Did you know that nearly 1 in 5 adults in the United States suffer from chronic pain? This pain is often linked to inflammatory conditions. It’s key to use inflammation imaging to detect inflammation and manage these conditions well.
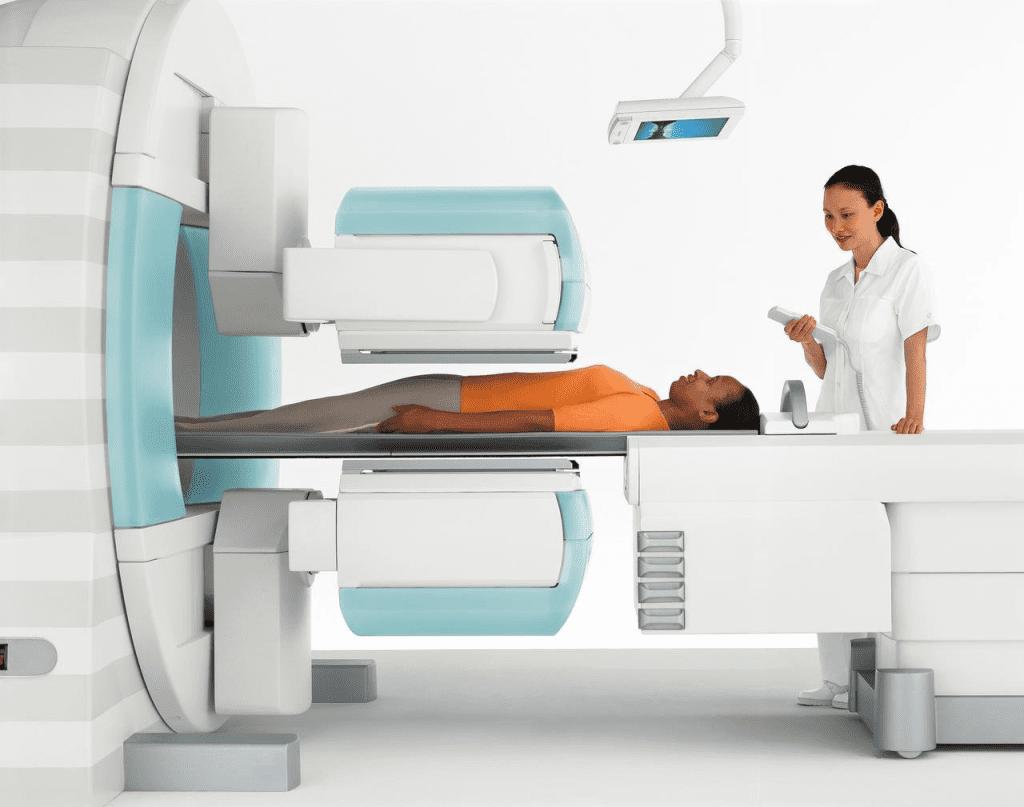
SPECT (Single Photon Emission Computed Tomography) scans are a type of nuclear medicine imaging. They can spot inflammation in the body. Studies show SPECT scans can find conditions like PSPS-T2 and SAPHO syndrome.
Healthcare pros use SPECT technology to see how much inflammation is there. This helps them make better diagnoses and treatment plans.
Key Takeaways
- SPECT scans can help detect inflammation in the body.
- Inflammatory conditions like PSPS-T2 and SAPHO syndrome can be identified using SPECT scans.
- Accurate detection of inflammation is key for good diagnosis and treatment.
- SPECT technology gives insights into inflammation presence and extent.
- Targeted treatment plans can be made based on SPECT scan results.
Understanding SPECT Scan Technology
SPECT scan technology is at the core of nuclear medicine. It greatly helps us find and manage inflammatory diseases. It uses small amounts of radioactive tracers that gather in inflamed areas.
Basic Principles of SPECT Imaging
SPECT scan technology works by detecting gamma rays from radioactive tracers. These tracers are made to find specific parts or processes in the body, like inflammation. The scanner moves around the patient, catching gamma rays from different sides to make detailed, three-dimensional images.
First, a SPECT tracer is given to the patient. This tracer is picked for its ability to find the target area or process. For inflammation, tracers that stick to inflammatory cells or gather in inflamed areas are used. The tracer sends out gamma rays, which the SPECT scanner catches.
How SPECT Differs from Other Nuclear Medicine Techniques
SPECT is different from other nuclear medicine methods, like PET, because it uses gamma rays instead of positrons. Both give insights into the body’s inner workings, but SPECT is great for nuclear imaging inflammation because it makes detailed images of specific areas.
A big plus of SPECT is it can look at multiple tracers at once. This is because it can tell different gamma ray energies apart. This is really helpful in complex cases where many processes need to be checked.
| Modality | Tracer Type | Primary Use |
| SPECT | Gamma-emitting tracers | Inflammation imaging, infection detection |
| PET | Positron-emitting tracers | Cancer staging, neurological disorders |
Choosing between SPECT and other imaging methods depends on the clinical question, the tracer type, and the needed information for patient care. For inflammation imaging, SPECT is a valuable tool. It gives insights that help in making treatment plans.
The Role of SPECT in Inflammation Imaging
SPECT can spot inflammation at the cellular level, marking a big step in medical imaging. Inflammation is a complex response to injury or infection. It involves immune cells and chemical mediators. Knowing this helps doctors diagnose and treat inflammatory conditions.
What Is Inflammation at the Cellular Level
Inflammation at the cellular level means immune cells like leukocytes and macrophages work together. They release cytokines and chemokines to start the inflammatory response. SPECT detects inflammation by finding specific biomarkers of this activity.
Inflammation can be either acute or chronic. Acute inflammation quickly brings immune cells to the injury or infection site. Chronic inflammation lasts longer and can damage tissues.
Biomarkers of Inflammation Detectable Through SPECT
SPECT scans find inflammation by looking for certain biomarkers. Key biomarkers include labeled white blood cells (WBCs) or leukocytes. Labeled WBC scans are great for spotting infection or inflammation in different body parts.
- Labeled WBCs: These are white blood cells with a radioactive tracer, making them visible on SPECT scans.
- Leukocyte scans: These use radiolabeled leukocytes to find inflammation or infection.
- Other biomarkers: SPECT can also spot other inflammation biomarkers, like cytokines and chemokines.
Using these biomarkers, SPECT is key in diagnosing and managing inflammation. It gives detailed images of inflammation. This helps doctors understand how severe it is and how to treat it.
SPECT Tracers Used for Inflammation Detection

SPECT imaging uses special tracers to find inflammation. These tracers are radioactive and build up in inflamed areas. This makes them visible for doctors to see.
Technetium-99m Based Tracers
Technetium-99m (Tc) tracers are popular for finding inflammation. They have the right half-life and gamma energy for SPECT scans.
Common Tc-based tracers include:
- 99mTc-hexamethylpropyleneamine oxime (99mTc-HMPAO) labeled leukocytes
- 99mTc-ciprofloxacin
Gallium-67 for Inflammation Imaging
Gallium-67 (Ga) citrate is used for finding inflammation, like in infections. It binds to proteins in inflamed areas.
Ga is helpful in diagnosing conditions like sarcoidosis and infections.
Emerging SPECT Tracers for Inflammation
New SPECT tracers are being developed to better detect inflammation. These tracers aim to be more accurate and specific.
| Tracer | Characteristics | Potential Use |
| Tc- labeled anti-TNF-α | Targets tumor necrosis factor-alpha | Imaging inflammatory conditions like rheumatoid arthritis |
| Tc-MDP | Binds to bone hydroxyapatite | Detecting bone inflammation and infection |
These new tracers could make SPECT imaging even better for finding inflammation.
Labeled White Blood Cell (WBC) Scans
Labeled White Blood Cell (WBC) scans are a key tool in nuclear medicine for finding inflammation. They work by labeling a patient’s white blood cells with a radioactive tracer. These cells are then injected back into the body. They gather in areas of inflammation, making it possible to spot them with SPECT imaging.
Process of Labeling Leukocytes
The first step in labeling leukocytes is to take white blood cells from a patient’s blood. These cells are then mixed with a radioactive tracer, like Technetium-99m HMPAO or Indium-111 oxine. This process labels the cells without changing how they work. After labeling, the cells are put back into the patient. They then go to areas of inflammation or infection.
The choice of radioactive tracer depends on the situation and what’s needed for the scan. For example, Technetium-99m HMPAO is often used because it works well and labels cells efficiently.
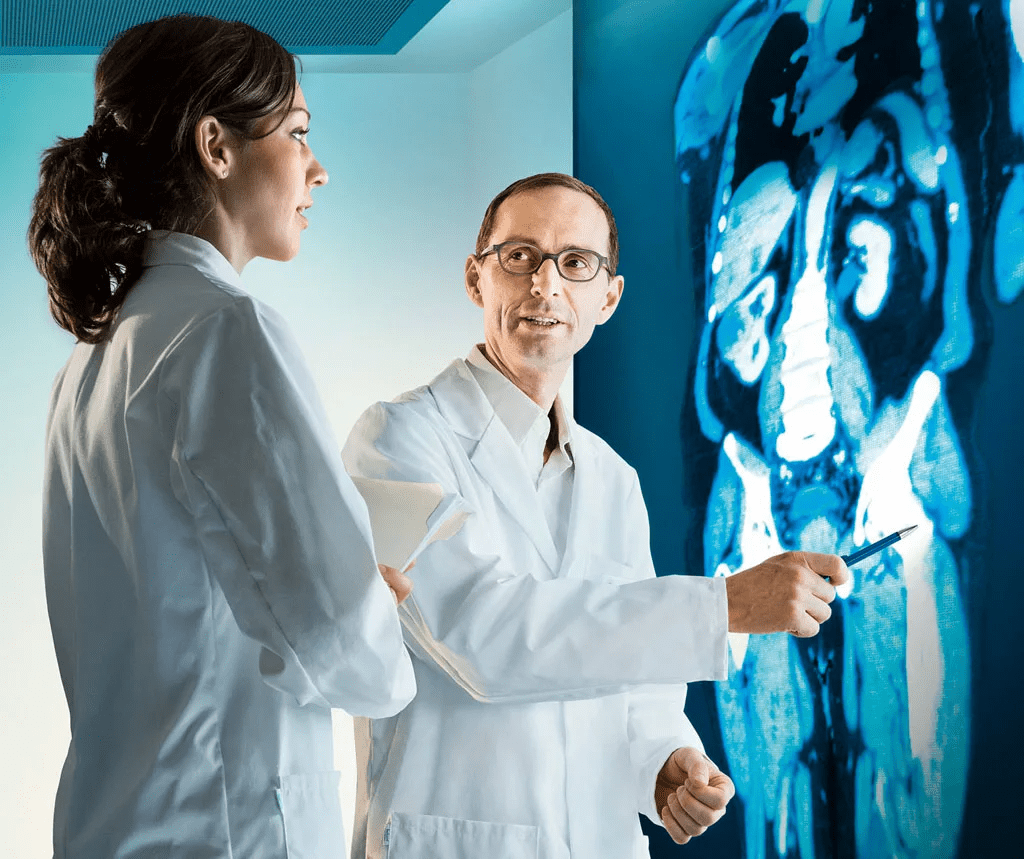
Interpretation of Labeled WBC SPECT Images
Understanding labeled WBC SPECT images is important. It involves knowing where labeled leukocytes usually go and what patterns show inflammation. Normally, these cells go to the spleen, liver, and bone marrow. But if they show up in other places, it might mean there’s inflammation or infection.
The amount and pattern of uptake are key to figuring out how bad the inflammation is. For example, if the uptake is focused in one area, it might mean a localized infection. But if it’s spread out, it could mean the inflammation is more widespread.
- Key factors in interpretation include:
- The intensity of tracer uptake
- The distribution pattern of the labeled cells
- Correlation with clinical symptoms and other diagnostic findings
Gallium Scans for Inflammatory Disease Detection
Gallium-67 citrate is used in SPECT imaging to spot and track inflammatory diseases. It’s been key in finding and handling different inflammatory issues, like infections and abscesses.
How Gallium Binds to Inflammatory Sites
Gallium-67 citrate sticks to inflammatory areas because of its attraction to certain proteins and cells. The tracer builds up in these areas, making them visible with SPECT imaging. But, it also goes to tumors and other non-inflammatory spots, so the images need careful looking at.
“The power of gallium scans to spot inflammation at the cell level has made them a must-have in nuclear medicine,” say experts.
Clinical Applications of Gallium SPECT
Gallium SPECT is used in many ways, mainly for finding and watching inflammatory diseases. It helps spot abscesses, infections, and some inflammatory disorders. Gallium scans are good at showing how much inflammation there is and if treatments are working.
- Detecting abscesses and infections
- Monitoring inflammatory disease activity
- Assessing response to treatment
Gallium SPECT is a big deal in medical practice for dealing with inflammatory conditions. It gives clear pictures of where inflammation is, helping doctors manage patients with tough inflammatory diseases.
SPECT Imaging for Infection Detection
SPECT technology is key in finding infections. It gives clear images that show the difference between infection and inflammation.
Differentiating Between Infection and Inflammation
It’s hard to tell infection from inflammation in medical practice. SPECT imaging helps by using special tracers for infected tissues. For example, labeled white blood cell (WBC) scans are great for spotting infection areas.
These scans work by tagging the patient’s white blood cells with a radioactive tracer. This tracer goes to infected areas. This makes SPECT imaging better at finding infections.
Key benefits of using labeled WBC scans include:
- High sensitivity in detecting acute infections
- Ability to localize the infection site accurately
- Useful in monitoring response to treatment
Sensitivity and Specificity in Infection SPECT
The success of SPECT imaging in finding infections depends on the tracer and imaging method. Research shows labeled WBC SPECT is very good at spotting infections. This is true for infections in prosthetic joints and bone infections.
To make diagnosis even better, SPECT imaging can be paired with CT scans. This combo helps pinpoint infection locations and gives a fuller picture.
Advantages of hybrid SPECT/CT imaging include:
- Improved anatomical localization of infection sites
- Enhanced diagnostic confidence
- Better differentiation between infection and other pathologies
Bone SPECT for Inflammatory Conditions
Bone SPECT imaging is a key tool for spotting and tracking bone and joint inflammation. It uses special tracers that light up where inflammation is happening. This gives doctors a clear picture of how bad the inflammation is.
The way bone scan uptake works in inflammation is quite complex. Bone SPECT tracers stick to areas where bone is changing a lot. This usually means there’s inflammation.
Mechanism of Bone Scan Uptake in Inflammation
Bone SPECT tracers light up in inflamed areas because of more blood flow and bone activity. This makes the inflamed spots show up on the scan.
| Mechanism | Description |
| Increased Blood Flow | Inflammation brings more blood to the area, leading to more tracer uptake. |
| Bone Turnover | Inflammation also makes bone turnover go up, adding to the tracer buildup. |
Clinical Applications in Rheumatology and Orthopedics
Bone SPECT is very useful in rheumatology and orthopedics. It helps diagnose and keep an eye on diseases like rheumatoid arthritis and osteomyelitis. Spotting inflammation early means doctors can act fast to manage it.
Using Bone SPECT in medicine has made diagnosing better and helped doctors decide on treatments. It’s also great for tracking how diseases progress and how well treatments work. This makes it a key tool for managing bone inflammation.
Neuroinflammation Assessment with SPECT
Using SPECT to check for neuroinflammation involves special tracers. These tracers go to areas of inflammation, helping doctors diagnose and track neurodegenerative diseases. This method offers insights into brain inflammation.
Brain SPECT Techniques for Inflammatory Disorders
Brain SPECT imaging uses radiopharmaceuticals that find inflammation. Technetium-99m labeled tracers are often chosen because they work well and stick to inflammatory areas. The right tracer depends on the type of inflammation being studied.
First, the tracer is given to the patient. Then, SPECT imaging is done. The images show where the tracer is most active, showing inflammation. This helps doctors understand and diagnose neurological issues.
Applications in Neurodegenerative Diseases
SPECT imaging is key for diseases like Alzheimer’s, Parkinson’s, and multiple sclerosis. It helps doctors see inflammation and track how the disease progresses. This can help find new treatments.
Brain SPECT also helps monitor how well treatments work. Quantitative analysis of SPECT images shows if anti-inflammatory treatments are effective. This helps doctors adjust treatment plans for each patient.
Also, SPECT helps researchers understand neurodegenerative diseases better. By studying inflammation, they can create better treatments. This research is vital for finding new ways to fight these diseases.
Cardiac SPECT in Inflammatory Heart Conditions
Cardiac SPECT imaging helps us see heart inflammation. It’s a big step forward in cardiology.
This imaging is key for spotting and tracking heart inflammation. It helps doctors make better treatment plans.
Myocarditis and Pericarditis Imaging
Myocarditis and pericarditis are hard to diagnose because their symptoms are not clear. Cardiac SPECT imaging spots these heart issues by showing where inflammation is.
Cardiac SPECT also shows how well the heart works. This helps doctors understand how bad the inflammation is and how it affects the heart.
Cardiac Sarcoidosis Detection
Cardiac sarcoidosis is when inflammation and scarring happen in the heart. Finding out if the heart is involved is very important. Cardiac SPECT helps find these problems in the heart.
Using Cardiac SPECT for cardiac sarcoidosis means doctors can catch it early. This helps patients get better faster.
Comparing SPECT to Other Inflammation Imaging Modalities
Several methods are used to image inflammation, each with its own strengths and weaknesses. SPECT (Single Photon Emission Computed Tomography) is a nuclear medicine technique used to detect inflammation. To see how well it works, we need to compare it with other methods like PET, MRI, and CT.
SPECT vs. PET for Inflammation
SPECT and PET are both nuclear medicine techniques that use tracers to see metabolic processes. PET is generally considered to have higher sensitivity and resolution than SPECT, making it better for spotting subtle inflammation changes. But SPECT is more available and cheaper than PET.
Choosing between SPECT and PET depends on the clinical situation and available resources.
SPECT vs. MRI for Inflammatory Disease
MRI is a non-invasive imaging method that shows soft tissue well, making it great for inflammatory diseases. MRI does not involve ionizing radiation, a big plus over SPECT and PET. But MRI might not catch all inflammation, like the molecular kind.
SPECT vs. CT for Inflammation Detection
CT scans are used to see anatomical changes due to inflammation, like damage or abscesses. While CT is good for detailed anatomy, it doesn’t offer the functional info SPECT does. SPECT can spot metabolic changes in inflammation before CT can see anatomical changes.
| Modality | Sensitivity for Inflammation | Advantages | Limitations |
| SPECT | High | Functional information, widely available | Lower resolution compared to PET |
| PET | Very High | High sensitivity, high resolution | Expensive, less widely available |
| MRI | Moderate to High | No ionizing radiation, excellent soft tissue contrast | May not detect molecular changes |
| CT | Low to Moderate | Detailed anatomical information | Lacks functional information |
Limitations of SPECT in Inflammation Imaging
SPECT has its challenges in imaging inflammation, like low spatial resolution and specificity. Despite its progress, these issues can make it less reliable for detecting inflammation.
Spatial Resolution Challenges
SPECT’s spatial resolution is a big challenge. It’s not as sharp as MRI or CT scans. This makes it hard to spot small or faint inflammatory areas.
Factors contributing to spatial resolution challenges in SPECT include:
- Collimator design and sensitivity
- Detector technology and resolution
- Reconstruction algorithms and filtering
New SPECT cameras with better resolution are helping. But, finding the right balance between sensitivity and resolution is key.
Specificity Issues in Complex Cases
In complex cases, SPECT’s specificity is a big issue. SPECT tracers can bind to many tissues, not just inflamed ones. This makes it hard to know what’s really inflamed.
| Challenge | Description | Impact on Inflammation Imaging |
| Lack of Specificity | SPECT tracers accumulate in non-inflammatory tissues | False positives, reduced diagnostic accuracy |
| Complex Anatomy | Difficulty in interpreting images in complex anatomical regions | Increased risk of misinterpretation |
| Co-existing Conditions | Presence of multiple conditions simultaneously | Challenges in attributing tracer uptake to specific conditions |
In complex cases, SPECT’s lack of specificity makes diagnosis tough. It’s hard to tell if something is inflamed or not. This is why doctors need to look at images carefully and use other tests too.
In summary, SPECT is useful for seeing inflammation, but we must know its limits. Research and new tech aim to improve SPECT. This will help doctors better detect and treat inflammation.
Clinical Interpretation of Inflammatory SPECT Findings
Understanding SPECT images for inflammation is complex. It needs a deep grasp of the tech and the disease. Accurate reading is key for treating inflammatory conditions well.
Quantitative Analysis Techniques
Quantitative analysis is key for better SPECT findings. It measures tracer uptake in specific areas. This is compared to a reference area or uses standardized uptake values (SUVs).
This method gives a clear view of inflammation. It helps track disease changes and treatment effects over time.
- Region-of-interest (ROI) analysis quantifies tracer uptake in specific areas.
- Standardized uptake values (SUVs) offer a way to compare uptake across scans and patients.
Pitfalls in Interpretation
Even with SPECT’s progress, challenges remain. These include artifacts from motion or attenuation, nonspecific uptake, and differentiating inflammation from other diseases.
To overcome these, SPECT results should be matched with symptoms, lab tests, and other images. A team effort from nuclear medicine, radiology, and doctors improves accuracy.
Important steps for accurate interpretation include:
- Knowing SPECT’s limits.
- Recognizing and understanding artifacts.
- Linking SPECT results with other diagnostic info.
By using a detailed and careful approach, doctors can get the most from SPECT for diagnosing inflammation.
Future Directions in SPECT Inflammation Imaging
The field of SPECT inflammation imaging is on the verge of a big change. This is thanks to new tracer technology and hybrid imaging methods. As we learn more, we can better detect and track inflammation. This could lead to more accurate diagnoses and better care for patients.
New Tracer Development
Creating new SPECT tracers is key to improving inflammation imaging. Researchers have made tracers that focus on specific inflammation markers. This makes imaging more precise.
Emerging Tracers: New tracers are being developed to spot inflammation early. This could help treat problems before they get worse. Early detection could greatly improve treatment results.
| Tracer | Target | Clinical Application |
| Technetium-99m labeled tracers | Inflammatory cells | Infection and inflammation imaging |
| Gallium-67 | Inflammatory sites | Detecting inflammatory diseases |
| Newly developed tracers | Specific biomarkers | Early detection of inflammation |
Hybrid Imaging Approaches
Hybrid imaging combines SPECT with CT or MRI. This mix is becoming more common in inflammation imaging. It lets us see both how things work and their structure, making diagnosis better.
Benefits of Hybrid Imaging: By combining SPECT with other imaging, we can better pinpoint where inflammation is. This gives us a fuller picture of the disease.
The future of SPECT in inflammation imaging looks promising. With ongoing research and development, we can expect big improvements in this field.
Conclusion
SPECT imaging is now a key tool in medicine for spotting inflammation. It uses special tracers and methods to help doctors find and track inflammation. This allows for quick action to help patients.
SPECT imaging is used in many ways, from finding infections to studying brain inflammation. As SPECT technology gets better, so will its use in helping patients. This will make care even better for those with inflammatory diseases.
In short, SPECT imaging is very important in today’s medicine. It’s a precise way to find inflammation. As it keeps getting better, it will play an even bigger role in treating patients with inflammatory diseases.
FAQ
What is a SPECT scan and how does it show inflammation?
A SPECT scan is a way to see inside the body using a tiny bit of radioactive material. It helps doctors see how different parts of the body work, like where there’s inflammation. It does this by finding special markers that show up in inflamed areas.
What are the different types of SPECT tracers used for inflammation detection?
A SPECT scan is a way to see inside the body using a tiny bit of radioactive material. It helps doctors see how different parts of the body work, like where there’s inflammation. It does this by finding special markers that show up in inflamed areas.
How does a labeled white blood cell scan work?
A labeled white blood cell scan tags a patient’s white blood cells with a radioactive tracer. Then, these cells are put back into the patient. A SPECT scan follows to find where these cells have gathered, showing inflammation or infection.
What is the role of gallium scans in detecting inflammatory diseases?
Gallium scans use a radioactive tracer that sticks to inflamed areas. This makes them great for finding diseases like sarcoidosis and certain infections. Gallium SPECT is very helpful in these cases.
Can SPECT imaging differentiate between infection and inflammation?
SPECT imaging can sometimes confuse infection with inflammation. This is because both can show up as increased activity. But, some tracers are better at finding infections, while others, like gallium-67, can show up in both.
How does bone SPECT help in diagnosing inflammatory conditions?
Bone SPECT can spot inflammation by looking at bone activity. It’s really useful in checking for conditions like osteoarthritis and rheumatoid arthritis. This helps doctors understand what’s going on in the bones.
What are the limitations of SPECT in inflammation imaging?
SPECT has some big challenges. It can struggle to see small details and might not always know what it’s looking at. This can make it hard to tell different types of inflammation apart or to know if it’s something else.
How is SPECT compared to other inflammation imaging modalities like PET, MRI, and CT?
SPECT has its own strengths and weaknesses compared to other imaging methods. It’s more common and cheaper than PET but might not be as accurate. MRI and CT are better at showing what’s going on in the body but might miss inflammation signs.
What are the future directions in SPECT inflammation imaging?
The future of SPECT imaging looks bright. New tracers are being made to improve how well it works. Also, combining SPECT with other imaging like CT or MRI could give even better views of inflammation.
How is SPECT used in assessing neuroinflammation?
SPECT helps spot neuroinflammation by looking at brain activity. It’s really useful for diagnosing and tracking neurodegenerative diseases. This helps doctors understand what’s happening in the brain.
Can SPECT be used for cardiac inflammation imaging?
Yes, SPECT is great for looking at the heart for inflammation. It’s very helpful in finding and tracking conditions like myocarditis, pericarditis, and cardiac sarcoidosis.
References
- Nishikawa, Y., et al. (2022). Diagnostic performance of quantitative Ga-SPECT/CT for detecting infection and inflammation. European Journal of Hybrid Imaging, 6(1), 11. https://ejhi.springeropen.com/articles/10.1186/s41824-022-00148-z























