance and Follicular Development
Insulin resistance is a critical aspect of PCOS. Insulin resistance happens when the body’s cells don’t respond well to insulin. This hormone helps control blood sugar levels. As a result, the body makes more insulin, causing metabolic problems.
Insulin resistance affects follicular development in PCOS. High insulin levels can make the ovaries produce more androgens. This worsens the hormonal imbalance and disrupts normal follicular maturation and ovulation.
| Hormonal Aspect | Effect on PCOS | Clinical Implications |
|---|---|---|
| Elevated Androgens | Disrupts ovulation, leads to hirsutism and acne | Fertility issues, cosmetic concerns |
| Insulin Resistance | Exacerbates hormonal imbalance, disrupts follicular development | Metabolic issues, increased risk of diabetes |
| Hormonal Feedback Loops | Complex interplay between hormones, affects ovulation and metabolism | Difficulties in managing symptoms, need for complex treatment plans |
Hormonal Feedback Loops
The hormonal imbalances in PCOS involve complex feedback loops. The interaction between insulin, androgens, and other hormones creates a cycle that’s hard to break. For example, high insulin levels can increase androgen production. This disrupts normal hormonal feedback mechanisms, making the condition worse.
Understanding these hormonal feedback loops is vital for effective treatment. By addressing hormonal imbalances comprehensively, healthcare providers can help women with PCOS manage their symptoms better. This reduces the risk of long-term health problems.
Recognizing PCOS Symptoms
It’s key to spot PCOS symptoms early for better care. PCOS affects many areas of a woman’s health.
Menstrual Irregularities and Anovulation
Menstrual issues are a big sign of PCOS. These can be infrequent or long periods. This happens because the ovaries don’t release an egg as they should.
These problems can really upset a woman’s life.
- Infrequent menstrual periods (oligomenorrhea)
- Prolonged menstrual periods (menorrhagia)
- Amenorrhea, or the absence of menstruation
Physical Symptoms: Hirsutism, Acne, and Weight Changes
PCOS also brings physical symptoms. Hirsutism is when you grow too much hair in places you don’t want. Acne is common too, on your face, chest, and back. Many also struggle with weight changes.
- Excessive hair growth (hirsutism)
- Acne, specially on the face and upper body
- Weight changes, including obesity
Emotional and Psychological Impact
PCOS affects more than just your body. It can lead to depression and anxiety. It can also hurt your self-esteem and how you see your body.
Getting help from doctors, family, and support groups is vital. They can help you deal with the emotional side of PCOS.
Diagnosing PCOS: Modern Criteria
Today, diagnosing PCOS uses advanced ultrasound and hormone tests. This method has changed with new medical tech. It’s now more accurate and detailed.
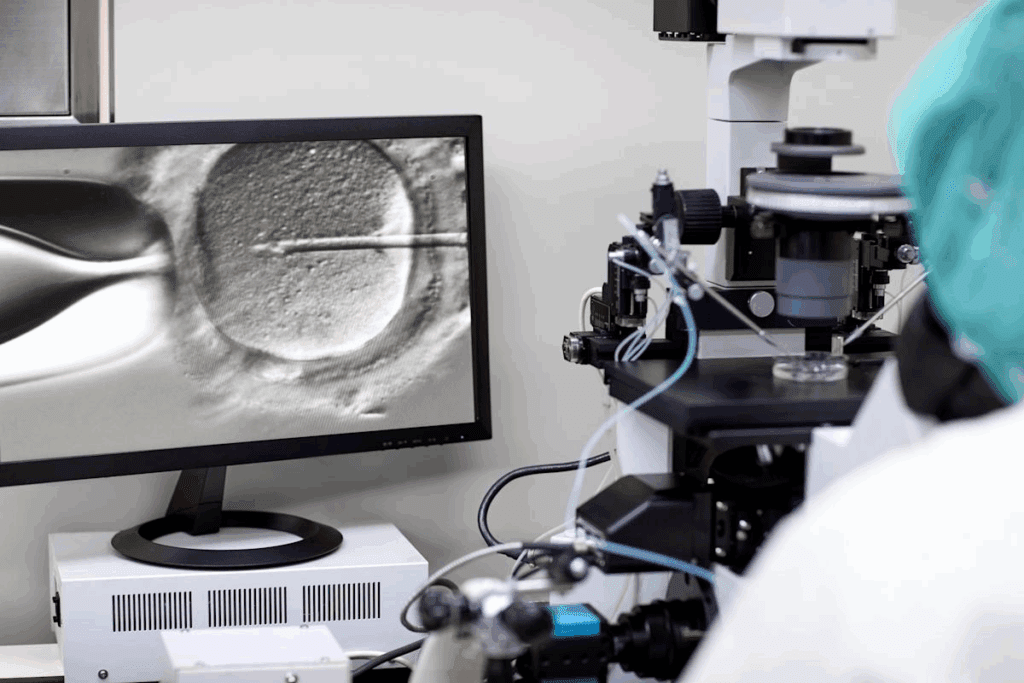
Transvaginal Ultrasound Technology
Transvaginal ultrasound is a key tool for PCOS diagnosis. It lets doctors see the ovaries clearly. They can check their size and count the follicles.
Transvaginal ultrasound helps spot the “string of pearls” look. This is when many small follicles line the ovaries.
Identifying Small Peripheral Follicles
PCOS is marked by many small peripheral follicles. These are under 10 mm and spread out in the ovaries. Ultrasound is key to finding these follicles.
This helps doctors tell PCOS apart from other conditions. It’s important for a correct diagnosis.
Blood Tests and Hormone Evaluation
Blood tests are also vital for diagnosing PCOS. They check for hormone imbalances, like androgens and insulin resistance. High androgens can cause hair growth and acne.
Testing for insulin resistance is also important. It helps understand the metabolic problems linked to PCOS.
Doctors use ultrasound and blood tests together. This way, they can accurately diagnose PCOS. Then, they can create a treatment plan that fits the person’s needs.
PCOS and Fertility Challenges
PCOS and fertility have a complex relationship. It involves many factors that affect how well a woman can ovulate and conceive. Women with PCOS often find it hard to get pregnant because of ovulation problems.
Women with PCOS face challenges because of multiple ovarian follicles. It might seem strange, but having many follicles doesn’t always mean regular ovulation. In fact, too many small follicles can mess up the ovulation process. This leads to irregular periods and makes it hard to get pregnant.
Disrupted Ovulation: A Key Fertility Challenge
PCOS with multiple ovarian follicles can cause anovulation or irregular ovulation. This is because the follicles might not grow right, causing hormonal imbalances. These imbalances can mess up the ovulation process. As a result, women with PCOS might have irregular or long periods. This makes it tough to predict when they’re ovulating and get pregnant.
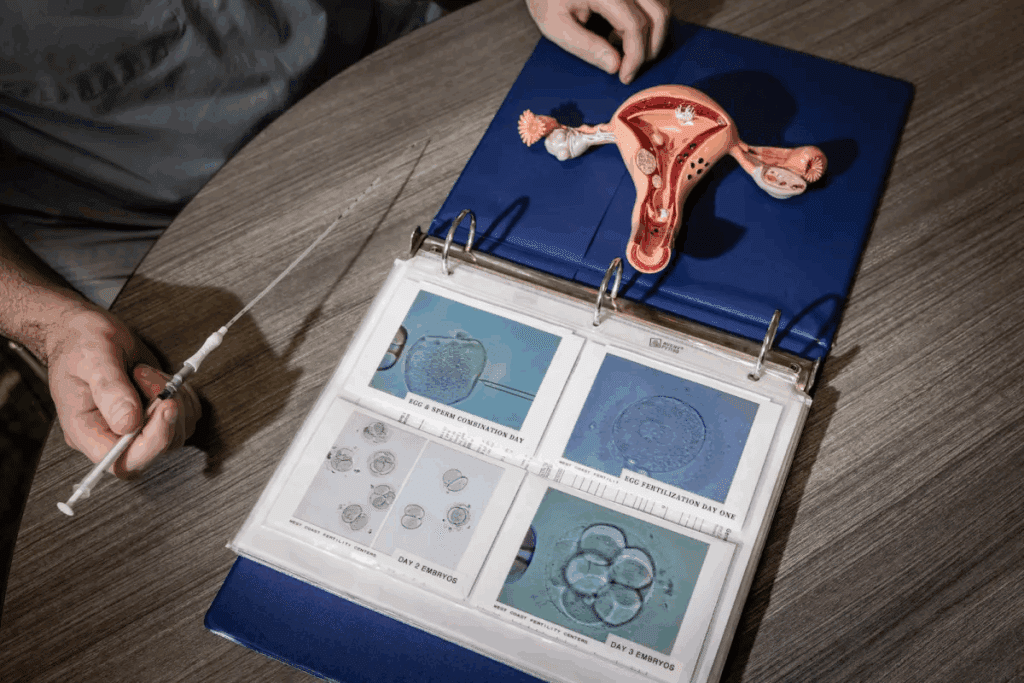
Fertility Treatment Options
There are many fertility treatments for women with PCOS. These include:
- Clomiphene Citrate: A medication that helps ovulation by releasing hormones needed for follicle growth.
- Letrozole: An aromatase inhibitor that stimulates ovulation by lowering estrogen levels and increasing FSH production.
- Gonadotropins: Injectable hormones that help the ovaries produce eggs. They’re often used with other treatments like IUI or IVF.
- IVF: A more advanced treatment where eggs are retrieved, fertilized in a lab, and then transferred to the uterus.
Success Rates and Expectations
The success of fertility treatments for women with PCOS depends on several factors. These include age, overall health, and the treatment used. Women with PCOS often respond well to fertility medications, with many getting pregnant. But, it’s important to have realistic expectations and know that results can vary.
| Treatment | Success Rate | Key Considerations |
|---|---|---|
| Clomiphene Citrate | 50-60% success rate in inducing ovulation | Often the first line of treatment; may require careful monitoring to avoid overstimulation. |
| Letrozole | Higher success rates compared to Clomiphene Citrate in some studies | May be more effective for women with PCOS who are resistant to Clomiphene Citrate. |
| Gonadotropins + IUI | 15-20% success rate per cycle | Requires careful monitoring to minimize the risk of multiple pregnancies. |
| IVF | 40-50% success rate per cycle for women under 35 | A more invasive and costly option, but often recommended for women with additional fertility issues or after failed other treatments. |
Knowing about fertility treatment options and their success rates helps women with PCOS make informed choices. While the journey can be complex, many women with PCOS successfully conceive with the right treatment.
Treatment Approaches for PCOS
Managing PCOS requires a mix of medical treatments and lifestyle changes. Every woman’s PCOS journey is different. So, treatment plans are made to fit each person’s needs and goals.
Medication Options
Medicines are key in controlling PCOS symptoms. We often give:
- Hormonal birth control to regulate menstrual cycles and lower androgen levels
- Anti-androgen medications to treat hirsutism and acne
- Fertility medications to help with ovulation
- Insulin-sensitizing medications to better insulin use
| Medication | Purpose | Benefits |
|---|---|---|
| Hormonal Birth Control | Regulate menstrual cycles, reduce androgen levels | Improves menstrual regularity, reduces hirsutism and acne |
| Anti-androgen Medications | Treat hirsutism and acne | Reduces excess hair growth, improves skin clarity |
| Fertility Medications | Stimulate ovulation | Enhances fertility, increases chances of conception |
Surgical Interventions
Sometimes, surgery is needed. Procedures like ovarian drilling can help with ovulation and fertility.
Complementary Therapies
Complementary therapies can boost the effects of medical treatments. We suggest:
- Dietary changes to manage weight and improve insulin sensitivity
- Regular exercise to reduce insulin resistance and improve overall health
- Stress management techniques, such as yoga or meditation, to reduce stress and improve mental well-being
By using these methods together, women with PCOS can manage their symptoms better. This improves their quality of life.
Lifestyle Management for PCOS
Lifestyle management is key to easing PCOS symptoms and boosting health. By adopting healthy habits, women with PCOS can manage their condition better. This improves their quality of life.
Nutrition Strategies
Eating a balanced diet is vital for PCOS management. Nutrition strategies should include whole foods like veggies, fruits, whole grains, and lean proteins. These help control blood sugar and insulin levels.
- Eat foods high in omega-3s, like salmon and walnuts, to fight inflammation.
- Choose complex carbs, such as whole grains and legumes, to manage blood sugar.
- Reduce processed foods and sugars to lower insulin resistance.
Exercise Recommendations
Regular exercise is essential for PCOS management. Exercise recommendations include aerobic activities like brisk walking or cycling. Also, do resistance training to boost insulin sensitivity and health.
- Do at least 150 minutes of moderate-intensity aerobic exercise weekly.
- Do strength training twice a week to build muscle.
- Try high-intensity interval training (HIIT) for efficient calorie burn and better insulin sensitivity.
Stress Management and Sleep Quality
Managing stress and getting enough sleep are critical for PCOS care. Stress management techniques like mindfulness, meditation, and yoga can help reduce stress.
- Use relaxation techniques, such as deep breathing or progressive muscle relaxation, to calm the mind and body.
- Try to sleep 7-8 hours a night to regulate hormones and insulin sensitivity.
Weight Management Approaches
For many women with PCOS, weight management is a big challenge. A mix of dietary changes, regular exercise, and stress management can help achieve and keep a healthy weight.
Even a small weight loss of 5-10% can greatly improve PCOS symptoms. This includes better menstrual regularity and insulin sensitivity.
Long-term Health Implications of PCOS
PCOS affects more than just fertility. It also impacts metabolic, cardiovascular, and mental health. Knowing these risks is key to managing and reducing them.
Metabolic Risks: Diabetes and Insulin Resistance
Women with PCOS face a higher risk of insulin resistance and type 2 diabetes. Insulin resistance means the body’s cells don’t use insulin well, causing high blood sugar. This can lead to diabetes and is linked to PCOS’s hormonal imbalances.
- Increased risk of metabolic syndrome
- Higher likelihood of developing type 2 diabetes
- Importance of monitoring blood sugar levels
To tackle these risks, diet and exercise are vital. A balanced diet and regular exercise can boost insulin sensitivity.
Cardiovascular Considerations
PCOS raises the risk of heart diseases like hypertension and atherosclerosis. Hormonal and metabolic issues in PCOS contribute to these risks.
- Regular monitoring of blood pressure
- Lipid profile checks
- Lifestyle modifications to reduce cardiovascular risk
Managing cholesterol levels and blood pressure can lower cardiovascular risk for women with PCOS.
Endometrial Health and Cancer Risk
Women with PCOS face a higher risk of endometrial hyperplasia and cancer due to unbalanced estrogen. Regular gynecological check-ups and proper management are critical.
Mental Health Considerations
PCOS’s hormonal imbalances and physical symptoms can harm mental health. Anxiety and depression are common in women with PCOS.
- Importance of mental health support
- Access to counseling and psychological services
- Stress management techniques
Recognizing PCOS’s mental health aspects and providing support can improve women’s overall well-being.
Conclusion: Living Well with PCOS
PCOS is a complex condition that affects many aspects of a woman’s health. With the right management and support, women with PCOS can live healthy and fulfilling lives. It requires a care approach that tackles hormonal imbalances, menstrual issues, and fertility challenges.
Managing PCOS effectively means using medical treatments, making lifestyle changes, and getting emotional support. Women can better handle the challenges of PCOS by understanding it. Support from healthcare providers, family, and support groups is key in coping with the condition.
We stress the need for a holistic approach to managing PCOS. This includes nutrition strategies, exercise, and stress management. By adopting these measures, women with PCOS can reduce its impact on their health. This leads to a healthier and more active life.
FAQ
What is PCOS and how does it affect ovarian follicles?
PCOS, or Polycystic Ovary Syndrome, is a hormonal disorder. It affects the growth of ovarian follicles. This leads to many small, immature follicles in the ovaries. It can stop ovulation and affect fertility.
What are the characteristic ultrasound findings in PCOS?
Ultrasound findings in PCOS include many small follicles in both ovaries. These are called “multiple bilateral ovarian follicles” or “polycystic ovarian morphology.”
How does PCOS affect fertility, and what are the available treatment options?
PCOS can disrupt ovulation, affecting fertility. But, there are treatments like medications and IVF to help.
What are the hormonal imbalances associated with PCOS?
PCOS has hormonal imbalances. These include high androgen levels and insulin resistance. They can stop follicles from growing and ovulating.
What lifestyle changes can help alleviate PCOS symptoms?
Changes like good nutrition, exercise, stress management, and a healthy weight can help. They can ease PCOS symptoms and improve health.
What are the long-term health risks associated with PCOS?
Women with PCOS face risks like diabetes and heart disease. They may also have issues with endometrial health and mental well-being.
How is PCOS diagnosed, and what diagnostic tools are used?
PCOS is diagnosed with clinical evaluation, ultrasound, and blood tests. These tools check for ovarian changes and hormonal imbalances.
Can PCOS be treated with medication, and what are the options?
Yes, medication can treat PCOS. It helps with hormonal imbalances, improves fertility, and regulates menstrual cycles.
What is the prevalence of PCOS, and who is at risk?
PCOS affects about 1 in 10 women. Risk factors include genetics, environment, age, and ethnicity.
How do multiple ovarian follicles affect ovulation in PCOS?
Many small follicles in the ovaries can disrupt ovulation. This leads to irregular periods and fertility issues.
References
World Health Organization. PCOS: Ovarian Follicles, Fertility, and Women’s Health. Retrieved from https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7115104/










