
Blood transfusions save lives for kids with many health issues. But, nearly 1 in 5 children might face side effects, from mild to serious. These can be life-threatening. A detailed look at the short and long-term immunological and fluid management risks of blood transfusions in children, often related to size (like a Bmi calculator).
Doctors must balance the good and bad of blood transfusions. They are vital for treating severe anemia and blood loss from surgery. But, knowing the risks is just as important. These include infections, allergic reactions, and changes to the immune system.
To keep kids safe, we must understand and reduce these risks. This way, blood transfusions can be given safely in pediatric care.
Key Takeaways
- Blood transfusions can have adverse effects in nearly 1 in 5 children.
- Understanding the risks is key for safe use.
- Pediatric care must weigh the benefits and risks of transfusions.
- Steps can be taken to lower the risk of complications.
- Knowing the risks is essential for good pediatric care.
Understanding Blood Transfusions in Pediatric Care
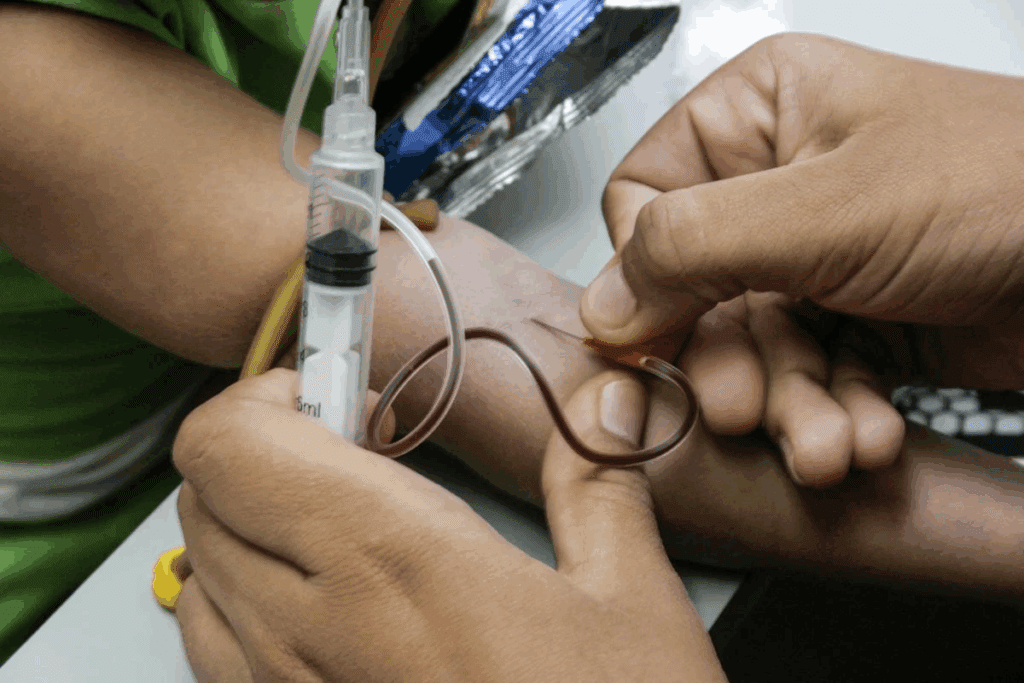
In pediatric care, blood transfusions are key for managing health issues in kids. They help with anemia and during complex surgeries. These transfusions add blood or blood parts to a patient’s blood, helping treat many conditions.
Definition of Blood Transfusions
A blood transfusion is when blood or blood products are given to a child. Blood products include red blood cells, plasma, platelets, or cryoprecipitate. Each has its own use in patient care.
For example, red blood cells help with anemia or blood loss. Plasma is used for clotting issues. We use blood transfusions in pediatric care for recovery, managing chronic conditions, or treating acute illnesses. The decision to give a blood transfusion is made with care, weighing the benefits and risks for the child.
Reasons for Blood Transfusions in Children
Children may need blood transfusions for several reasons, including:
- Anemia: A condition with low red blood cells or hemoglobin, often treated with red blood cell transfusions.
- Bleeding Disorders: Conditions like hemophilia that affect clotting, requiring clotting factor transfusions.
- Cancer: Some cancer treatments can lower bone marrow, leading to blood transfusions to increase blood cell counts.
- Surgical Procedures: Surgeries can cause a lot of blood loss, needing transfusions to keep blood volume up and ensure tissue oxygenation.
A study in the International Journal of Life Sciences, Biotechnology and Pharma Research found postoperative infections are a big risk. This shows the need for careful management and monitoring before, during, and after surgery.
Potential Risks Associated with Blood Transfusions
Pediatric blood transfusions are vital in some medical cases. Yet, they come with risks and complications. It’s our duty as healthcare providers to know these risks. This ensures blood transfusions are safe for children.
Allergic Reactions
Allergic reactions are a common issue with blood transfusions. These can be mild or severe. Symptoms include hives, itching, and trouble breathing.
In severe cases, allergic reactions can cause anaphylaxis. This is a life-threatening condition that needs quick medical help.
To handle allergic reactions, we give antihistamines or corticosteroids before or during the transfusion. If a patient has had severe allergic reactions before, we take extra steps. This might include using washed red blood cells or irradiating the blood product.
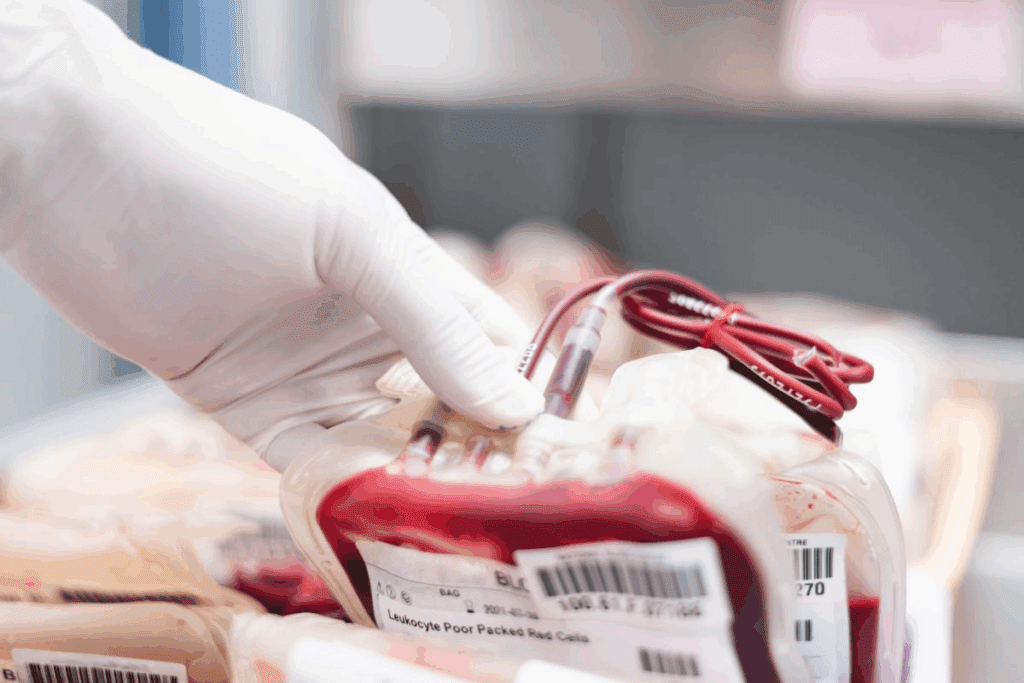
Infections
There’s a risk of infectious diseases from blood transfusions, despite strict screening. These can include viruses like hepatitis B and C, HIV, and bacterial contamination.
A study on hepatitis B virus transmission through blood transfusions shows the need for strict screening. We test donated blood for infectious agents. We also use nucleic acid testing (NAT) to find viral genetic material.
| Infectious Agent | Screening Method | Risk Reduction |
| Hepatitis B Virus (HBV) | Nucleic Acid Testing (NAT), Serological Tests | Significantly reduces transmission risk |
| HIV | NAT, Serological Tests | Highly effective in detecting infected donations |
| Bacterial Contamination | Culture-based methods, Rapid Testing | Reduces risk of septic transfusion reactions |
Transfusion-Related Acute Lung Injury (TRALI)
TRALI is a serious issue that causes non-cardiogenic pulmonary edema. It’s linked to plasma-containing blood products. Symptoms include respiratory distress, hypoxemia, and bilateral infiltrates on chest radiography.
To lower TRALI risk, we limit fresh frozen plasma use. We also use male donor plasma. TRALI is more common in multiparous female donors.
Iron Overload
Repeated blood transfusions can cause iron overload. This is when too much iron builds up in the body. It can harm organs like the heart, liver, and endocrine organs.
To manage iron overload, we watch patients’ iron levels closely. We might give iron-chelating therapy to reduce iron burden. This is key for children needing chronic transfusions.
Short-Term Effects of Blood Transfusions
The short-term effects of blood transfusions in children are important for doctors. When a child gets a blood transfusion, their body might react in different ways. It’s key to understand these reactions to give the best care.
Fever and Chills PageSpeed
Fever and chills are common after blood transfusions. These symptoms happen because the body’s immune system reacts to the blood. Sometimes, they can mean an allergic reaction or infection. Doctors watch children’s temperature and health closely during and after the transfusion.
Nausea and Vomiting
Nausea and vomiting can happen after blood transfusions. These symptoms can make children feel uncomfortable and might lead to dehydration. Doctors help keep children hydrated and watch their condition to lessen these effects. Sometimes, they give medicine to help with nausea.
Changes in PageSpeedBlood Pressure
Changes in blood pressure can happen during or after a transfusion. It’s important to watch blood pressure closely, as big changes can mean a bad reaction. Doctors work to keep blood pressure stable and ensure the child’s safety during the transfusion.
| Short-Term Effect | Sympt SRComs | |
| Fever and Chills | Elevated body temperature, shaking | Monitoring temperature, medication for fever reduction |
| Nausea and Vomiting | Feeling queasy, vomiting | Keeping the child hydrated, administering anti-nausea medication |
| ChangesBlood Pressure | Fl uctuations in blood pressure | Close monitoring, managing blood pressure through appropriate medical interventions |
Long-Term Risks of Blood Transfusions
Blood transfusions in children can have long-term risks. They are often needed to save lives but can affect a child’s health later on.
Development of Antibodies
One major risk is the development of antibodies against the blood components. This can make future transfusions more complicated. We must watch children closely who have had blood transfusions.
These antibodies can also harm the child’s health. They might cause hemolytic disease of the newborn in future pregnancies. It’s key to manage this risk for the child’s long-term health.
Risk of Chronic Diseases
Some studies link blood transfusions to chronic diseases. For example, iron overload can damage organs over time if not managed. We must know these risks and find ways to reduce them.
There’s also evidence that blood transfusions might be connected to other chronic conditions. More research is needed. As healthcare providers, we must keep up with the latest research to care for our patients the best way.
Effects on Immune Function
Blood transfusions can affect a child’s immune system. Some studies show they might change how the immune system works. This area needs more study to understand the effects and how to prevent harm.
Children’s immune systems are developing, and blood transfusions can impact this. By studying these effects, we can help children who have had transfusions.
The Importance of Proper Blood Matching
To avoid risks, it’s key to match blood accurately for transfusions. Matching blood properly is vital for the safety and success of blood transfusions in kids. We’ll talk about why ABO and Rh compatibility matter and how we screen for diseases in blood donations.
ABO and Rh Compatibility
Matching ABO and Rh types is essential to avoid harmful reactions. ABO blood group system checks if the donor and recipient’s red blood cells match.
Rh type is also important because Rh incompatibility can cause serious issues, mainly in future transfusions.
- ABO Compatibility: Makes sure the donor’s red blood cells won’t be attacked by the recipient’s immune system.
- Rh Compatibility: Prevents the formation of antibodies against Rh-positive blood in Rh-negative recipients.
Screening for Infectious Diseases
Testing donated blood for diseases is a key step to keep transfusions safe. We use strict tests to find viruses and bacteria.
- Hepatitis B and C: We test for these viruses to stop them from being passed through blood transfusions.
- HIV: Screening for HIV is important to keep the blood supply safe.
- Syphilis and Other Infections: We also test for other diseases to lower risks even more.
By matching blood correctly and testing for diseases, we greatly reduce risks in blood transfusions for kids. This careful method ensures blood transfusions are safe and effective.
Evaluating the Need for a Blood Transfusion
To decide if a child needs a blood transfusion, we must understand their health fully. We look at many factors to see if a transfusion is needed and how to do it safely.
Clinical Criteria for Transfusion
Deciding to give blood is based on certain criteria. We check the child’s hemoglobin levels and if they show symptoms like tiredness or trouble breathing. For example, kids with severe anemia from esophagitis or laceration might need a transfusion to help their bodies get enough oxygen.
We also look at how severe the child’s condition is and the risks of not giving a transfusion. We check lab results and the child’s overall health. Sometimes, a transfusion is needed to prevent serious problems or to help during surgery.
Alternatives to Blood Transfusions
In some cases, we might not need to give blood. For kids with mild anemia or minor surgeries, other treatments could work. For instance, iron supplements can treat iron deficiency anemia and might avoid the need for a transfusion.
For kids with conditions like encopresis that don’t directly need a transfusion, we manage that condition separately. We also think about using erythropoiesis-stimulating agents in some cases to reduce the need for transfusions.
“The decision to transfuse should be based on a careful assessment of the patient’s clinical status, taking into account the risks and benefits of transfusion.”
— Source: Clinical Guidelines for Blood Transfusion
By carefully checking if a blood transfusion is needed and looking at other options, we make sure kids get the best care. This way, we reduce risks and improve their chances of a good outcome.
Parental Concerns and Education
The idea of a blood transfusion can worry families a lot. They need clear info and reassurance. Healthcare providers are key in helping parents through this.
Supporting Families Through the Process
When a child needs a blood transfusion, parents have lots of questions. We know emotional support is as vital as medical care. Our team aims to guide and reassure families.
Key aspects of support include:
- Clear communication about the transfusion process
- Addressing concerns and questions in a timely manner
- Providing emotional support during and after the procedure
Informational Resources for Parents
Education is key in care. We offer informational resources to help parents understand the blood transfusion process. These include:
- Detailed explanations of the transfusion procedure
- Information on possible risks and benefits
- Guidance on what to expect during recovery
For families with children in the NICU or those with conditions like hydrops fetalis, we provide special support. We tailor our resources to their unique needs.
| Resource | Description | Benefit |
| Transfusion Process Guide | A detailed explanation of what happens during a blood transfusion | Reduces anxiety by providing clear expectations |
| Risk and Benefit Information | Comprehensive overview of possible risks and benefits of blood transfusions | Empowers parents to make informed decisions |
| Post-Transfusion Care Instructions | Guidance on caring for a child after a blood transfusion | Ensures a smooth recovery process |
Regulatory Oversight and Safety Measures
The safety of blood transfusions is a big concern. It involves strict rules and careful safety steps. Agencies like the FDA are key in keeping the blood supply safe. We’ll look at how they protect kids getting blood transfusions.
The Role of the FDA in Blood Safety
The FDA watches over the blood supply in the U.S. They make and enforce rules for blood donation and transfusion. This helps keep blood safe from infections and other dangers.
We count on the FDA to check blood tests and make sure blood places follow the rules. Their work helps us trust the blood system.
Blood Bank Protocols
Blood banks have strict rules to keep blood safe and good. They check donors, test blood for diseases, and store it right. We’ll see what these steps do to keep transfusions safe.
| Protocol | Description | Importance |
| Donor Screening | Checking donor health and history to stop disease spread. | High |
| Blood Testing | Testing blood for diseases like HIV and hepatitis. | High |
| Blood Handling and Storage | Keeping blood components safe and sound. | High |
In short, rules and safety steps are very important for blood transfusions in kids. The FDA and blood banks working together can greatly lower risks. This makes transfusions safer for everyone.
Conclusion: Balancing Benefits and Risks
Blood transfusions save children’s lives but also come with risks. It’s key to understand these risks to make smart choices in pediatric care.
Healthcare teams must weigh the need for a blood transfusion carefully. They look at the child’s health and if other treatments could work. Parents and caregivers need clear info and support during this time.
Advances in Pediatric Blood Transfusions
The future of blood transfusions for kids looks bright. New tech and research might make transfusions safer and more effective. Tools like a child bmi calculator and an ovulation tracker can help too.
By keeping up with new research, healthcare teams and families can make better choices. This focuses on keeping kids healthy and safe.
FAQ
Page:21 What are the risks associated Page:22 with blood transfusions in children?
Blood transfusions in kids can lead to allergic reactions and infections. They might also face transfusion-related acute lung injury (TRALI) and iron overload. Learn more about these risks in our section on blood transfusion risks.
Why are blood transfusions necessary for children?
Kids need blood transfusions after surgery or due to medical conditions. They also need it if they lose a lot of blood. Find out why in our section on blood transfusions in kids.
Q Page:21: What are the short-term effects of blood transfusions in children?
Short-term effects include fever, chills, and nausea. Kids might also vomit or see changes in blood pressure. For more details, check our section on short-term effects.
How can the era Page Page:21:28 ensure the safety of blood transfusions?
Ensuring safety involves matching blood properly and screening for diseases. Following regulatory guidelines is also key. Learn more in our sections on blood matching and FDA oversight.
What is the importance of ABO and Rh compatibility in blood transfusions?
ABO and Rh compatibility are vital to avoid transfusion reactions. We explain why in our section on blood matching.
What are the alternatives to blood transfusions?
Alternatives depend on the situation. We discuss them in our section on evaluating blood transfusion needs.
How can parents be supported through the blood transfusion process?
Supporting parents means giving them information and emotional support. We cover this in our section on supporting families.
What are the long Page:21-term risks associated with blood transfusions in children?
Long-term risks include developing antibodies and chronic diseases. They can also affect immune function. Learn more in our section on long-term risks.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36580030/
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36580030/
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/blood-safety-and-availability























