Last Updated on December 2, 2025 by Bilal Hasdemir

Immunotherapy has changed how we treat cancer. It uses the body’s immune system to fight cancer cells. But, it doesn’t work for everyone, leaving patients and doctors looking for other options.
When immunotherapy fails, finding the right next step is key. Second-line cancer treatments and salvage therapy offer hope. They provide care that fits each patient’s needs.Listing key restrictions and discussing Options after immunotherapy failure (alternative treatments).
Key Takeaways
- Immunotherapy is used to treat various types of cancer.
- When immunotherapy fails, other treatments are available.
- Second-line cancer treatment and salvage therapy are possible next steps.
- Understanding these options is important for patients and doctors.
- Continuing care is tailored to the patient’s specific needs.
Understanding Immunotherapy Failure
When immunotherapy fails, it’s important to know why. This treatment uses the immune system to fight cancer. But, it can face obstacles.
Common reasons for immunotherapy resistance
Several factors can make immunotherapy less effective. These include the tumor’s traits and how it develops resistance. Some common reasons are:
- Tumor mutational burden: Tumors with few mutations may not trigger an immune response.
- PD-L1 expression: If tumor cells don’t have PD-L1, PD-1/PD-L1 inhibitors won’t work well.
- Tumor microenvironment: An environment that suppresses the immune system can block its action.
How to determine if your treatment isn’t working
To see if immunotherapy is working, regular checks are needed. Important signs include:
- Imaging studies: Scans to see how the tumor is responding.
- Tumor markers: Watching specific biomarkers related to cancer.
- Clinical evaluation: Checking overall health and managing symptoms.
Knowing why immunotherapy fails is key to finding new treatments. By looking at tumor traits and tracking disease, doctors can plan better care.
Comprehensive Evaluation After Treatment Failure
When immunotherapy doesn’t work, a detailed check is needed. This includes advanced tests and a close look at the cancer’s stage. It’s key to figure out the best treatment plan next.
Tumor Mutational Analysis and Biomarker Testing
Tumor mutational analysis looks at the tumor’s genetic changes to find therapy targets. Biomarker testing shows the tumor’s traits and how it might react to treatments. These tests help tailor treatments to fit each person’s cancer.
These tests can show why immunotherapy didn’t work. They might suggest other treatments. For example, some mutations could make the tumor more treatable with specific drugs.
Reassessing Cancer Stage and Disease Progression
Checking the cancer stage and disease progression is important after treatment fails. Imaging and other tests help see how the cancer has changed. This helps doctors pick the best treatments.
This detailed check helps choose the next treatment and find clinical trials. It shows the value of a team approach in fighting cancer that doesn’t respond to first treatments.
Options After Immunotherapy Failure
When immunotherapy doesn’t work, it’s time to look at other treatment options. Patients and doctors need to explore new ways to fight cancer.
Key factors that influence second-line treatment decisions
Choosing the right second-line treatment depends on several things. These include the type of cancer, past treatments, and the patient’s health.
- Cancer Type: Different cancers react differently to treatments.
- Previous Treatments: Past treatments’ success and side effects matter.
- Patient Health: The patient’s health affects how well they can handle more treatment.
| Factor | Influence on Treatment |
| Cancer Type | Determines the most effective treatment approach |
| Previous Treatments | Affects the choice of subsequent treatments |
| Patient Health | Influences the tolerability of further treatment |
The role of multidisciplinary tumor boards in treatment planning
Multidisciplinary tumor boards are key in planning treatment after immunotherapy fails. These teams include experts from different fields working together to find the best treatment.
Benefits of Multidisciplinary Tumor Boards:
- Comprehensive review of patient cases
- Collaboration among specialists
- Access to a broader range of treatment options
Healthcare providers use these boards to consider all factors. This way, they can create second-line treatment plans that fit each patient’s needs.
Targeted Therapy as a Second-Line Approach
When immunotherapy doesn’t work, targeted therapy becomes a good second choice. It targets specific parts of cancer cells that help them grow.
Precision oncology is key in finding these targets. It uses advanced tests to look at a tumor’s genes. This helps doctors pick the best treatment.
Precision Oncology: Matching Treatments to Specific Mutations
Precision oncology uses genetic info to choose treatments. It makes treatments more personal by focusing on the cancer’s specific mutations.
Tumor profiling is a big part of this. It uses next-generation sequencing (NGS) to deeply analyze tumor genetics. This helps find the best therapy targets.
Common Targeted Therapies by Cancer Type
Each cancer type has its own genetic changes. Targeted therapies are made to fight these changes. For example:
- EGFR inhibitors are for non-small cell lung cancer (NSCLC) with EGFR mutations.
- HER2-targeting drugs work well in HER2-positive breast cancer.
- BRAF inhibitors are used in melanoma with BRAF V600E mutations.
By matching the therapy to the cancer and its genes, doctors can offer better treatments. These are for patients who didn’t get better from first treatments.
Chemotherapy Following Immunotherapy
When immunotherapy doesn’t work as hoped, chemotherapy is often considered next. This choice depends on the cancer type, the patient’s health, and past treatments.
Optimal Sequencing of Systemic Therapies
Choosing the right order for treatments like chemotherapy is key. Optimal sequencing means looking at the patient’s past treatments, current health, and cancer details.
| Treatment Sequence | Considerations | Potential Benefits |
| Immunotherapy followed by Chemotherapy | Previous treatment response, Cancer type | Targeted approach to remaining cancer cells |
| Chemotherapy as a standalone second-line treatment | Health status, Cancer stage | Quick reduction in tumor size |
Managing Side Effects and Setting Realistic Expectations
It’s important to manage side effects when starting chemotherapy after immunotherapy. This means watching for adverse reactions and making changes to the treatment plan if needed. It’s also key to set clear expectations with patients about what to expect and possible side effects.
Chemotherapy can cause serious side effects, but with the right care, many patients can keep up with their treatment. Regular check-ups and a team of healthcare professionals are essential in managing these effects.
Combination Therapy Strategies
When immunotherapy alone isn’t enough, combining therapies offers hope for cancer treatment. This method uses several treatments together to beat the limits of single therapies.
Immunotherapy plus targeted therapy combinations
Using immunotherapy with targeted therapy is showing promise in cancer treatment. Targeted therapy targets specific cancer growth factors. Immunotherapy boosts the body’s immune fight against cancer. Together, they might make treatments more effective.
For example, mixing checkpoint inhibitors with targeted therapies can boost the immune fight against tumors. This mix is being tested in clinical trials, with promising results.
Multi-modal treatment approaches
Multi-modal treatments combine different therapies like immunotherapy, targeted therapy, chemotherapy, and radiation. The aim is to attack cancer from all sides for better results.
These treatments can be customized for each patient based on their cancer type, stage, and past treatments. For instance, a patient with a specific genetic mutation might get a mix of targeted therapy and immunotherapy.
| Treatment Combination | Potential Benefits | Current Status |
| Immunotherapy + Targeted Therapy | Enhanced anti-tumor immune response, improved efficacy | Exploration in clinical trials |
| Multi-modal Treatment | Attacking cancer from multiple angles, better outcomes | Customized approaches for individual patients |
Advanced Cellular and Immune Therapies
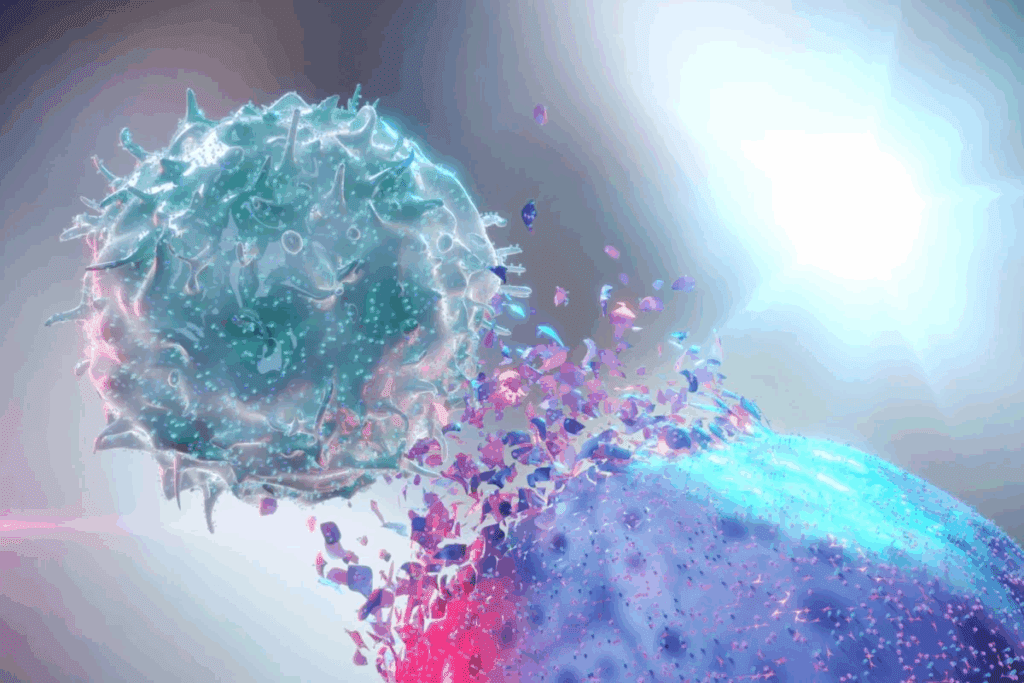
Advanced cellular and immune therapies are changing cancer treatment. They offer hope to those who haven’t seen results from immunotherapy. These new methods aim to boost the body’s fight against cancer cells.
CAR-T Therapy and TIL Therapy Applications
CAR-T (Chimeric Antigen Receptor T-cell) therapy changes a patient’s T cells to target cancer. It’s shown great promise in treating blood cancers. TIL (Tumor-Infiltrating Lymphocyte) therapy expands and reinfuses T cells from tumors. Both are being studied for different cancers.
CAR-T therapy works well for B-cell lymphoma and leukemia that doesn’t respond to treatment. TIL therapy is effective in melanoma and is being looked at for other cancers too.
Bispecific Antibodies and Novel Checkpoint Inhibitors
Bispecific antibodies are made to bind to two targets: a cancer cell and an immune cell. This brings them together to kill the cancer cell. Novel checkpoint inhibitors help overcome resistance to current treatments, boosting the immune system’s fight against tumors.
These treatments are part of a bigger plan to better cancer treatment. By targeting different pathways, bispecific antibodies and novel checkpoint inhibitors give new hope to those with advanced cancer.
Clinical Trials and Emerging Treatment Options
Clinical trials are key for patients to get new treatments for cancer. These studies check if new treatments are safe and work well. They include new therapies not found in regular treatments.
How to Find and Qualify for Appropriate Clinical Trials
Finding the right clinical trial can be hard. But, there are many resources to help. Start by talking to your doctor. They can suggest trials based on your condition and health history.
Online databases also list ongoing trials. This includes cancer vaccine trials and next-generation immunotherapies.
To join a trial, you must meet certain criteria. This includes your cancer type, stage, past treatments, and health. Always check the criteria for each trial you’re interested in.
Promising Investigational Approaches
New treatments are always being developed. Several promising methods are being tested in trials. These include:
- Cancer vaccines to boost the immune system against cancer cells.
- Next-generation immunotherapies that improve on current treatments, aiming for better results and fewer side effects.
Cancer Vaccines in Development
Cancer vaccines are a hopeful area of research. Several vaccines are being tested in trials. They aim to make the immune system fight cancer cells better. Examples include vaccines targeting specific cancer proteins and those that enhance the immune response.
Next-Generation Immunotherapies
Next-generation immunotherapies are a big step forward in cancer treatment. These include:
| Therapy Type | Description | Potential Benefits |
| CAR-T Therapy | A form of immunotherapy that involves removing T cells from the patient’s blood, modifying them to recognize cancer cells, and reinfusing them. | High response rates in certain types of blood cancers. |
| Bispecific Antibodies | Antibodies designed to bind to two different targets, such as a cancer cell and an immune cell, bringing them together to facilitate cancer cell destruction. | Enhanced immune response against cancer cells. |
| Checkpoint Inhibitors | Drugs that release the brakes on the immune system, allowing it to more effectively target and destroy cancer cells. | Improved efficacy in various cancer types. |
These new therapies offer hope for cancer patients, even those who haven’t responded to usual treatments.
Conclusion: Building Your Personalized Treatment Plan
Creating a personalized treatment plan is key for patients who haven’t seen results from immunotherapy. This plan looks at many factors. These include the type of cancer, past treatments, and what the patient wants.
Palliative care is important in cancer treatment. It helps ease symptoms and stress from serious illnesses. Adding palliative care to a treatment plan can greatly improve a patient’s life quality.
Monitoring the disease is also critical. It lets doctors track the disease’s progress and change the treatment plan as needed. By using personalized medicine, disease monitoring, and palliative care, patients get treatments that fit their needs.
Working with a team of healthcare experts helps create a treatment plan that meets a patient’s specific needs. This approach improves their overall health and well-being.
FAQ
What happens if immunotherapy doesn’t work for my cancer treatment?
If immunotherapy doesn’t work, your healthcare team will look into other options. They might suggest targeted therapy, chemotherapy, or clinical trials.
How is it determined if immunotherapy is not working?
To check if immunotherapy is not working, doctors use imaging tests. They look at tumor size and activity. They also watch for new lesions or disease progression.
What is tumor mutational analysis, and how does it help in cancer treatment?
Tumor mutational analysis is genetic testing for tumors. It finds specific mutations. This helps choose treatments that might work better for your tumor.
What are the key factors that influence second-line treatment decisions after immunotherapy failure?
Decisions on second-line treatments depend on several factors. These include cancer type and stage, previous treatments, overall health, and genetic mutations.
How does precision oncology play a role in targeted therapy?
Precision oncology uses tumor genetics to guide treatments. It matches patients with therapies targeting specific tumor mutations or biomarkers.
What are some common targeted therapies used for different types of cancer?
Targeted therapies vary by cancer type. For example, trastuzumab is used for HER2-positive breast cancer. EGFR inhibitors are for lung cancer, and BRAF inhibitors for melanoma. The choice depends on the tumor’s genetics.
How is chemotherapy used after immunotherapy, and what are the considerations for its use?
Chemotherapy might be used if cancer progresses or doesn’t respond to immunotherapy. Considerations include cancer type, stage, previous treatments, and overall health.
What are combination therapy strategies, and how are they used in cancer treatment?
Combination therapy uses multiple treatments together. This can include immunotherapy and targeted therapy. It aims to improve treatment outcomes and overcome resistance.
What are CAR-T therapy and TIL therapy, and how are they used in cancer treatment?
CAR-T therapy modifies T cells to recognize cancer cells. TIL therapy uses T cells from tumors to fight cancer. Both are adoptive cell therapies for certain cancers.
How can I find and qualify for clinical trials for my cancer treatment?
To find clinical trials, search online databases. Talk to your healthcare team or contact cancer research organizations. Eligibility depends on cancer type, stage, and previous treatments.
What is palliative care, and how does it fit into cancer treatment?
Palliative care focuses on relieving symptoms and stress of cancer and its treatment. It’s an important part of cancer care, supporting patients and families at any stage.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9655090/
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9655090/
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/s41416-024-02887-1