Hepatoblastoma is a rare liver cancer that mainly hits young kids. Most cases are found in the first 18 months of life. This makes it a big worry for kids’ health.
Studies show that catching it early is key for better treatment and results in kids with hepatoblastoma. Knowing when it usually shows up helps parents and doctors spot signs early.
Key Takeaways
- Hepatoblastoma is mainly found in kids under 3.
- Spotting it early greatly boosts treatment success.
- Knowing when it usually shows up is vital for parents and doctors.
- Pediatric liver tumors like hepatoblastoma need special care.
- The usual age range for finding hepatoblastoma is the first 18 months of life.
Understanding Hepatoblastoma: A Rare Pediatric Liver Cancer
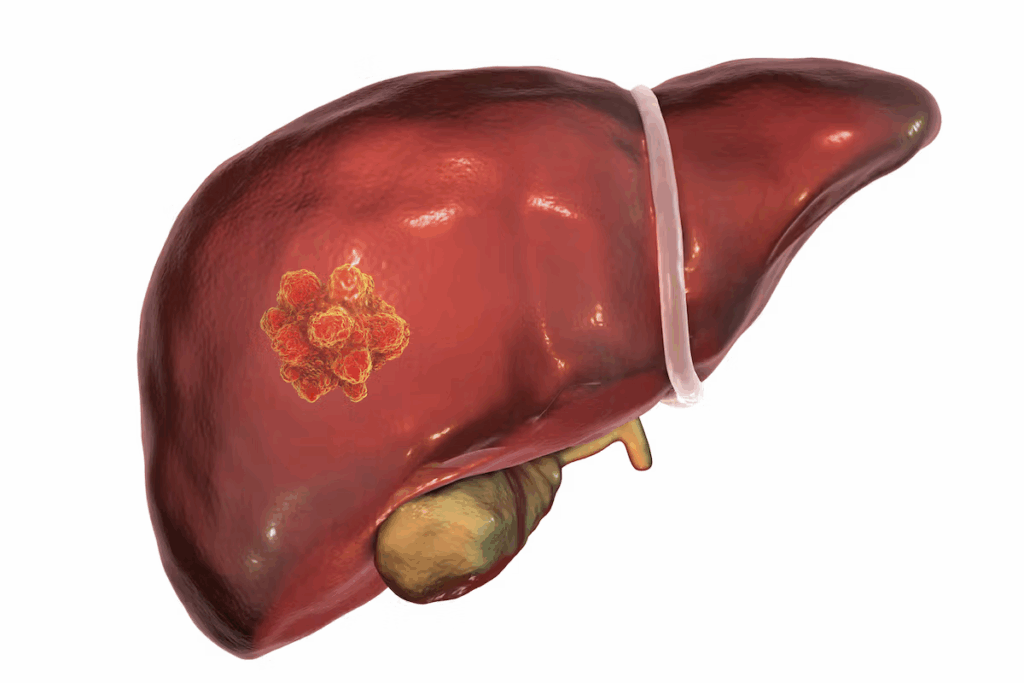
Hepatoblastoma is a rare liver cancer that mainly affects children. It’s the most common liver cancer in kids. This cancer is special because of its unique challenges in diagnosis and treatment.
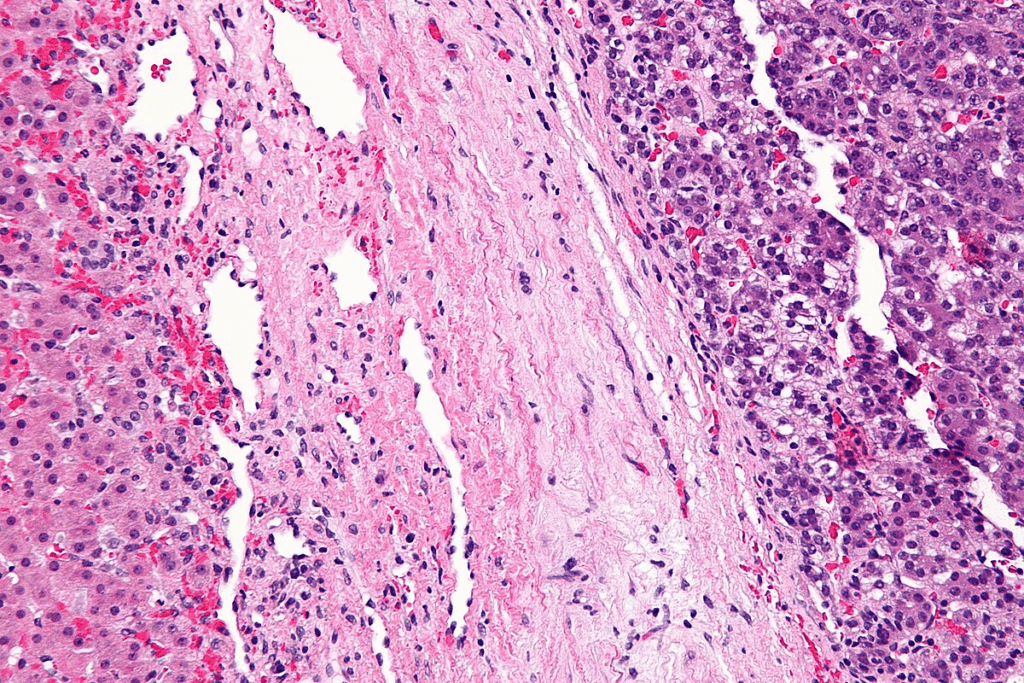
Definition and Classification of Hepatoblastoma
Hepatoblastoma is a cancer of the liver that mostly happens in kids under 3. It starts from immature liver cells. There are different types of hepatoblastoma, each with its own characteristics.
These types include fetal, embryonal, macrotrabecular, and small cell undifferentiated. Knowing the type helps doctors predict how well a child will do and plan treatment.
Incidence Rates in the United States
Hepatoblastoma is rare, making up about 1% of all cancers in kids. In the U.S., it affects about 1.5 kids per million under 15 each year. The number of cases hasn’t changed much, but some studies show a slight rise.
Because it’s so rare, studying it is hard. This highlights the importance of working together on research.
Age of Hepatoblastoma Diagnosis: Typical Presentation Window

Hepatoblastoma is a rare liver cancer mostly found in young children. We’ll look at when it’s usually diagnosed and how it’s spread out by age. This helps us understand this rare cancer better.
Primary Age Range for Diagnosis
Most cases of hepatoblastoma happen in kids under 3. This age is key because it’s when cancer is most common. Studies say the average age of diagnosis is about 18 months. This shows why it’s important to screen for it early in childhood.
Statistical Distribution Across Age Groups
About 90% of hepatoblastoma cases are in kids under 5. The number of cases drops as kids get older. This makes it mostly a disease of young children. Research also shows boys are slightly more likely to get it, and it’s more common in kids with certain genetic conditions.
Let’s break down the numbers further:
- Infants (0-12 months): A lot of cases are found in the first year.
- Toddlers (1-3 years): This is when most cases are diagnosed, usually between 1-2 years.
- Preschool age (4-5 years): The number of cases starts to go down but stays high.
- School age and beyond (6 years and older): Cases are rare but can happen, so we must stay alert.
Knowing when and how often hepatoblastoma is diagnosed helps us make better screening plans. This can lead to catching it earlier and improving treatment chances.
Prenatal and Neonatal Hepatoblastoma Detection
The prenatal and neonatal periods are key for spotting hepatoblastoma, a rare liver cancer in kids. New ultrasound tech has made finding congenital tumors like hepatoblastoma better.
Congenital Hepatoblastoma Cases
Congenital hepatoblastoma means the cancer is there at birth. These cases are very rare and often linked to genetic syndromes. Finding congenital hepatoblastoma early is key for treatment.
Research shows congenital hepatoblastoma can be seen as early as 24-28 weeks in the womb. It’s usually found by chance during routine scans. This shows how important regular prenatal care is.
Screening During Pregnancy and After Birth
Routine prenatal ultrasound isn’t made to find hepatoblastoma. But, it can spot liver issues. After birth, doctors use exams and scans to diagnose hepatoblastoma in newborns. Programs for screening and follow-up care are vital for early detection.
Guidelines for screening high-risk groups, like those with certain genetic syndromes, are changing. Early detection through prenatal ultrasound and postnatal screening can greatly improve treatment results.
We suggest that pregnant women with a family history of genetic syndromes talk to their doctor. Discussing risk and screening options can lead to early detection and management of congenital hepatoblastoma.
Infant Hepatoblastoma (Ages 0-12 Months)
Hepatoblastoma in infants is different from in older kids. It’s vital to catch it early. Infants often show signs like a big belly or vague symptoms, making it hard to diagnose.
Presentation Characteristics in Infants
Infant hepatoblastoma shows signs that don’t point directly to liver cancer. Common signs include:
- Abdominal enlargement or distension
- Failure to thrive or loss of appetite
- Jaundice or yellowing of the skin and eyes
- Abdominal pain or discomfort
These symptoms can mean many things, not just liver cancer. Doctors must be very careful when they see these signs in babies.
Diagnostic Challenges in This Age Group
Diagnosing hepatoblastoma in babies is tough. The symptoms are not clear, so doctors might not think of liver cancer first. Babies can’t tell us how they feel, so doctors have to rely on what they see and tests.
Diagnostic Approaches: Doctors use many tests like ultrasound and CT scans. They also check blood for alpha-fetoprotein (AFP) levels. Sometimes, they might take a biopsy, but it’s risky for young babies.
It’s very important to find and treat infant hepatoblastoma early. We stress the need for doctors to be very careful and use the latest tests to help these young patients.
Toddler and Preschool Age Diagnosis (Ages 1-5 Years)
It’s important to know about hepatoblastoma in young kids. This rare liver cancer mainly hits children. Finding it early in toddlers and preschoolers is key.
Peak Incidence Period
Hepatoblastoma hits hardest in kids aged 1 to 3. This age group sees the most cases. Early detection is vital for better treatment results.
Research shows the highest rate of hepatoblastoma is in the first three years. This highlights the need for close monitoring during this time.
Common Presenting Symptoms
The symptoms of hepatoblastoma in young kids vary. Yet, there are common signs to watch for. These include:
- Abdominal distension or swelling
- Pain or discomfort in the abdominal area
- Loss of appetite or weight loss
- Fatigue or lethargy
Spotting these symptoms early can lead to quick diagnosis and treatment. Parents and caregivers should seek medical help if they notice anything odd.
Even though hepatoblastoma is rare, knowing its symptoms and when it usually appears can help. This knowledge is critical for young children’s health.
School-Age and Adolescent Cases (Ages 6-18 Years)
Hepatoblastoma is rare in kids aged 6 to 18. It’s mostly seen in young children. But, it can also happen in older kids and teens. This makes it important to know how to diagnose it in these age groups.
Rarity and Distinctive Features
Hepatoblastoma is rarely found in kids over 5. When it does occur in older kids, it has unique signs. These signs can include a big belly, pain, or early puberty symptoms.
Because it’s so rare, finding it early can be hard. Doctors need to be very careful to catch it on time.
Differential Diagnosis Considerations
Figuring out if a child has hepatoblastoma involves a few steps. Doctors use imaging, lab tests, and looking at tumor tissue. This helps tell it apart from other liver issues or diseases.
It’s key to know the special traits of hepatoblastoma in older kids. Some types might be more common in this age group. This can change how doctors treat it and what the future might hold.
In short, while rare, knowing about hepatoblastoma in older kids is vital. It helps doctors make the right diagnosis and start treatment quickly.
Risk Factors Influencing Age of Onset
Knowing what increases the chance of getting hepatoblastoma early is key. This rare liver cancer has several risk factors. Knowing them helps in managing the disease better.
Genetic Predisposition Syndromes
Some genetic syndromes raise the risk of hepatoblastoma. Beckwith-Wiedemann syndrome is one, causing overgrowth and a higher chance of tumors. Other conditions like Familial Adenomatous Polyposis (FAP) and Li-Fraumeni syndrome also increase the risk.
Children with these syndromes need to be watched closely from a young age. These conditions can lead to hepatoblastoma early, often in the first year of life.
| Genetic Syndrome | Characteristics | Risk Level |
| Beckwith-Wiedemann Syndrome | Overgrowth, macroglossia, omphalocele | High |
| Familial Adenomatous Polyposis (FAP) | Multiple colon polyps, increased risk of colorectal cancer | Moderate to High |
| Li-Fraumeni Syndrome | Increased risk of various cancers, including sarcomas and breast cancer | High |
Environmental and Maternal Factors
Genetic factors aren’t the only ones to consider. Environmental and maternal factors also play a part. For example, chemicals and infections during pregnancy can increase risk. Maternal smoking and certain jobs are also linked to higher risk.
Low birth weight and being born too early also raise the risk. Knowing these factors helps find children who need early checks.
Healthcare providers can then offer better care by knowing these risks. This can lead to better outcomes for children at risk of hepatoblastoma.
Diagnostic Methods Across Different Age Groups
Diagnosing hepatoblastoma needs a detailed plan that changes with age. It uses imaging, lab tests, and biopsies, all tailored for the patient’s age.
Imaging Techniques by Age
Imaging is key in finding hepatoblastoma. The right imaging tool depends on the patient’s age and symptoms.
- Infants (0-12 months): Ultrasound is first because it’s safe and doesn’t use radiation.
- Toddlers and Preschoolers (1-5 years): MRI is added to ultrasound for clearer tumor images.
- School-age children and Adolescents (6-18 years): MRI is preferred over CT scans for its detailed images and safety.
Laboratory Markers and Biopsy Considerations
Laboratory tests and biopsies are vital for diagnosis.
Laboratory Markers: Alpha-fetoprotein (AFP) is a key marker for hepatoblastoma. High AFP levels often point to this cancer, but levels can vary.
| Age Group | Typical AFP Levels | Diagnostic Consideration |
| Infants (0-12 months) | Normally elevated, can be >1000 ng/mL | Compare to age-adjusted norms |
| Toddlers and Preschoolers (1-5 years) | Usually | Significant elevation suggests hepatoblastoma |
| School-age children and Adolescents (6-18 years) | Normally | Any elevation is considered abnormal |
Biopsy Considerations: A biopsy is often needed to confirm the diagnosis. The type of biopsy depends on the tumor’s size and location.
We stress the need for a thorough diagnostic plan. It should include imaging, lab tests, and biopsies to accurately diagnose hepatoblastoma in all age groups.
Staging and Classification Based on Age at Diagnosis
Understanding how to stage and classify hepatoblastoma is key for doctors. The age when a child is diagnosed affects how serious the disease is. This information helps doctors decide the best treatment.
PRETEXT and Other Staging Systems
The PRETEXT system is a common way to check how big a tumor is in a child’s liver. It looks at how many parts of the liver the tumor has reached. Other systems might also be used to get a clearer picture of the disease.
Age-Specific Risk Stratification
It’s important to group children with hepatoblastoma by age. This helps doctors plan treatments that fit each child’s needs. This way, treatments can be more effective.
For example, babies with this disease might need special care that older kids don’t. The PRETEXT system helps doctors figure out the best treatment plan for each child.
By understanding the age at diagnosis, doctors can predict how well a child might do. They can then tailor treatments to improve care and outcomes.
Treatment Approaches Based on Age of Diagnosis
Age is key in picking the best treatment for hepatoblastoma. This rare liver cancer in kids is treated with surgery and chemotherapy. The treatment plan is made just for the child, based on their age when they were diagnosed.
Surgical Considerations for Different Age Groups
Surgery is a big part of treating hepatoblastoma, no matter the age. But, the surgery can change based on the child’s age and the tumor’s type. For babies, the surgery needs to fit their small body. Older kids aim to remove the tumor while keeping the liver working well.
Young kids, like those under 12 months, face special challenges. Their small liver and possible birth defects make surgery harder. Older kids might have bigger tumors, needing more complex surgeries.
| Age Group | Surgical Considerations | Chemotherapy Protocols |
| Infants (0-12 months) | Adapted surgical techniques for smaller anatomy | Reduced dose intensity to minimize toxicity |
| Toddlers and Preschoolers (1-5 years) | Standard surgical resection with focus on liver preservation | Standard chemotherapy protocols with monitoring for toxicity |
| School-age and Adolescents (6-18 years) | Complex resections for larger tumors | Intensified chemotherapy protocols with careful management of side effects |
Chemotherapy Protocols and Age-Related Toxicity
Chemotherapy is a key part of treating hepatoblastoma. It’s used before surgery to shrink tumors and after to kill any left-over cancer cells. The type and amount of chemotherapy depends a lot on the child’s age.
Young kids, like babies, get lower doses of chemotherapy to avoid harm. As kids get older, the chemotherapy can be stronger. But, it’s important to watch for side effects closely.
Finding the right balance between making chemotherapy work and avoiding harm is key. By adjusting treatments for each child’s age and health, we can help them get better while avoiding long-term problems.
Prognosis and Survival Rates by Age at Diagnosis
Knowing how age affects hepatoblastoma treatment is key. The outlook for this liver cancer changes with age. Younger kids usually have a better chance of recovery.
The Role of Age in Prognosis
Age plays a big role in how well a child with hepatoblastoma will do. Kids who get diagnosed early tend to do better. This is because their tumors are often easier to treat and they are healthier overall.
Age-related factors also include how well the tumor responds to treatment. Young kids are more likely to have tumors that can be removed. This leads to higher survival rates.
Long-term Outcomes and Survival Statistics
Thanks to better treatments, more kids with hepatoblastoma are living longer. Today, over 80% of kids survive for five years after diagnosis.
| Age Group | 5-Year Survival Rate |
| 0-12 months | 85% |
| 1-5 years | 82% |
| 6-18 years | 75% |
The table shows survival rates for different age groups. Younger kids have better chances, showing the importance of early treatment.
The link between age and hepatoblastoma prognosis is clear. Understanding these factors helps doctors create better treatment plans. This improves the chances of recovery for kids with this rare cancer.
Screening Recommendations for High-Risk Children
Children with certain genetic syndromes face a higher risk of hepatoblastoma. This makes it critical for pediatricians and caregivers to know which conditions increase this risk. They should be vigilant in screening these children.
Guidelines for Children with Predisposing Conditions
Children with Beckwith-Wiedemann syndrome, familial adenomatous polyposis (FAP), and trisomy 18 are at higher risk. Regular screening is key for early detection in these groups. We advise regular abdominal ultrasounds and alpha-fetoprotein (AFP) level checks for them.
The American Academy of Pediatrics suggests regular ultrasounds for children with Beckwith-Wiedemann syndrome. They should have ultrasounds every 3 months until they are 4, then every 6 months until they are 7. Early detection is vital for better treatment outcomes, making these guidelines essential.
Surveillance Protocols by Age Group
Screening for hepatoblastoma changes with age and risk. For high-risk infants and toddlers, screening starts soon after birth. AFP levels need to be watched closely as they can signal hepatoblastoma.
Children aged 1 to 3 should have ultrasounds every 3 to 6 months. As they get older, screenings might be less frequent. But they should be based on the child’s specific risk factors and medical history.
By sticking to these screening recommendations, we can catch hepatoblastoma early in high-risk children. It’s vital for healthcare providers to work with families. This ensures they follow the recommended surveillance protocols.
Conclusion: The Importance of Early Detection Across All Age Groups
Early detection and diagnosis are key to better health for kids with hepatoblastoma. This rare liver cancer can strike at any age, from before birth to the teenage years.
Getting a diagnosis early makes a big difference. It helps doctors treat the cancer more effectively and increases chances of survival. Knowing when and why hepatoblastoma happens helps doctors catch it sooner.
It’s vital to spread the word about hepatoblastoma. Parents, caregivers, and doctors need to know the signs. This knowledge helps catch the disease early.
By raising awareness, we help kids get the care they need fast. This leads to better health and a better life for them.
FAQ
What is the typical age range for hepatoblastoma diagnosis?
Hepatoblastoma is usually found in kids under 3. Most cases happen in the first 18 months.
Can hepatoblastoma be detected prenatally?
Yes, sometimes it can be found before birth through ultrasound. This shows how important prenatal checks are.
What are the common presenting symptoms of hepatoblastoma in toddlers and preschool-age children?
Symptoms include a big tummy, not wanting to eat, losing weight, and feeling tired. Finding it early is key.
How is hepatoblastoma diagnosed across different age groups?
Doctors use ultrasound, CT, and MRI scans. They also check alpha-fetoprotein (AFP) levels. Sometimes, a biopsy is needed to confirm it.
What are the risk factors that influence the age of onset of hepatoblastoma?
Certain genetic syndromes and environmental factors can raise the risk. These include Beckwith-Wiedemann syndrome and FAP.
How is hepatoblastoma staged and classified based on age at diagnosis?
The PRETEXT system is used for staging. The child’s age also plays a role in planning treatment.
What are the treatment approaches for hepatoblastoma based on age of diagnosis?
Treatments include surgery, chemotherapy, and sometimes liver transplant. The plan is made based on the child’s age, tumor, and health.
What is the prognosis for children with hepatoblastoma based on age at diagnosis?
Younger kids usually have a better chance of survival. Thanks to better treatments, more kids are living longer.
Are there screening recommendations for high-risk children?
Yes, kids with certain conditions should get regular checks. This includes imaging and AFP level tests to catch it early.
What is the importance of early detection across all age groups?
Finding it early helps kids get better treatments and live longer. Knowing the signs and symptoms is key to early detection.
National Center for Biotechnology Information. Hepatoblastoma age of diagnosis in pediatric patients. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9658228/
National Center for Biotechnology Information. Hepatoblastoma age of diagnosis in pediatric patients. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9658228/
References
Benoist, M. (2002). The natural history of lumbar degenerative spinal stenosis: A comprehensive review. Joint Bone Spine, 69(5), 450-457. https://www.sciencedirect.com/science/article/abs/pii/S1297319X02004293


































