
Did you know thousands of people are diagnosed with a condition that looks like leukemia but isn’t? This condition is called Myelodysplastic Syndrome (MDS). It’s a group of disorders caused by blood cells that don’t form right or work well. MDS symptoms are similar to leukemia, making it important to know the difference.
We’re here to help you learn about MDS. We’ll cover its symptoms and causes. Knowing what MDS is and how it affects the body is key. It helps us understand why getting the right diagnosis and treatment is so important. MDS is a unique condition that needs a detailed plan to manage its effects on patients’ lives.
Key Takeaways
- MDS is often confused with leukemia due to similar symptoms.
- Understanding MDS is key for accurate diagnosis and treatment.
- MDS is marked by blood cells that don’t form or work right.
- Knowing MDS symptoms and causes is vital.
- MDS needs a detailed treatment plan.
What Is Myelodysplastic Syndrome?
Myelodysplastic syndrome (MDS) is a condition where the bone marrow can’t make healthy blood cells. It’s a complex disorder that affects blood cell production, causing health problems.
Definition and Overview
MDS means the bone marrow can’t make enough healthy blood cells. This includes red blood cells, white blood cells, and platelets. It can cause anemia, infections, and bleeding disorders because of the lack of these cells.
The bone marrow fails to work right in MDS. It should make stem cells that turn into different blood cells. But in MDS, this process goes wrong, leading to dysplastic cells that are not good enough or not made in enough numbers.
Types of Myelodysplastic Syndrome
MDS is not just one disease but a group of disorders with different features. It’s classified based on which blood cells are affected and any genetic changes.
There are several types of MDS, including:
- Refractory Anemia (RA): This is when there’s anemia with too few red blood cells.
- Refractory Anemia with Ringed Sideroblasts (RARS): A subtype of RA with ringed sideroblasts in the bone marrow.
- Refractory Cytopenia with Multilineage Dysplasia (RCMD): This involves dysplasia in multiple blood cell lines.
- Refractory Anemia with Excess Blasts (RAEB): This is when there’s an increased number of immature blast cells in the bone marrow.
Knowing the specific type of MDS is key to understanding the prognosis and treatment plan. We’ll look at how to diagnose and treat MDS in the next sections.
Symptoms Page of Myelodysplastic Syndrome
Knowing the symptoms of Myelodysplastic Syndrome (MDS) is key for early treatment. MDS is a group of disorders that affect blood cells. This can lead to anemia and other issues.
Early Stage Symptoms to Watch For
In the early stages, MDS symptoms can be mild and easy to miss. Common signs include fatigue, shortness of breath, and pale skin. These are often due to anemia from not enough red blood cells.
Other early symptoms include:
- Weakness
- Dizziness or lightheadedness
- Headaches
- Cold hands and feet
Advanced Stage Symptoms
As MDS gets worse, symptoms can worsen. They may include:
- Increased frequency of infections due to low white blood cell counts
- Bleeding disorders, such as easy bruising or bleeding gums, resulting from low platelet counts
- Severe anemia requiring frequent blood transfusions
It’s vital for patients and healthcare providers to watch for these symptoms. This ensures timely treatment.
How Myelodysplastic Syndrome Differs from Leukemia
MDS and leukemia share some traits, but they are quite different. Knowing these differences helps doctors create better treatment plans.
Key Differences in Symptoms
MDS symptoms can be hard to spot and might look like leukemia. Yet, there are clear differences. MDS often leads to anemia, infections, and bleeding problems.
Leukemia, on the other hand, can cause fatigue, weight loss, and frequent infections. It might also cause bone pain and swelling from cancer cells.
- MDS Symptoms: Fatigue, weakness, shortness of breath, and recurrent infections.
- Leukemia Symptoms: Bone pain, swollen lymph nodes, fever, and night sweats.
Diagnostic Criteria
To diagnose MDS, doctors do a bone marrow biopsy and genetic tests. They look for abnormal bone marrow cells and the number of blasts.
For leukemia, doctors also do a bone marrow biopsy. They use tests like immunophenotyping and genetic analysis to find the type of leukemia.
| Characteristics | Myelodysplastic Syndrome (MDS) | Leukemia |
| Primary Feature | Dysplastic bone marrow cells, ineffective hematopoiesis | Malignant proliferation of leukemic cells |
| Symptoms | Anemia, infections, bleeding disorders | Bone pain, swollen lymph nodes, fever, night sweats |
| Diagnostic Approach | Bone marrow biopsy, genetic testing | Bone marrow biopsy, immunophenotyping, genetic analysis |
Understanding the differences between MDS and leukemia helps doctors give better diagnoses and treatments. This leads to better care for patients.
Risk Factors for Myelodysplastic Syndrome
Myelodysplastic syndrome (MDS) can be caused by genetic and environmental factors. Understanding these risk factors helps us know who might be more at risk. It also helps us take steps to prevent it.
Genetic Predispositions
Genetics play a big role in MDS. Some chromosomal changes, like deletions on chromosomes 5, 7, and 20, raise the risk of MDS.
- Chromosomal Deletions: These deletions can mess up cell function, leading to MDS.
- Genetic Syndromes: Syndromes like Fanconi anemia also increase MDS risk.
Environmental Factors
Some environmental factors can also raise MDS risk. These include:
- Chemical Exposure: Being exposed to chemicals like benzene increases MDS risk.
- Radiation Exposure: Too much radiation can also raise MDS risk.
- Previous Chemotherapy: People who have had chemotherapy, like with alkylating agents, are at higher risk.
| Risk Factor | Description |
| Chromosomal Deletions | Deletions involving chromosomes 5, 7, and 20 |
| Genetic Syndromes | Conditions like Fanconi anemia |
| Chemical Exposure | Exposure to benzene and other harmful chemicals |
| Radiation Exposure | High levels of radiation |
| Previous Chemotherapy | Especially with alkylating agents |
Diagnosing Myelodysplastic Syndrome
To diagnose MDS, doctors use several steps. First, they do blood tests to find any odd blood cell counts.
Blood Tests and Bone Marrow Biopsy
The first step is blood tests to check for low blood cell counts. These tests show how severe the condition is and guide further tests.
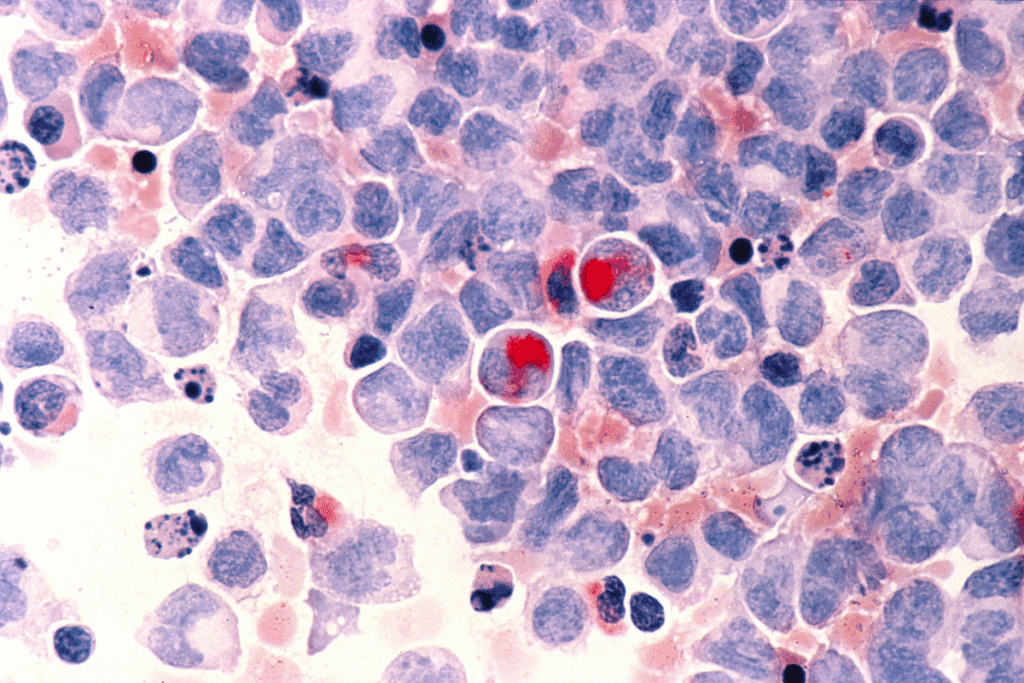
A bone marrow biopsy is a key test for MDS. It takes a bone marrow sample for a microscope check. This test looks at cell types and any odd cells, helping to diagnose MDS.
Key findings from a bone marrow biopsy include:
- Cellularity: The percentage of the bone marrow cavity occupied by hematopoietic cells.
- Morphology: The shape and structure of cells, which can indicate dysplasia or abnormal development.
- Cytogenetic analysis: Examination of the chromosomes in the bone marrow cells to identify genetic abnormalities.
Additional Diagnostic Procedures
Other tests may also be used to help diagnose MDS. These include:
- Cytogenetic testing to identify chromosomal abnormalities.
- Molecular testing to detect specific genetic mutations associated with MDS.
- Imaging studies, such as X-rays or CT scans, to assess any complications or related conditions.
The following table summarizes the key diagnostic procedures for MDS:
| Diagnostic Procedure | Purpose |
| Blood Tests | To identify cytopenias and assess blood cell counts. |
| Bone Marrow Biopsy | To examine the bone marrow’s cellularity and morphology. |
| Cytogenetic Testing | To detect chromosomal abnormalities. |
| Molecular Testing | To identify specific genetic mutations. |
By combining these test results, we can accurately diagnose MDS. Then, we can create a treatment plan that fits the patient’s needs.
Treatment Options for Myelodysplastic Syndrome
Myelodysplastic syndrome (MDS) treatment is complex. It includes supportive care, medications, and therapies tailored for each patient. The goal is to manage symptoms, improve life quality, and slow disease growth.
Every patient’s journey with MDS is different. So, treatment plans are made just for them. The choice of treatment depends on the MDS subtype, the patient’s health, and their specific risk factors.
Supportive Care and Transfusions
Supportive care is key in managing MDS. It aims to ease symptoms and enhance life quality. Blood transfusions are a big part of this, helping to increase red blood cells and reduce anemia symptoms.
Key aspects of supportive care include:
- Regular blood transfusions to manage anemia and thrombocytopenia
- Administration of growth factors to stimulate blood cell production
- Use of antibiotics to treat infections
Patients may also get medications for specific symptoms or complications. For example, iron chelation therapy can help with iron overload from frequent transfusions.
“The cornerstone of MDS management is supportive care, which not only improves the quality of life but also helps in navigating the complexities of the disease.”
– Expert in Hematology
Let’s look at the treatment options for MDS in a structured way:
| Treatment Approach | Description | Benefits/Outcomes |
| Supportive Care | Management of symptoms through transfusions and medications | Improved quality of life, reduced symptoms |
| Targeted Therapies | Medications aimed at improving bone marrow function | Potential improvement in blood cell production, reduced risk of progression |
| Immunosuppressive Therapy | Treatment to suppress the immune system in specific cases of MDS | May improve blood counts in certain patients |
Finding the right treatment can be tough. So, it’s vital for patients to work closely with their healthcare team. Together, they can find the best treatment plan for each patient’s needs.
Living with Myelodysplastic Syndrome
Living with myelodysplastic syndrome (MDS) is more than just treatment. It’s about managing the condition and improving life quality. MDS management means treating the syndrome and making life better.
Coping Strategies for Patients
Coping with MDS requires many strategies. A healthy lifestyle is key, including a balanced diet and exercise. Stress management, like meditation or yoga, helps with emotional challenges.
- Staying informed about MDS and its management
- Building a support network of family, friends, and support groups
- Engaging in activities that bring joy and fulfillment
Working with your healthcare team is vital. They help create a care plan that covers medical and well-being aspects.
Support Resources and Communities
Support is essential for MDS patients. Support groups offer community and understanding. They are a great resource for connections and advice.
Organizations also provide help, like educational materials and counseling. Patients and families should use these services to understand MDS better.
“The support I received from my MDS support group has been invaluable. It’s comforting to know I’m not alone in this journey.”
A patient with MDS
Living with MDS is tough, but with the right support, patients can live fulfilling lives. We’re here to provide care and resources every step of the way.
Research and Advancements in Treatment Page
Medical research is making big strides in understanding myelodysplastic syndrome (MDS). We’re seeing a big change in how we treat this complex condition. This change comes from ongoing research and clinical trials.
Clinical Trials and Studies
Clinical trials are key in finding new MDS treatments. Many studies are looking at different ways to treat the disease. They’re exploring targeted therapies and immunotherapies to help patients more.
Some important areas being studied include:
- The use of targeted therapies to address specific genetic mutations associated with MDS
- The development of immunotherapies designed to enhance the body’s immune response against cancer cells
- The investigation of combination therapies that pair different treatment approaches to achieve better results
Emerging Therapies in Development
New therapies are showing great promise for MDS treatment. These include:
| Therapy Type | Description | Potential Benefits |
| Targeted Therapy | Drugs that target specific genetic mutations | More precise treatment with potentially fewer side effects |
| Immunotherapy | Treatments that enhance the immune system’s ability to fight cancer | Potential for improved outcomes by leveraging the body’s natural defenses |
| Combination Therapy | Approaches that combine different treatments | May offer better efficacy by attacking the disease from multiple angles |
As research keeps moving forward, we’ll see new and innovative MDS treatments. These emerging therapies could greatly improve patient outcomes. They also promise to enhance the quality of life for those with MDS.
Myelodysplastic Syndrome Prognosis and Outcomes
Myelodysplastic syndrome (MDS) has a prognosis that depends on many factors. These include the type of MDS and the patient’s age. Knowing these factors helps doctors choose the best treatment and predict how well a patient will do.
MDS is a complex disease, and its outlook varies a lot among patients. Important factors include the type of MDS, the patient’s age, and genetic changes.
Survival Rates and Statistics
Thanks to new treatments, MDS survival rates have gotten better. But, these rates can change a lot based on the MDS type and other factors.
Studies show that survival for MDS patients varies. For example, those with lower-risk MDS usually do better than those with higher-risk MDS.
| MDS Subtype | Median Survival (Years) |
| Lower-risk MDS | 5-10 |
| Higher-risk MDS | 0.8-2 |
Factors Influencing Prognosis
Several things can affect how well a patient with MDS will do. These include:
- MDS Subtype: The type of MDS matters a lot. Some types are more likely to have a good outcome.
- Patient Age: Older patients often face a tougher time because of other health issues and less energy.
- Genetic Abnormalities: Some genetic changes can make the prognosis worse. These changes can increase the risk of turning into acute myeloid leukemia (AML).
- Blood Counts: How low the blood counts are can also affect the prognosis. Severe low counts usually mean a worse outcome.
Understanding these factors helps doctors give a better prognosis. They can then plan a treatment that fits the patient’s specific needs.
Conclusion: Understanding and Managing Myelodysplastic Syndrome
Myelodysplastic syndrome (MDS) is a complex condition that needs timely and right management. Early detection is key to better patient outcomes. It’s vital to grasp the importance of early MDS detection.
Early Detection and Patient Support
Early detection is very important. It lets for actions that can greatly improve MDS patients’ lives. We also stress the need for full patient support for MDS. This includes access to care resources and communities that offer myelodysplastic syndrome support.
By knowing about MDS and its care, we aim for better patient care and results. Our goal is to give top-notch healthcare with full support for international patients. We make sure they get the care they need.
FAQ
What is myelodysplastic syndrome (MDS)?
Myelodysplastic syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. This often leads to bone marrow failure.
What are the symptoms of myelodysplastic syndrome?
Symptoms include fatigue, shortness of breath, and infections. These happen because of low blood cell counts. As MDS gets worse, symptoms can get worse too. This may include bleeding, anemia, and a higher risk of infections.
How is myelodysplastic syndrome different from leukemia?
MDS and leukemia are both blood disorders. But MDS is when the bone marrow can’t make healthy blood cells. Leukemia is when abnormal white blood cells grow too much.
What are the risk factors for developing myelodysplastic syndrome?
Risk factors include genetic predispositions. Exposure to certain chemicals or radiation also increases risk. So does previous chemotherapy or radiation therapy.
How is myelodysplastic syndrome diagnosed?
Diagnosis starts with blood tests to check for abnormal blood cell counts. Then, a bone marrow biopsy is done. This examines the bone marrow’s cellular structure and function.
What are the treatment options for myelodysplastic syndrome?
Treatment options include supportive care like blood transfusions. Medications to stimulate blood cell production are also used. Targeted therapies address specific genetic mutations.
Can myelodysplastic syndrome be cured?
Some cases of MDS can be managed well. But a cure is usually only possible through allogeneic stem cell transplantation. This is a complex and high-risk procedure.
How can patients cope with myelodysplastic syndrome?
Coping strategies include a healthy lifestyle and stress management. Seeking support from healthcare professionals, family, and support groups is also important.
What is the prognosis for myelodysplastic syndrome?
Prognosis varies based on the type of MDS, the patient’s health, and treatment effectiveness. Survival rates are wide-ranging. It’s hard to predict individual outcomes.
Are there any ongoing research or new treatments for myelodysplastic syndrome?
Yes, research includes clinical trials for new medications and therapies. Studies also aim to understand MDS causes and find new treatment targets.
What is pre-leukemia or smoldering leukemia?
Pre-leukemia or smoldering leukemia are conditions like MDS. They have the chance to turn into acute leukemia. This is when abnormal cells are in the bone marrow.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4664149/


































