Explaining the procedure’s pain level and identifying the key Blood markers for hepatoblastoma (e.g., AFP). Hepatoblastoma is a rare liver cancer that mostly hits kids. Knowing about blood markers is key for catching it early and treating it well. It’s interesting that this cancer makes up only 1% of all cancers in kids. Yet, thanks to special blood tests, finding it has gotten much better.
We know how important it is to get a correct diagnosis for treating hepatoblastoma. Blood tests, like the alpha-fetoprotein test, are very important. They help find and keep track of this disease. We aim to give you a full look at these markers and why they’re so important for diagnosing hepatoblastoma.
Key Takeaways
- Understanding blood markers is key for diagnosing hepatoblastoma.
- The alpha-fetoprotein test is a major tool for diagnosis.
- Blood tests help track how the disease is doing.
- Finding it early can lead to better treatment results.
- Hepatoblastoma is a rare liver cancer mostly found in kids.
Understanding Hepatoblastoma: A Brief Overview
Hepatoblastoma is the most common liver cancer in kids, showing up early in life. It’s a rare and serious tumor in children. It’s hard to diagnose and treat because of its unique nature.
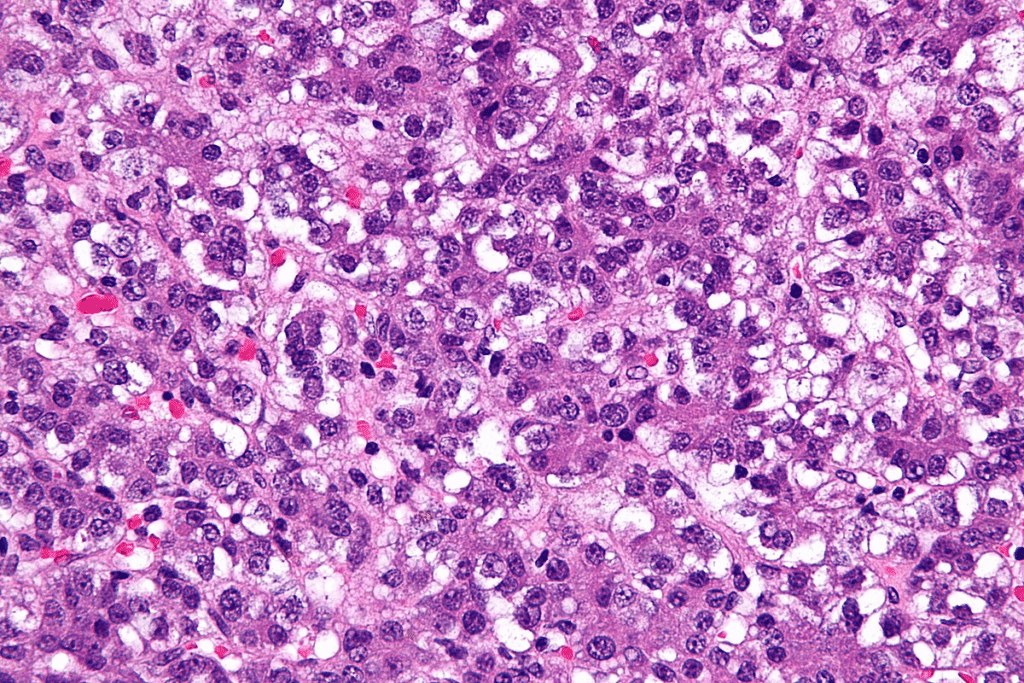
Definition and Epidemiology
Hepatoblastoma is a cancer of the liver that mostly affects kids under three. It starts from young liver cells and has different types based on how it looks under a microscope. It’s rare, happening to about 1.2 to 1.5 kids per million under 15 each year.
The most cases happen between 6 months and 3 years old. Boys are slightly more likely to get it. It often comes with genetic conditions and birth defects, showing it’s linked to both genes and the environment.
Risk Factors and Etiology
Hepatoblastoma comes from a mix of genetic and environmental factors. Some genetic syndromes increase the risk, like:
- Beckwith-Wiedemann syndrome
- Familial adenomatous polyposis (FAP)
- Low birth weight
- Premature birth
Exposure to chemicals in the womb might also play a role. But we’re not sure how these factors cause hepatoblastoma yet.
| Risk Factor | Description | Association with Hepatoblastoma |
| Beckwith-Wiedemann Syndrome | Genetic overgrowth disorder | Strongly associated |
| Familial Adenomatous Polyposis (FAP) | Genetic condition leading to colon polyps | Associated |
| Low Birth Weight | Birth weight less than 2,500 grams | Potential risk factor |
| Premature Birth | Birth before 37 weeks of gestation | Potential risk factor |
Knowing about these risk factors and how hepatoblastoma starts is key. It helps find it early and find better treatments.
The Importance of Blood Markers in Hepatoblastoma
Early detection and treatment monitoring of hepatoblastoma are greatly improved by blood markers. These markers help in diagnosing and managing the disease. They are substances in the blood that show the presence or growth of a disease.
Role in Early Detection
Early detection is key to treating hepatoblastoma successfully. Blood markers are essential in this process. They give early signs of the disease.
Alpha-fetoprotein (AFP) is a marker often used for diagnosing and monitoring hepatoblastoma. High AFP levels in the blood can mean hepatoblastoma or other conditions.
Using blood markers for early detection leads to timely treatment. This can greatly improve treatment results. Early treatment can make the disease less severe and increase survival chances.
Significance in Treatment Monitoring
Blood markers are also important for tracking treatment progress. They help doctors see how well the treatment is working. For example, a drop in AFP levels shows the treatment is effective.
- Assessing treatment efficacy: Blood markers help in evaluating how effectively the treatment is working.
- Detecting recurrence: Continuous monitoring of blood markers can help in early detection of disease recurrence.
- Guiding treatment decisions: The information obtained from blood markers can guide adjustments to treatment plans.
Understanding blood markers in hepatoblastoma shows they are more than just diagnostic tools. They are vital for ongoing patient care. By using these markers, we can offer more tailored and effective treatments.
Alpha-Fetoprotein (AFP): The Primary Blood Marker for Hepatoblastoma
Alpha-fetoprotein (AFP) plays a key role in diagnosing and tracking hepatoblastoma. It’s a protein found in high levels in patients with this cancer. This makes AFP a key marker for doctors to monitor treatment.
Normal vs. Elevated AFP Levels
Knowing the difference between normal and high AFP levels is important. AFP levels are high in fetuses but drop after birth. In adults and kids, levels should be under 10 ng/mL. But, in those with hepatoblastoma, levels can soar over 1000 ng/mL.
High AFP levels can signal hepatoblastoma, but they can also mean other things. It’s vital to look at AFP levels with other test results and symptoms.
| Condition | Typical AFP Level (ng/mL) |
| Normal | <10 |
| Hepatoblastoma | Often >1000 |
AFP as a Diagnostic Tool
AFP is a key tool for diagnosing hepatoblastoma. Doctors use it along with imaging and tissue tests to diagnose and manage the disease. High AFP levels help confirm hepatoblastoma, mainly in children.
“The measurement of AFP is a cornerstone in the diagnosis and follow-up of hepatoblastoma patients.”
Limitations of AFP Testing
Even though AFP is helpful, it has its limits. Not all hepatoblastomas show high AFP levels. Some tumors might have normal or just a bit higher levels. Also, other conditions can raise AFP levels, so results must be seen with other test findings.
We need to keep these limits in mind when using AFP. More research into other markers could help improve diagnosis.
Blood Markers for Hepatoblastoma: A Complete List
Having a complete list of blood markers is key for accurate diagnosis of hepatoblastoma. These markers help find the disease early. They also help track how well treatment is working and if the disease comes back.
Primary Markers
Primary blood markers are well-known for diagnosing and managing hepatoblastoma. The most important one is Alpha-Fetoprotein (AFP).
Alpha-Fetoprotein (AFP) is a liver and yolk sac protein in fetuses. In adults and kids, high AFP levels can mean certain cancers, like hepatoblastoma.
| Marker | Clinical Significance |
| Alpha-Fetoprotein (AFP) | Elevated levels often associated with hepatoblastoma; used for diagnosis and monitoring treatment response. |
Secondary Markers
Other blood markers can also help in diagnosing and managing hepatoblastoma.
- Beta-Human Chorionic Gonadotropin (β-hCG)
- Liver enzymes such as AST and ALT
- Bilirubin and Alkaline Phosphatase
These secondary markers give insights into the liver’s health and other possible conditions.
Beta-Human Chorionic Gonadotropin (β-hCG) is another tumor marker that can be high in some hepatoblastoma cases, mainly in certain types.
Knowing all blood markers for hepatoblastoma is vital for diagnosis and treatment planning. By using both primary and secondary markers, doctors can get a full picture of the disease.
Beta-Human Chorionic Gonadotropin (β-hCG) in Hepatoblastoma
Beta-human chorionic gonadotropin (β-hCG) is a key tumor marker in hepatoblastoma. This rare liver cancer mainly affects children. The role of β-hCG in diagnosing and managing it is becoming more important.
Clinical Significance
β-hCG’s clinical significance in hepatoblastoma is its use as a diagnostic and prognostic marker. High levels of β-hCG are seen in some subtypes of hepatoblastoma. This makes it useful for identifying certain tumor features.
While β-hCG is not the usual marker for hepatoblastoma, alpha-fetoprotein (AFP) is more common. Yet, in cases where AFP is low or more information is needed, β-hCG offers valuable insights.
Interpretation of β-hCG Levels
When looking at β-hCG levels in hepatoblastoma, many factors must be considered. These include the patient’s age, overall health, and other test results. Elevated β-hCG levels might point to a specific subtype of hepatoblastoma or a more complex tumor.
It’s important to look at β-hCG levels along with other markers and imaging. A complete diagnostic process helps ensure patients get the right diagnosis and treatment.
Liver Function Tests as Indirect Markers
Liver function tests are key in checking the liver’s health. They can hint at the presence of hepatoblastoma. These tests look at enzymes and proteins in the blood related to liver function.
When we check liver health, we look at several markers. AST (Aspartate Aminotransferase) and ALT (Alanine Aminotransferase) are mainly in the liver. High levels of these enzymes in the blood can mean liver damage or disease.
AST and ALT Levels
AST and ALT are important for diagnosing liver issues. ALT is more specific to the liver, while AST is found in other tissues too. So, a rise in ALT points more to liver damage.
In cases of hepatoblastoma, high ALT levels can show liver injury. Watching these levels helps us see how much damage the tumor has caused to the liver.
Bilirubin and Alkaline Phosphatase
Bilirubin and alkaline phosphatase are also key in liver function tests. Bilirubin is a pigment made when the liver breaks down hemoglobin. High bilirubin levels can mean liver problems or bile duct blockage, which can be linked to hepatoblastoma.
Alkaline phosphatase is in the liver and bones. While it can be high in many conditions, high levels with other liver issues might suggest hepatoblastoma.
We use these tests together to understand liver health. They’re not direct signs of hepatoblastoma but give important clues for further tests.
In summary, liver function tests are essential in diagnosing hepatoblastoma. By looking at AST, ALT, bilirubin, and alkaline phosphatase levels, doctors can check liver health and spot possible signs of hepatoblastoma.
Novel Biomarkers in Hepatoblastoma Detection
New research points to biomarkers that could change how we diagnose and watch hepatoblastoma. This rare liver cancer affects kids. Finding these biomarkers is key to better care for patients.
Emerging Research
Studies are now looking for new biomarkers to help fight hepatoblastoma. The focus is on:
- Proteomic analysis to find proteins linked to the disease
- MicroRNA profiling to spot unique patterns in cancer cells
- Genetic markers for early signs or disease growth
These new biomarkers could lead to earlier detection and better treatment tracking.
Potential Future Applications
Discovering new biomarkers for hepatoblastoma could change how doctors work. Here’s what might happen:
| Application | Description | Potential Benefit |
| Early Detection | Finding biomarkers in early stages of the disease | Higher chances of survival with early treatment |
| Personalized Medicine | Custom treatments based on biomarker profiles | More effective treatments with fewer side effects |
| Monitoring Disease Progression | Tracking changes in tumor size over time | Better ability to adjust treatment plans |
As research grows, we’ll see big changes in treating hepatoblastoma. This means better care for patients in the future.
Interpreting Blood Test Results for Hepatoblastoma
Understanding blood test results for hepatoblastoma is key. We look at markers like Alpha-Fetoprotein (AFP) and liver function tests. These tests help show if hepatoblastoma is present or growing.
Reference Ranges
Knowing the right ranges for blood markers is vital. For example, AFP levels are measured in nanograms per milliliter (ng/mL). What’s normal can differ between labs. Usually, an AFP over 1,000 ng/mL in kids might mean hepatoblastoma.
But, ranges can change with age, lab standards, and more. Infants have higher AFP levels that drop as they get older. So, we must look at the patient’s age and compare it to the right ranges.
Factors Affecting Test Results
Many things can make blood test results tricky. These include:
- Differences in how labs test and calibrate
- Things like age, gender, and health of the patient
- When the test is done, like during treatment or disease growth
- Other health issues that might change marker levels
Liver issues or inflammation can raise AFP levels temporarily. This might not always mean hepatoblastoma. So, we look at the whole clinical picture, including scans and other tests, when we read blood results.
By knowing these factors and ranges, doctors can better understand blood tests. This helps in diagnosing and treating hepatoblastoma more effectively.
Blood Markers in Monitoring Treatment Response
Monitoring how well treatment works is key in managing hepatoblastoma. Blood markers are essential for this. They help us see if the treatment is effective and if we need to change the plan.
Blood markers, like Alpha-Fetoprotein (AFP), are key in checking treatment success. AFP levels are closely watched because they show how the tumor is reacting to treatment.
Tracking AFP Decline During Treatment
One main use of AFP is to see how it goes down during treatment. When AFP levels drop, it usually means the treatment is working well. We check AFP levels often to:
- See if the current treatment is working
- Know if we need to change the treatment plan
- Guess how well the patient will do based on AFP decline
Regular monitoring helps us quickly respond to any changes in AFP levels. This ensures the treatment plan is always the best for the patient.
Markers of Disease Recurrence
Blood markers also help spot when hepatoblastoma might come back. If AFP levels start to rise or stay high, it could mean the disease is coming back. We also watch for other signs, like:
- Changes in liver function tests
- Other tumor markers going up
- Signs or symptoms that might mean the disease is coming back
Finding disease recurrence early is very important. By watching blood markers closely, we can catch problems early and adjust treatment as needed.
We keep a close eye on patients even after treatment ends. This helps us catch any signs of recurrence early. This ongoing watch is a big part of taking care of patients with hepatoblastoma.
Combining Blood Markers with Imaging Studies
Using blood markers and advanced imaging together boosts the accuracy of diagnosing hepatoblastoma. This method helps doctors plan treatments better. It combines the best of both worlds for a full picture of the disease.
Complementary Diagnostic Approaches
Blood markers, like alpha-fetoprotein (AFP), and imaging tools, such as ultrasound and CT scans, work together. Blood markers show the tumor’s chemical activity. Imaging studies reveal the tumor’s size, location, and if it has spread.
This combination helps in:
- Improving diagnosis by linking chemical markers with visual data
- Tracking how the disease changes and how well it responds to treatment
- Finding early signs of the disease coming back
Integrated Diagnostic Protocols
For managing hepatoblastoma well, using both blood markers and imaging is key. These protocols include:
- First, checking with blood markers (like AFP) and imaging (like ultrasound)
- Then, watching blood markers and doing imaging tests during treatment
- After treatment, using both to catch any disease return early
Here’s a simple example of how to use both for diagnosing hepatoblastoma:
| Diagnostic Stage | Blood Markers | Imaging Studies |
| Initial Diagnosis | AFP levels | Ultrasound, CT scan |
| During Treatment | Regular AFP monitoring | Periodic CT or MRI scans |
| Post-Treatment Surveillance | AFP levels every 3 months | Imaging studies (CT/MRI) every 6 months |
By mixing blood markers with imaging, doctors get a clearer view of hepatoblastoma. This leads to better care for patients.
AFP-Negative Hepatoblastoma: Diagnostic Challenges
Diagnosing AFP-negative hepatoblastoma is tough. It’s a rare liver cancer in kids, and alpha-fetoprotein (AFP) is key for diagnosis. But, sometimes AFP levels are normal, making it hard to diagnose.
Alternative Diagnostic Approaches
When AFP is not high, doctors use other methods. They use ultrasound, CT scans, and MRI to see the tumor. They also look at biopsy samples to confirm the diagnosis.
Researchers are looking for new markers and tools. This includes:
- Beta-human chorionic gonadotropin (β-hCG)
- Liver function tests
- Novel biomarkers identified through research
Using these methods together can make diagnosis more accurate, even when AFP is not high.
| Diagnostic Approach | Description | Utility in AFP-Negative Hepatoblastoma |
| Imaging Studies | Ultrasound, CT, MRI | High |
| Histopathology | Biopsy examination | Critical for confirmation |
| β-hCG Levels | Measurement of beta-human chorionic gonadotropin | Potential supplementary marker |
Case Studies and Findings
Many case studies show the challenges and successes in diagnosing AFP-negative hepatoblastoma. For example, a study in the Journal of Pediatric Hematology/Oncology talked about a 2-year-old with a liver mass and normal AFP. The diagnosis was made with imaging and biopsy.
These cases show the need for a detailed diagnostic approach. They also highlight the importance of ongoing research for new biomarkers and techniques.
Blood Marker Screening in High-Risk Populations
Screening high-risk groups for hepatoblastoma with blood markers is key to early detection. It helps improve patient outcomes. We focus on finding those at risk and setting up good screening plans.
Screening Protocols
Good screening for hepatoblastoma means watching blood markers like alpha-fetoprotein (AFP) in high-risk people. High-risk groups include kids with certain genetic syndromes and those with a family history of the disease.
We suggest regular screening for high-risk individuals from birth or when risk is identified. How often to screen depends on the individual’s risk factors. A healthcare provider should decide.
Cost-Effectiveness and Outcomes
Screening for hepatoblastoma in high-risk groups is cost-effective. Research shows early detection leads to better results and lower costs over time.
Early detection can mean less intense and expensive treatments. This improves patients’ lives and cuts healthcare costs.
Early detection is key to successful treatment. We think setting up detailed screening plans for high-risk groups is vital for better hepatoblastoma outcomes.
Future Directions in Hepatoblastoma Blood Marker Research
New technologies are changing how we study blood markers for hepatoblastoma. We’re learning more about this disease and finding better ways to diagnose and treat it.
Proteomics and Metabolomics
Proteomics and metabolomics are leading the way in hepatoblastoma research. They help find new biomarkers for early detection and tracking of the disease.
Proteomic analysis looks at all proteins in an organism. It helps us understand what’s happening in hepatoblastoma. Metabolomics studies small molecules in cells and tissues. It shows us the health or disease state of a cell or tissue.
| Technology | Application in Hepatoblastoma | Potential Benefits |
| Proteomics | Identification of novel protein biomarkers | Early detection, personalized treatment |
| Metabolomics | Analysis of metabolic profiles | Understanding disease mechanisms, monitoring treatment response |
Liquid Biopsy Approaches
Liquid biopsy is becoming more important in studying hepatoblastoma. It looks at DNA or biomarkers in blood or fluids. This is a less invasive way than traditional biopsies.
Liquid biopsy is great because it’s easy to do again and again. It can also find disease early or when it comes back.
Genetic Markers in Blood
Studying genetic markers in blood is also promising. It helps find specific genetic changes linked to the disease. This leads to blood tests for diagnosis and tracking.
These genetic markers tell us a lot about the tumor. They help doctors decide on treatment and watch for disease return.
As research grows, using these new technologies will change how we manage hepatoblastoma. It brings hope for better care and outcomes for patients.
Conclusion
We’ve looked into how blood markers help diagnose and manage hepatoblastoma. Alpha-fetoprotein (AFP) is key in spotting and tracking this disease. These markers give us important clues about how the disease is doing and how well treatments are working.
Using blood markers with imaging tests makes diagnosing better and helps decide on treatments. New research might bring even better ways to find and treat hepatoblastoma. This could include new biomarkers found through studying proteins and metabolism.
Knowing the value of blood markers helps us give better care to patients. As we keep looking for new ways to diagnose and treat, we can improve how we handle this complex disease.
FAQ
What are the primary blood markers used for diagnosing hepatoblastoma?
The main blood marker for diagnosing hepatoblastoma is alpha-fetoprotein (AFP). High levels of AFP often point to this condition.
How is alpha-fetoprotein (AFP) used in the diagnosis of hepatoblastoma?
AFP helps identify possible cases of hepatoblastoma, mainly in kids. High AFP levels suggest this tumor might be present.
Are there other blood markers associated with hepatoblastoma beside AFP?
Yes, markers like beta-human chorionic gonadotropin (β-hCG) and liver function tests also help diagnose hepatoblastoma. They offer more information for diagnosis.
What is the role of liver function tests in diagnosing hepatoblastoma?
Liver function tests, such as AST and ALT, can hint at hepatoblastoma. They show if the liver is not working right.
How are blood markers used in monitoring treatment response for hepatoblastoma?
Blood markers, like AFP, track how well treatment is working. They show if AFP levels are going down and if the tumor might come back.
What are the challenges in diagnosing AFP-negative hepatoblastoma?
Diagnosing AFP-negative hepatoblastoma is tough. It needs other tests, like imaging and blood markers, to confirm the tumor’s presence.
How can combining blood markers with imaging studies improve hepatoblastoma diagnosis?
Using blood markers with imaging studies makes diagnosis better. It helps find and track hepatoblastoma more accurately.
What are the future directions in hepatoblastoma blood marker research?
Research is looking into new ways like proteomics and genetic markers in blood. These could lead to better diagnosis and monitoring of hepatoblastoma.
Are there specific screening protocols for high-risk populations regarding hepatoblastoma?
Yes, there are special screening plans for those at high risk. This includes kids with certain genetic conditions or a family history of hepatoblastoma.
How do blood markers contribute to the overall management of hepatoblastoma?
Blood markers are key in finding, diagnosing, and tracking hepatoblastoma. They help manage the disease and improve patient care.
What is the significance of interpreting blood test results for hepatoblastoma correctly?
It’s vital to understand blood test results for hepatoblastoma. Knowing what the results mean helps in accurate diagnosis and treatment.
References
National Center for Biotechnology Information. Hepatoblastoma blood markers for early detection in children. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4728840/
National Center for Biotechnology Information. Hepatoblastoma Blood Markers for Early Detection and Diagnosis. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4728840/
National Center for Biotechnology Information. Hepatoblastoma Blood Markers Diagnosis Implications. Retrieved from https://pubmed.ncbi.nlm.nih.gov/22180200/



































