Did you know millions of people worldwide get life-saving blood transfusions every year? The American Cancer Society says many cancer patients need blood transfusions. This can be a worrying and complex issue. Listing the medical conditions, surgeries, and trauma that lead to the critical need for Why would someone need a blood transfusion.
Blood transfusions are a common medical treatment. They help with cancer, surgery, and injuries. They are used to help patients recover from big blood loss or manage blood cell issues. Knowing why someone needs a blood transfusion helps us support them better.
Key Takeaways
- Blood transfusions are used to treat various medical conditions, including cancer and injuries.
- Many cancer patients require blood transfusions as part of their treatment.
- Blood transfusions help patients recover from significant blood loss.
- We use blood transfusions to manage conditions that affect blood cell production.
- Understanding the need for a blood transfusion is key for patient care.
Understanding Blood Transfusions
It’s important for patients to know about blood transfusions. They are a key part of medical care. They help treat many conditions, from severe injuries to blood disorders.
What Is a Blood Transfusion?
A blood transfusion adds blood or blood parts to a patient’s blood. The National Cancer Institute says it’s key for those who have lost a lot of blood. This can happen due to surgery, injury, or disease.
Transfusions can include different parts:
- Red blood cells: to carry oxygen
- Platelets: to help blood clot
- Plasma: carries cells, proteins, and more
- Cryoprecipitate: a source of clotting factors
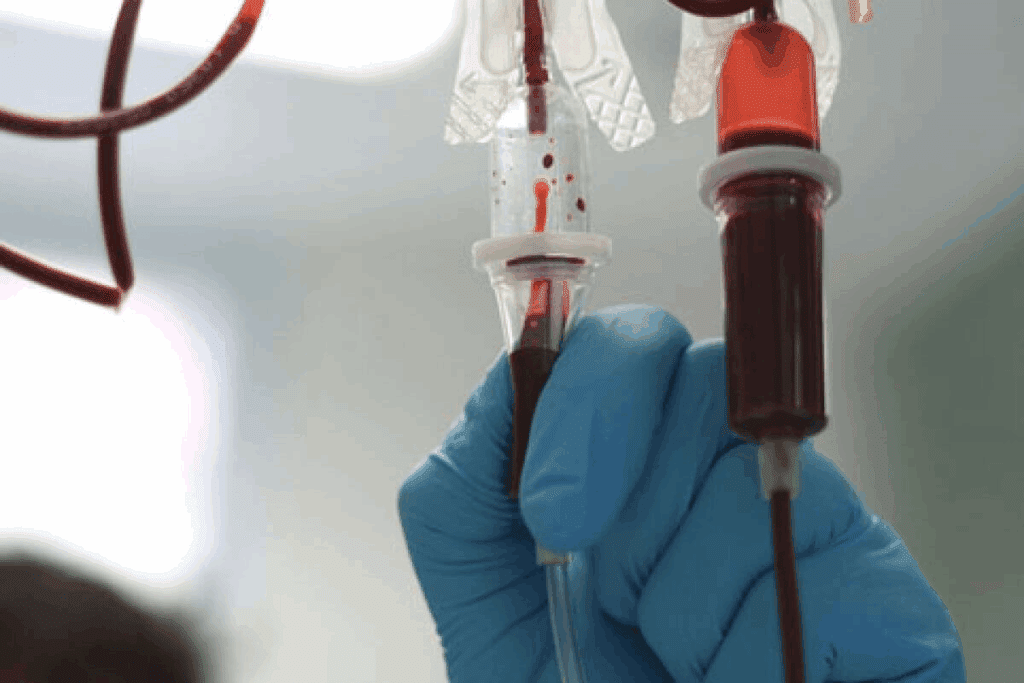
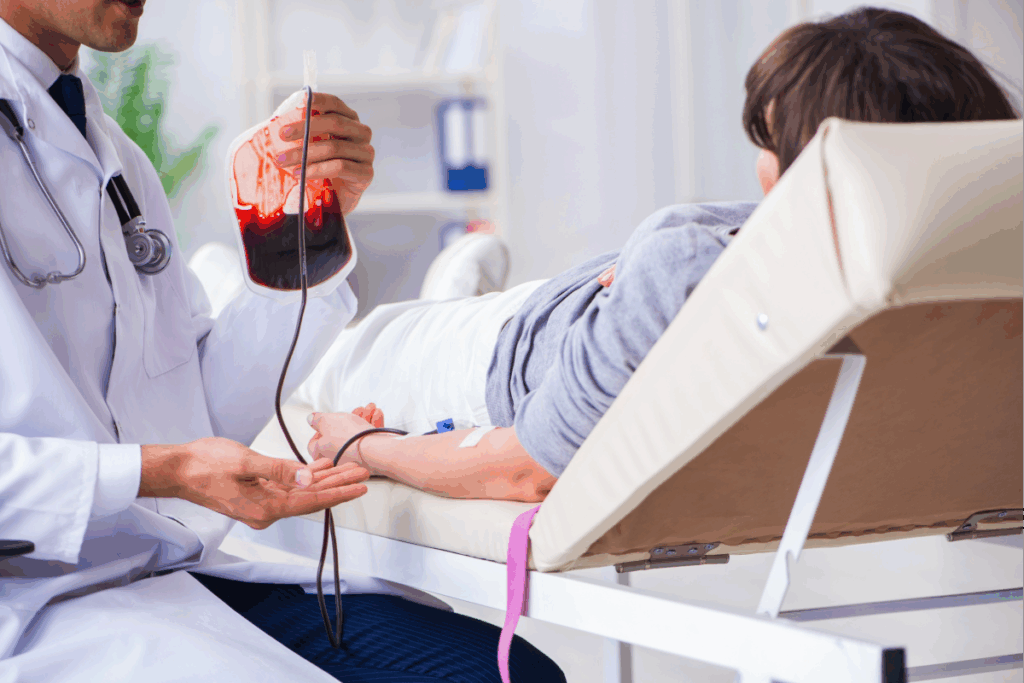
How Are Blood Transfusions Performed?
The transfusion process is safe and precise. First, a doctor checks if a transfusion is needed. They test the patient’s blood type to match it with the donated blood.
| Blood Component | Purpose | Compatibility Test |
| Red Blood Cells | To increase red blood cell mass and improve oxygen delivery | ABO and Rh typing |
| Platelets | To prevent or treat bleeding due to low platelet count | Cross-matching may be performed |
| Plasma | To replace clotting factors and other proteins | ABO compatibility |
After checking compatibility, the transfusion is given through an IV. It’s done in a hospital or clinic with doctors watching closely. This ensures the patient’s safety.
The Importance of Blood
Blood is vital for our bodies. It carries oxygen, fights infections, and helps us heal. It also transports nutrients and keeps our body temperature stable. Let’s look at what makes up blood and why it’s so important.
Components of Blood
Blood has several key parts, each with its own role. These include:
- Red blood cells, which carry oxygen
- White blood cells, vital for fighting infections
- Platelets, important for blood clotting
- Plasma, the liquid part that carries nutrients and waste
Keeping these parts in balance is essential for our health. Any imbalance can cause health problems, sometimes needing a blood transfusion.
| Component | Function |
| Red Blood Cells | Carry oxygen throughout the body |
| White Blood Cells | Fight infections and support immune function |
| Platelets | Help blood to clot and prevent excessive bleeding |
| Plasma | Transports nutrients, hormones, and waste products |
Why Blood is Vital for Health
Blood is essential for our health. It delivers oxygen and nutrients, removes waste, and helps regulate body temperature. It also plays a big role in our immune system, helping us fight infections and heal.
Without enough healthy blood cells, we can face health problems like anemia and bleeding disorders. Understanding blood’s importance and the role of blood transfusions is key to appreciating medical care.
Common Reasons for Blood Transfusions
It’s important for patients and doctors to know why blood transfusions happen. These transfusions are key in many medical situations. They act as a lifeline in critical times.
Injury and Trauma
Big injuries or trauma can cause a lot of blood loss. This is when a blood transfusion is needed. It helps replace lost blood and keeps vital organs getting enough oxygen. This is true for major accidents, severe injuries, or trauma where a lot of blood is lost.
Surgical Procedures
Some surgeries can also cause a lot of blood loss. Blood transfusions are then needed to replace lost blood. This helps keep the patient stable during and after surgery. Orthopedic surgeries, cardiac surgeries, and organ transplants often require blood transfusions.
Blood Disorders
Some blood disorders, like anemia, leukemia, or lymphoma, may need blood transfusions. These conditions can affect blood cell production or function. Transfusions are used to supplement or replace these affected cells.
In short, blood transfusions are essential for treating many medical issues. This includes injuries, surgical problems, and blood disorders. Knowing why they’re needed helps us see their importance in healthcare.
Cancers That Might Require Blood Transfusions
Certain cancers may need blood transfusions to help patients recover. Blood transfusions are key in cancer care. They help ease symptoms and improve treatment results.
Leukemia and Lymphoma
Leukemia and lymphoma are blood cancers. They affect the body’s blood cell production. Patients often need blood transfusions to replace damaged cells.
Leukemia causes abnormal white blood cells to grow too much. Lymphoma affects the lymphatic system, which is part of the immune system.
Types of Leukemia:
- Acute Lymphoblastic Leukemia (ALL)
- Acute Myeloid Leukemia (AML)
- PageSize:
- Chronic Lymphocytic Leukemia (CLL)
- Chronic Myeloid Leukemia (CML)
PageSize:>
| Leukemia Type | Common Symptoms | Treatment Approaches era | |
| ALL | Fatigue, infections, bruising | Chemotherapy, targeted therapy | |
| AML | Shortness of breath, infections, | bleeding | Chemotherapy, bone marrow transplant |
Myeloma
Myeloma is a cancer of plasma cells in the bone marrow. It causes anemia, bone pain, and infections. Blood transfusions help manage these issues.
Solid Tumors
Solid tumors start in organs or tissues, like breast or colon cancer. They might need blood transfusions if surgery or chemotherapy causes blood loss or anemia.
Knowing what cancer patients need is key to good care. Blood transfusions can greatly improve their quality of life during treatment.
Cancer Treatments and Blood Loss
Cancer treatments like chemotherapy and radiation therapy can harm blood cells. This might lead to the need for blood transfusions. It’s key to understand these effects for better patient care.
Chemotherapy’s Impact on Blood Cells
Chemotherapy attacks fast-growing cells, including cancer and blood-making cells in the bone marrow. This can lower the count of red, white blood cells, and platelets.
Effects on Blood Cells:
- Anemia: Fewer red blood cells cause fatigue and weakness.
- Neutropenia: Less white blood cells make infections more likely.
- Thrombocytopenia: Fewer platelets can lead to bleeding issues.
Radiation Therapy Effects
Radiation therapy can also harm the bone marrow’s blood-making ability. This is more likely if the treatment area is the pelvis, spine, or ribs.
The effects of radiation on blood cells are similar to chemotherapy. It can cause anemia, neutropenia, or thrombocytopenia.
| Treatment Type | Potential Effects on Blood Cells |
| Chemotherapy | Anemia, Neutropenia, Thrombocytopenia |
| Radiation Therapy | Anemia, Neutropenia, Thrombocytopenia (depending on the area treated) |
Both chemotherapy and radiation therapy need close watch on blood cell counts. This helps decide if blood transfusions are needed to avoid complications.
Signs Someone Might Need a Blood Transfusion
It’s important to know when someone might need a blood transfusion. We’ll talk about the signs that show a patient might need one. This includes symptoms of severe anemia and other serious conditions.
Symptoms of Severe Anemia
Severe anemia means not enough red blood cells or hemoglobin. The symptoms can be very clear and include:
- Fatigue and Weakness: Feeling very tired or weak, even after resting or doing little.
- Pale Skin: Skin looks pale because of less hemoglobin.
- Shortness of Breath: Hard to breathe or feel winded, even when sitting or doing light activities.
These signs happen because the body’s tissues don’t get enough oxygen. Red blood cells usually carry oxygen. If you’re feeling these symptoms, see a doctor right away.
Other Warning Signs
There are other signs that might mean someone needs a blood transfusion. These include:
- Dizziness or Lightheadedness: Feeling like you might faint because of poor blood flow and oxygen to the brain.
- Rapid Heartbeat: Heart beats faster to make up for not enough red blood cells or hemoglobin.
- Chest Pain: Chest pain can happen if the heart works too hard to get oxygen to the body’s tissues.
| Signs | Description |
| Fatigue and Weakness | Feeling extremely tired or weak |
| Pale Skin | Noticeable paleness due to reduced hemoglobin |
| Shortness of Breath | Difficulty breathing even at rest |
| Dizziness or Lightheadedness | Feeling like you might pass out |
| Rapid Heartbeat | Increased heart rate to compensate for lack of red blood cells |
| Chest Pain | Pain due to the heart working harder |
If you notice any of these signs or symptoms, get medical help fast. A doctor can decide if a blood transfusion is needed based on your situation.
Pre-Transfusion Testing and Compatibility
Pre-transfusion testing is key to making blood transfusions safe and effective. We know how important it is to prevent bad reactions and keep patients safe.
The main goal is to check if the blood is compatible. This means looking at the blood type and other factors to avoid bad reactions. Making sure the blood is compatible is a big deal for patient safety.
Importance of Blood Typing
Blood typing is a big part of pre-transfusion testing. We find out the patient’s blood group to make sure the donated blood is safe. The main groups are A, B, AB, and O, each with its own traits.
Getting the blood type right is key to avoid serious reactions. These reactions can be very dangerous.
- The ABO blood group system is the most critical factor in determining compatibility.
- Rh factor is another important consideration, as it can also impact the compatibility of the blood.
Knowing the patient’s blood type helps us pick the right blood for them. This makes the treatment safer and more effective.
Crossmatching Process
The crossmatching process is a final check to make sure the blood is safe. It mixes the donor’s red blood cells with the recipient’s serum to look for bad reactions. A compatible match is key for a safe transfusion.
“The crossmatch is the final check before transfusion, ensuring that the blood is safe for the recipient.”
AABB Standards
This process is very detailed and important. We do it to find any problems that could cause bad reactions. This way, we make sure the transfusion is safe and works well.
- The donor’s red blood cells are mixed with the recipient’s serum.
- The mixture is then observed for signs of hemolysis or agglutination.
- If no adverse reaction is observed, the blood is deemed compatible for transfusion.
Through pre-transfusion testing, like blood typing and crossmatching, we make blood transfusions safer and more effective. Our strict testing ensures patients get the best care.
Risks and Benefits of Blood Transfusions
Choosing to get a blood transfusion means looking at the good and the bad. Blood transfusions are key in medical care. They help with many health issues, from serious injuries to big surgeries and serious diseases.
Potential Risks Involved
Even though blood transfusions can save lives, they also have risks. These include:
- Transfusion Reactions: The body might react to the blood, causing mild to severe problems.
- Transmission of Infections: Though rare, there’s a chance of getting infections from the blood.
- Iron Overload: Getting blood too often can lead to too much iron in the body, harming organs.
| Risk | Description | Prevention/ Management |
| Transfusion Reactions | Immune response to transfused blood | Careful blood typing and cross-matching |
| Transmission of Infections | Rare risk of infectious agents | Strict screening of blood donors |
| Iron Overload | Accumulation of iron from frequent transfusions | Monitoring iron levels, chelation therapy |
Benefits of Receiving Blood
Despite the risks, blood transfusions have big advantages, including:
- Improved Oxygen Delivery: They help get more oxygen to tissues and organs.
- Reduced Symptoms: They can make symptoms of anemia, like tiredness and short breath, better.
- Enhanced Quality of Life: They can improve how well patients feel and live.
It’s important to know the risks of blood transfusions and benefits of blood transfusions. This helps patients and doctors make smart choices about treatment. While there are risks, the good often outweighs them, which is true in serious cases.
Deciding if a blood transfusion is needed depends on many things. It looks at the patient’s health, why the transfusion is needed, and other treatment options. By looking at the risks and benefits, patients can understand why blood transfusions are needed and how they help in treatment.
Alternatives to Blood Transfusions
Blood transfusions are common for many medical issues. But, there are other ways to help patients. These alternatives can make life better for those with cancer or chronic diseases.
Erythropoiesis-Stimulating Agents
Erythropoiesis-stimulating agents (ESAs) boost red blood cell production. They’re great for people with chronic kidney disease or cancer patients. ESAs can cut down on the need for blood transfusions.
Benefits of ESAs:
- Reduced need for blood transfusions
- Improved hemoglobin levels
- Enhanced quality of life for patients with chronic diseases
Iron Supplements
Iron deficiency leads to anemia, which iron supplements can fix. These supplements raise iron levels, helping make more red blood cells. Iron supplements come in tablets and injections.
“Iron supplementation is a cornerstone in the management of iron deficiency anemia, providing a simple and effective solution.”
— Medical Guidelines
It’s important for patients to take the right amount of iron. They should talk to their doctor to find the best treatment.
Emotional Aspects of Blood Transfusions
Getting a blood transfusion is more than just a medical act. It deeply affects a person’s emotions and mind. Patients may feel scared, worried, relieved, or thankful.
Psychological Impact on Patients
The mind of a patient can be greatly affected by blood transfusions. Anxiety and fear are common feelings. These come from worries about the transfusion’s safety and success. Yet, some feel relief knowing it could save their life.
Patients might fear infections or bad reactions. This can harm their mental health. It’s key for doctors to listen and reassure them.
Support Systems for Patients
Having a strong support network is vital for those getting blood transfusions. Family and friends offer much-needed emotional support. They help patients deal with the stress and fear of the procedure.
Doctors and nurses also play a big part. They guide, reassure, and care for patients during the transfusion. Clear communication and understanding from healthcare staff can ease patient worries.
- Emotional support from loved ones
- Guidance from healthcare providers
- Access to counseling services
With a good support system, patients can face the emotional hurdles of blood transfusions better. This leads to better overall health and well-being.
How to Prepare for a Blood Transfusion
Preparing for a blood transfusion is important to reduce anxiety and ensure success. The process can seem scary, but with the right help, patients can feel more confident.
Medical Preparations
Before a blood transfusion, several steps are needed. We make sure the patient’s blood type is known to avoid bad reactions. This includes checking the patient’s medical history and current health.
Patients usually have blood tests to find their blood group and check for antibodies. This is key to making sure the blood is compatible.
What to Expect During the Procedure
During the transfusion, patients are watched closely for any signs of a reaction. We use advanced medical tools to keep an eye on their vital signs and make sure everything is safe.
Medical experts say, “A blood transfusion is a complex process that needs careful monitoring and patient care.”
“The key to a successful transfusion lies in meticulous preparation and attentive care during the procedure.”
Patients can expect the transfusion to be given slowly and with careful attention. We aim to make this experience as comfortable as possible.
Post-Transfusion Care
After a blood transfusion, patients need careful watching. This ensures their safety and the treatment’s success. We focus on post-transfusion care, which includes watching for bad reactions and long-term health.
Monitoring for Adverse Reactions
Patients are watched closely for bad reactions after a transfusion. We track their vital signs and look for symptoms like fever or shortness of breath. If any odd symptoms show up, quick medical help is needed.
Long-Term Considerations for Patients
Patients who have had blood transfusions face long-term health issues. The number of transfusions needed varies by medical condition. We help patients figure out the best treatment and when more transfusions are needed.
Understanding post-transfusion care helps patients manage their treatment and recovery. We aim to offer full support during the transfusion process.
FAQ
Why do people need blood transfusions?
People need blood transfusions when they lose blood due to injury, surgery, or illness. They also need it when their blood cells don’t work right. Blood transfusions help replace lost blood cells and ensure tissues get enough oxygen.
What is a blood transfusion?
A blood transfusion is when we move blood or blood parts from a donor to a patient. This can include red blood cells, platelets, plasma, or other parts, based on what the patient needs.
Why do cancer patients need blood transfusions?
Cancer patients might need blood transfusions because of chemotherapy, radiation, or the cancer itself. For example, those with leukemia or lymphoma might get anemia or low platelet counts, needing transfusions.
Can you donate blood if you have cancer?
Usually, people with cancer can’t donate blood because of the risk of cancer cells or other problems. But, it depends on the cancer type, treatment, and other factors.
How many blood transfusions can a person have?
How many transfusions a person can have varies based on their health and needs. Some might need many transfusions, while others might only need one.
What are the signs that someone might need a blood transfusion?
Signs that might mean someone needs a transfusion include severe anemia symptoms like fatigue, shortness of breath, or dizziness. Also, low blood cell counts or active bleeding are signs.
How is blood type compatibility determined for transfusions?
We check the patient’s blood type and match it with donated blood of the same type. This makes transfusions safe and reduces the risk of bad reactions.
What are the risks and benefits of blood transfusions?
Blood transfusions can have risks like allergic reactions or complications. But, for patients with specific needs, the benefits like better oxygen delivery and reduced symptoms often outweigh these risks.
Are there alternatives to blood transfusions?
Yes, there are alternatives like erythropoiesis-stimulating agents (ESAs) and iron supplements. They help make more red blood cells or treat anemia.
How can patients prepare for a blood transfusion?
Patients should follow their doctor’s instructions to prepare for a transfusion. This might include giving medical history, blood tests, and getting guidance on what to expect during the procedure.
What is post-transfusion care like?
After a transfusion, patients are watched for any bad reactions. Their doctor will also give them advice on long-term care and follow-up appointments to make sure the transfusion was successful and the patient is okay.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2581075