Finding metastasis is key in cancer care. Many cancer patients struggle with cancer spreading. So, quick and right diagnosis is very important.
They help spot cancer spread. This guides doctors in making treatment plans.
Key Takeaways
- CT scans are vital in detecting metastasis in cancer patients.
- Advanced imaging technology aids in accurate metastatic cancer diagnosis.
- Early detection of cancer spread improves treatment outcomes.
- CT scans help in monitoring the progression of metastatic cancer.
- Timely diagnosis is key for effective cancer treatment.
Understanding Metastasis and Medical Imaging
Finding cancer metastasis is key in fighting cancer. It helps doctors decide on treatments and improves patient chances of recovery. Metastasis happens when cancer cells move from where they started to other parts of the body. This makes treatment harder and changes how well a patient might do.
What is metastasis in cancer progression
Metastasis is a complex process. It starts with cancer cells breaking away from the main tumor. They then move into nearby tissues, get into the blood or lymph, and spread to other organs. This is a big part of how cancer grows and affects treatment plans.
The process of metastasis involves many changes in the cancer cells. These changes help them survive and grow in new places. Knowing about these changes is important for finding and treating cancer better.
The importance of early detection
Finding metastasis early is very important. It helps patients live longer and better. For some cancers, like bladder cancer, watching closely for signs of return is a must. New imaging tools help find metastasis early.
Early detection has many benefits:
- Starting treatment on time
- Better chances of recovery
- Living a better life with targeted treatments
Overview of imaging modalities for metastasis
There are many ways to find metastasis, each with its own strengths and weaknesses. These include:
| Imaging Modality | Key Features | Applications in Metastasis Detection |
| CT Scan | High-resolution cross-sectional imaging | Liver, lung, and lymph node metastases |
| MRI | Excellent soft tissue contrast | Brain, liver, and bone metastases |
| PET/CT | Functional imaging combined with anatomical detail | Whole-body assessment for metastatic disease |
Choosing the right imaging tool depends on where the metastasis might be, the type of cancer, and the patient’s situation. Knowing about these tools is key for accurate diagnosis and planning treatment.
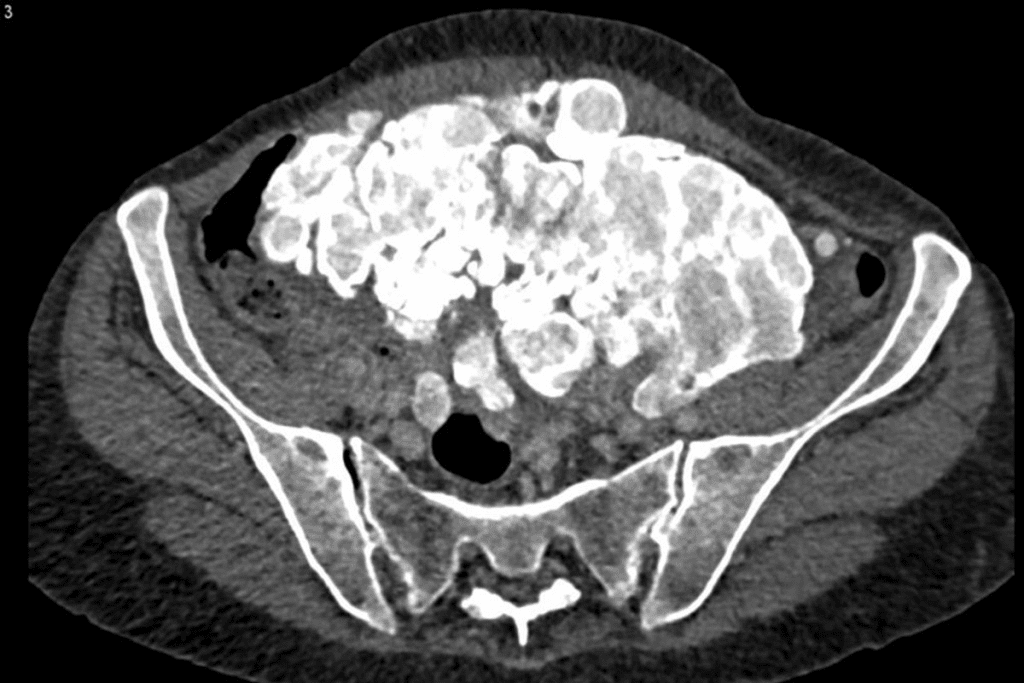
How CT Scan Detect Metastasis Cancer Spread
CT scans are key in finding metastasis. They use X-rays to make detailed images of the body. This helps spot cancer spreading to different parts.
Basic Principles of Computed Tomography
CT scans use X-rays to see inside the body. They show more detail than regular X-rays by taking images in slices. This is done by moving the X-ray source and detectors around the body.
The data from these scans is turned into images by computers. These images can be seen in different ways, like from the side or top. This helps doctors see tumors in various parts of the body. The cross-sectional imaging of CT scans is great for finding metastasis.
Cross-Sectional Imaging Advantages
CT scans have big benefits for finding metastasis. They let doctors:
- See the size and where metastatic lesions are.
- Check if tumors are touching other parts.
- Watch how tumors change size over time, which helps see how well treatments are working.
These benefits make CT scans very useful for tracking cancer.
Density Differences in Metastatic Lesions
Metastatic lesions can be seen on CT scans because they are different in density from normal tissue. Their density can tell doctors what they are; for example, some may look darker because they are dead tissue or lighter if they have calcium.
Using contrast-enhanced CT imaging makes lesions even clearer. Contrast agents, like iodine, are given through an IV. They show up differently in tumors than in healthy tissue, making tumors stand out on the images.
Using contrast in CT scans has many benefits for finding metastasis:
- It helps find lesions, like in the liver and spleen.
- It shows how tumors fit with the surrounding tissue better.
- It helps figure out what a lesion is by how it looks on the scan.
Types of CT Scans Used for Metastasis Detection

CT scans play a key role in finding metastasis. They come in different types, each suited for specific needs. The right CT scan depends on where the metastasis is likely and the patient’s health.
Non-contrast CT scans
Non-contrast CT scans don’t use contrast agents. They’re good for spotting some metastases, like in the lungs and bones. Non-contrast CT is often used for initial assessments or when contrast agents are contraindicated. For example, they can spot lung metastases by showing nodules or masses in the lung tissue.
Contrast-enhanced CT imaging
Contrast-enhanced CT imaging uses a contrast agent to show tissue differences. It’s great for finding metastases in organs like the liver. Contrast-enhanced CT scans are also valuable for assessing the vascularity of tumors and their relationship to surrounding structures. For instance, in liver metastases, it can show the enhancement patterns of metastatic lesions.
Multiphase CT protocols
Multiphase CT protocols scan the same area multiple times after contrast agent. This is good for organs like the liver and kidneys. Multiphase CT can help identify the specific characteristics of metastatic lesions, such as their enhancement patterns and washout characteristics. It’s useful for spotting hypervascular metastases, seen in some cancers.
Knowing about the different CT scans helps doctors pick the best one for each patient. This approach improves diagnosis and helps plan better treatments.
Common Sites of Metastasis Detected by CT
CT scans are key in finding cancer spread in organs like the liver, lungs, and bones. They help doctors know how far cancer has spread and plan treatment. This is very important for cancer care.
Liver Metastases Detection
The liver is often where cancer spreads to, mainly from the stomach and intestines. CT scans can spot liver metastases by showing them against normal liver. Contrast-enhanced CT imaging makes these spots clearer.
Liver metastases look darker on non-contrast CT scans. But, they show up better on scans with contrast. Using multiphase CT protocols helps catch these lesions by showing how they change with contrast.
Lung Metastases Identification
Lung metastases are common in cancer spread. CT scans of the chest are very good at finding these, even small ones. They give detailed images of lung nodules.
Non-contrast CT scans usually work well for lung metastases because they contrast well with lung tissue. But, sometimes, scans with contrast are needed to see how these lesions relate to nearby tissues.
Bone Metastases Visualization
Bone metastases happen in cancers like breast, prostate, and lung. CT scans can spot these by showing changes in bone density and structure. While not as good as some other tests, CT is useful for looking at bone and soft tissues.
CT scans are great for checking if bones might break from cancer and for planning treatments like radiation or surgery.
Lymph Node Metastases Assessment
Lymph node metastases are key in cancer staging. They show cancer has spread. CT scans can check lymph nodes by looking at their size and shape. Big lymph nodes might mean cancer has spread.
Contrast-enhanced CT is better for looking at lymph nodes. It helps tell them apart from blood vessels. Checking lymph nodes on CT scans is important for knowing how far cancer has spread and for treatment planning.
Brain Metastases and CT Imaging
Brain metastases are a big challenge in cancer care. CT scans are key for finding them. It’s important to know how well different imaging methods work.
Limitations of CT for Brain Metastases
CT scans are fast and easy to get, but they have limits. They struggle to show details in soft brain tissues. This can lead to missed or wrong diagnoses.
CT scans also face issues with artifacts. These can hide or distort images. This makes it hard to see tumors clearly.
When Contrast is Essential
Adding contrast agents helps CT scans spot brain metastases better. It shows where the blood-brain barrier is broken. But, CT scans might not find small or hard-to-reach tumors as well as MRI.
CT versus MRI for Brain Metastases
For finding brain metastases, MRI is better than CT scans. MRI can see small tumors and soft tissues better. But, CT scans are useful in emergencies or when MRI can’t be used.
Choosing between CT and MRI depends on the situation. It’s about the patient’s needs and the tumor’s details. Knowing each method’s strengths and weaknesses helps doctors care for patients better.
Accuracy and Limitations of CT in Metastasis Detection
It’s key to know how well CT scans find metastases for cancer care. CT scans help spot metastatic lesions, but their success depends on where and how big these lesions are.
Sensitivity Rates for Different Metastatic Sites
CT scans work better in some places than others. They’re good at finding liver and lung metastases. But, they’re not as good at finding them in other parts of the body.
| Organ | Sensitivity of CT Scan |
| Liver | 85-90% |
| Lung | 80-85% |
| Lymph Nodes | 70-75% |
Size Threshold for Detection
The size of metastatic lesions matters for CT scans. Lesions over 5 mm are usually seen. But, this can change based on where they are and the CT technology used.
False Negatives and Missed Metastases
False negatives happen for a few reasons. Small size, poor contrast, or hard-to-image areas can hide metastases.
Micrometastases and CT Limitations
Micrometastases are tiny and hard for CT scans to find. Current CT tech struggles to spot these small lesions. This might lead to cancer being under-staged.
Improving CT scan accuracy for finding metastases needs better tech. New contrast agents and more sensitive scanners are needed. Also, using CT scans with other imaging methods can help get a clearer picture.
CT Scan Compared to Other Imaging Modalities
Many imaging methods are used to find metastasis, each with its own benefits and drawbacks. The right choice depends on the cancer type, where the metastasis might be, and the patient’s health.
CT versus PET and PET/CT
CT scans are often compared to PET (Positron Emission Tomography) and PET/CT. PET/CT combines PET’s functional info with CT’s detailed images. It’s great for spotting cancer cells that are active.
PET/CT Advantages: It gives both functional and anatomical details, making it very good at finding active cancer cells.
| Imaging Modality | Strengths | Weaknesses |
| CT Scan | High-resolution anatomical images, quick and widely available | Limited functional information, may miss small metastases |
| PET/CT | Combines functional and anatomical information, highly sensitive for active cancer | Higher radiation exposure, more expensive, may not be as widely available |
CT versus MRI for Specific Metastases
MRI (Magnetic Resonance Imaging) is also a strong tool for finding metastasis, mainly in soft tissues. For some cancers, MRI is better than CT because it shows soft tissues better.
MRI Advantages: It’s great at showing soft tissue details, helping find metastases in the brain, liver, and other organs.
Ultrasound and Metastasis Detection
Ultrasound is a non-invasive, common way to find metastasis, like in the liver and other abdominal areas. But, its success depends on the person doing the scan and it might not find small metastases as well as CT or MRI.
Nuclear Medicine Techniques
Nuclear medicine, like bone scans, is used to find metastasis, mainly in bones. It uses tiny amounts of radioactive material to show where bone is changing.
Bone Scan Advantages: It’s very good at finding bone metastases, helping see how much of the skeleton is involved.
In summary, picking the right imaging method for finding metastasis depends on many things, like the cancer type and where the metastasis might be. Each method has its own good points and bad points. Sometimes, using more than one method is needed to get a clear picture for treatment planning.
The Role of CT in Cancer Staging and Metastatic Workup
CT scans are key in oncology for checking cancer stages and finding metastasis. This part explains how CT scans help in cancer staging and finding metastasis.
TNM Classification and CT Findings
The TNM system is used to stage cancer. It looks at the tumor size (T), nearby lymph nodes (N), and if it has spread (M). CT scans are vital for TNM staging by showing detailed images of the tumor and its spread.
CT findings are key in determining the T stage by measuring the tumor size and seeing if it has invaded nearby tissues. For the N stage, CT scans spot lymph node involvement by looking for enlarged nodes. For the M stage, CT scans find metastases in organs like the liver, lungs, and bones.
Whole-Body CT for Complete Staging
Whole-body CT scans image from the skull to the mid-thigh. They give a full view of the cancer’s spread. This is great for finding distant metastases and seeing the disease’s total burden.
| Advantages of Whole-Body CT | Clinical Implications |
| Comprehensive assessment of cancer spread | Accurate staging and treatment planning |
| Detection of distant metastases | Informed decision-making regarding surgery, chemotherapy, or radiation therapy |
Integration with Clinical Assessment
CT scan info is mixed with clinical assessment for a full disease picture. This includes patient history, physical exam, and lab tests. It makes sure treatments fit the patient’s needs.
Clinical correlation is key to check CT scan results and handle any false negatives. This mix boosts cancer staging and metastatic workup accuracy. It helps guide treatment choices.
Confirming Metastases Beyond CT Imaging
CT scans are key in spotting possible metastases. But, a full check-up needs more than just scans. It’s important to confirm these findings to plan the best treatment.
CT-guided Biopsy Procedures
CT-guided biopsy helps confirm metastases. It’s a small procedure where a CT scan guides a needle into the suspected area. Then, the tissue is checked to see if it’s cancer.
Benefits of CT-guided biopsy include:
- High accuracy in sampling the target lesion
- Minimally invasive, reducing the risk of complications
- Ability to perform the procedure under local anesthesia
Tissue Sampling Techniques
Getting a clear diagnosis of metastasis is key. Methods like fine-needle aspiration biopsy (FNAB) and core needle biopsy (CNB) are used. The right method depends on the tumor’s location and the patient’s health.
| Biopsy Technique | Description | Advantages |
| CT-guided Biopsy | Uses CT imaging to guide needle placement | High accuracy, minimally invasive |
| Fine-needle Aspiration Biopsy (FNAB) | Involves using a thin needle to aspirate cells | Less invasive, quick recovery |
| Core Needle Biopsy (CNB) | Uses a larger needle to obtain a tissue core | Provides more tissue for histological examination |
Correlation with Tumor Markers and Blood Tests
Tumor markers and blood tests are also vital. They help confirm metastases and track how the disease is progressing. Some cancers have specific markers in the blood.
For example, high levels of prostate-specific antigen (PSA) might mean prostate cancer has spread. Carcinoembryonic antigen (CEA) levels are watched in colorectal cancer patients. Blood tests also check the patient’s overall health and side effects from treatment.
By using CT scans, biopsy results, and blood tests, doctors can make better diagnoses. This helps in creating targeted treatment plans for patients with suspected metastases.
Monitoring Treatment Response with CT Scans
CT scans are key in managing cancer. They give detailed images that help doctors see how tumors change. This is important for knowing if treatment is working.
RECIST Criteria for Measuring Response
The Response Evaluation Criteria in Solid Tumors (RECIST) is a standard for cancer treatment response. It uses CT scans to measure tumor size changes. The criteria have four categories: complete response, partial response, stable disease, and progressive disease.
| Response Category | RECIST Criteria |
| Complete Response | Disappearance of all target lesions |
| Partial Response | At least a 30% decrease in the sum of diameters of target lesions |
| Stable Disease | Neither sufficient shrinkage to qualify for partial response nor sufficient increase to qualify for progressive disease |
| Progressive Disease | At least a 20% increase in the sum of diameters of target lesions, with an absolute increase of at least 5 mm, or the appearance of new lesions |
Evaluating Chemotherapy Effectiveness
CT scans help check if chemotherapy is working. A smaller tumor size means the treatment is effective. But, if the tumor grows or new ones appear, it might not be working.
“The use of CT scans to monitor treatment response has revolutionized the field of oncology, enabling healthcare providers to make data-driven decisions regarding treatment continuation or modification.”
” Expert Opinion
Assessing Immunotherapy and Targeted Therapy Response
CT scans also help check how well immunotherapy and targeted therapy work. Immunotherapy might first make tumors look bigger due to inflammation. Then, the tumors might shrink.
Challenges in Interpreting Post-Treatment Changes
It can be hard to understand changes after treatment on CT scans. This is because of inflammation, fibrosis, and necrosis. These can look like tumor changes. So, doctors need to look at the whole picture and might use other imaging too.
In summary, CT scans are very important in tracking cancer treatment. They help doctors see how tumors are changing. By using standards like RECIST and understanding different treatments, doctors can make better choices for their patients.
Surveillance CT Protocols for Metastatic Disease
Surveillance CT scans are key in tracking how metastatic disease grows and how well treatments work. They help spot changes in tumor size and spread. This information guides doctors in making treatment plans.
Frequency of Follow-up Scans
The timing of follow-up CT scans depends on the cancer type, treatment, and patient health. Scans are usually done every 3 to 6 months. This helps track disease growth and treatment success.
Factors influencing the frequency of scans include:
- Tumor type and aggressiveness
- Stage of disease
- Treatment modality (e.g., chemotherapy, immunotherapy)
- Patient’s overall health and response to treatment
Duration of Surveillance
The length of time for surveillance CT scans varies. It depends on the risk of disease coming back. For many cancers, scans are needed for years after treatment. The scan frequency may slow down if the patient stays cancer-free.
Guidelines for surveillance duration:
| Cancer Type | Typical Surveillance Duration | Frequency of CT Scans |
| Colorectal Cancer | 5 years | Every 6-12 months |
| Breast Cancer | 5-10 years | Every 12 months |
| Lung Cancer | 2-5 years | Every 3-6 months |
Radiation Exposure Considerations
CT scans add up radiation over time. This is a worry because it might raise the risk of getting cancer again. So, the good of scanning must be weighed against the risks.
Strategies to minimize radiation exposure:
- Using low-dose CT protocols
- Limiting the number of scans to the minimum necessary
- Employing alternative imaging modalities when appropriate
Risk-Benefit Analysis of Repeated Scanning
It’s important to do a detailed risk-benefit check for each patient. This looks at the benefits of early detection against the risks of radiation and the emotional impact of frequent scans.
Healthcare providers can create good surveillance CT plans. These plans help patients with metastatic disease while keeping risks low.
Future Advances in CT Technology for Metastasis Detection
The future of finding metastasis is bright with new CT technologies. These advancements bring us closer to detailed and precise diagnoses.
As cancer treatments get better, so does CT imaging. New technologies are set to change how we detect and manage metastasis.
Dual-Energy CT Applications
Dual-energy CT (DECT) is a big step forward. It takes images at two energy levels at once. This helps spot metastatic lesions better.
Benefits of DECT include:
- Improved lesion detection and characterization
- Enhanced visualization of iodine, helping in the assessment of tumor vascularity
- Better differentiation between various tissue types
| DECT Application | Clinical Benefit |
| Lesion Detection | Improved sensitivity for metastatic lesions |
| Tissue Characterization | Better differentiation between tumor types |
| Tumor Vascularity Assessment | Enhanced visualization of iodine uptake |
Artificial Intelligence and Radiomics
AI and radiomics are changing CT imaging in oncology. AI looks at lots of data to find patterns and predict outcomes. This is beyond what humans can do.
Key applications include:
- Automated detection and segmentation of metastatic lesions
- Predictive modeling for treatment response
- Enhanced diagnostic accuracy through quantitative imaging features
Improved Contrast Agents and Protocols
New contrast agents and protocols are making CT scans better for finding metastasis. These advancements include safer and more targeted agents.
Improvements include:
- Enhanced contrast between tumor and normal tissue
- Reduced toxicity and improved patient safety
- Tailored contrast agents for specific tumor types
Integration with Molecular Imaging
CT will soon work with molecular imaging. This mix of anatomical and functional imaging gives a deeper look at metastasis.
Benefits of integration include:
- Enhanced diagnostic accuracy through combined anatomical and functional information
- Improved assessment of tumor biology and behavior
- Better guidance for targeted therapies
Conclusion
Computed Tomography (CT) scans are key in finding where cancer has spread. They help doctors spot cancer in other parts of the body. This makes it easier to plan treatments that work best.
Thanks to CT scans, doctors can now predict how well a patient will do better. They can see how far the cancer has spread early on. This helps doctors choose the best treatment.
CT scans also help in making decisions about care for patients with cancer that has spread. They improve the patient’s quality of life. Using CT scans in cancer care has changed how we manage cancer that has spread.
FAQ
Can a CT scan detect metastasis?
Yes, CT scans are used to find metastasis, like in the liver, lungs, and lymph nodes. They show detailed images that help spot metastatic lesions.
How accurate are CT scans in detecting metastasis?
CT scans’ accuracy in finding metastasis depends on the size and location of the lesions. They’re good at spotting larger metastases but might miss smaller ones.
What are the limitations of CT scans in detecting brain metastases?
CT scans struggle with finding small brain metastases or those in areas with lots of artifacts. MRI is better at this.
How do CT scans compare to PET scans in detecting metastasis?
CT scans show detailed anatomy, while PET scans reveal metabolic activity. PET/CT combines both, giving a fuller picture.
Can CT scans be used to monitor treatment response in metastatic disease?
Yes, CT scans are used to check how well treatment is working in metastatic disease. They help see if tumors are getting smaller or changing.
How often should surveillance CT scans be performed in patients with metastatic disease?
The timing of surveillance CT scans varies based on the cancer type, treatment, and other factors. Scans are usually done every 3-6 months to track disease changes.
What are the risks associated with repeated CT scans?
Repeated CT scans increase radiation exposure, which can harm. But, the benefits of tracking treatment and disease progression often outweigh these risks.
Can CT-guided biopsy be used to confirm metastases?
Yes, CT-guided biopsy is a safe way to confirm metastases. It uses CT images to guide the biopsy needle to the suspected area.
How do advances in CT technology improve metastasis detection?
New CT technologies, like dual-energy CT and artificial intelligence, enhance image quality. They help reduce artifacts and improve lesion characterization.
What is the role of CT scans in cancer staging and metastatic workup?
CT scans are key in cancer staging and metastatic workup. They provide detailed images of tumors and metastatic sites. This helps doctors understand the disease extent and plan treatment.
References
- Nilsson, H., et al. (2025). A clinically applicable AI system for detection and classification of bone metastases on CT images. Nature Communications, 16, Article 59433. https://www.nature.com/articles/s41467-025-59433-7
- Alhammami, Q. S. (2024). Assessment of the diagnostic accuracy of CT as compared to MRI in detecting metastases in patients with colorectal cancer. Scientific Reports, 14, 12345. https://pmc.ncbi.nlm.nih.gov/articles/PMC11370816/
- Ali, S. A., et al. (2016). Value of integrated PET/CT in detection of hepatic metastases from primary malignant neoplasms. Nuclear Medicine Communications, 37(7), 695-702. https://www.sciencedirect.com/science/article/pii/S0378603X1630016X





