Last Updated on November 12, 2025 by
Recent advances in cancer treatment have led to a big change. Immunotherapy for cancer is now a key player. It uses the body’s immune system to fight cancer.
At our institution, we aim to provide top-notch healthcare. We support international patients fully. We look into whether immunotherapy is better than targeted therapy.
Research shows immunotherapy is making big strides in cancer care. It has impressive survival rates and works better when combined with other therapies. Knowing the differences between immunotherapy and targeted therapy is key.
Key Takeaways
- Cancer treatment is becoming more personalized.
- Immunotherapy uses the body’s immune system to fight cancer.
- Recent studies show big advances in immunotherapy.
- Combination therapies are boosting response rates.
- Understanding the differences between therapies is important for patients.
The Evolution of Cancer Treatment Approaches
Cancer treatment has changed a lot, moving from old chemotherapy to new precision medicine. New breakthroughs have brought new ways to fight cancer, making treatments better for patients.
From Conventional Chemotherapy to Precision Medicine
Old treatments used chemotherapy, which had big side effects. Precision medicine changed this by making treatments fit each patient’s cancer. This change came from better genetic sequencing and understanding cancer.
Targeted therapies are a big step forward. They aim only at cancer cells, not healthy ones. This makes treatments better and safer than old chemotherapy.
The Emergence of Novel Therapeutic Strategies
New strategies like immunotherapy have also come up. It uses the body’s immune system to fight cancer. This method has shown great promise, with some patients seeing long-lasting results.
Small molecular targeted therapies are also important. They target specific cancer growth drivers. This keeps treatments strong while lowering the chance of cancer becoming resistant.
Current Landscape of Cancer Treatment Options
Now, there are many ways to treat cancer, like surgery, radiation, and new medicines. The right treatment depends on the cancer type, stage, and the patient’s health.
We’re getting better at treating cancer with a more personal touch. We pick the best treatment for each patient based on their cancer’s unique traits.
Understanding Cancer Immunotherapy
Immunotherapy has changed cancer treatment a lot. It uses the immune system to fight cancer. We’ll look at how it works, its benefits, and the different ways it’s used.
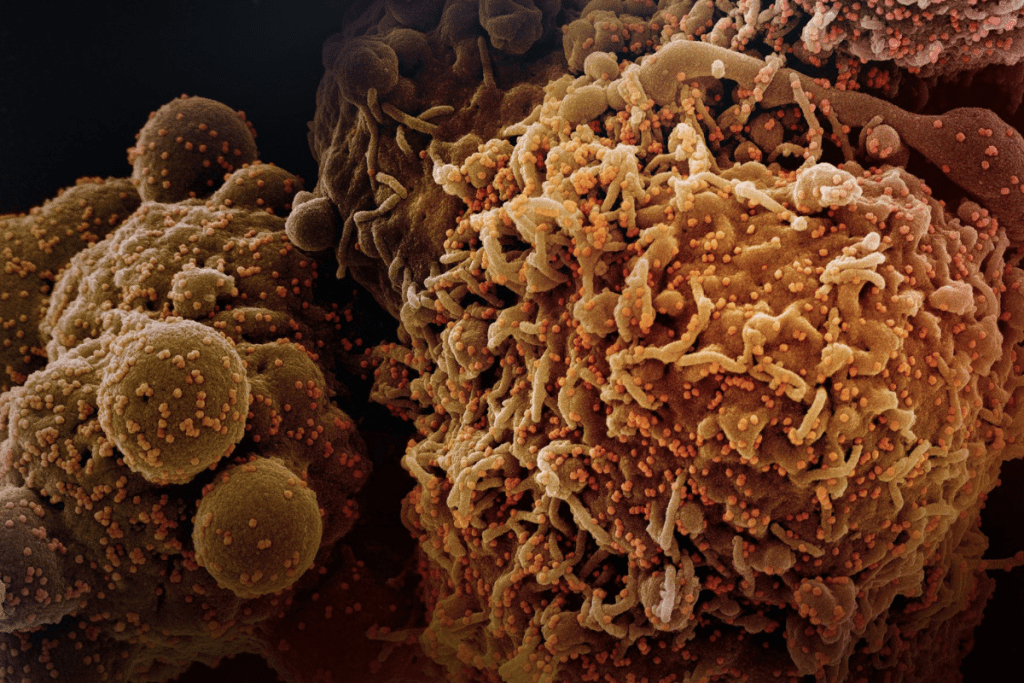
Definition and Fundamental Mechanisms
Immunotherapy, or immune therapy, boosts the immune system to fight cancer better. It makes the body’s defenses stronger to find and destroy cancer cells. This method has shown great promise in treating many cancers.
The immune system is key in fighting cancer. It can spot and kill cancer cells with the help of immune cells like T cells and natural killer cells. Immunotherapy helps the immune system do this job better.
Major Types of Immunotherapy Approaches
There are many immunotherapy types for cancer, each working in its own way. Some main types include:
- Checkpoint Inhibitors: These drugs let the immune system attack cancer cells more freely.
- Cancer Vaccines: These vaccines help the immune system recognize and fight cancer cells.
- Adoptive T-cell Therapy: This method takes T cells, changes them to recognize cancer, and then puts them back in the body.
- Monoclonal Antibodies: These are made antibodies that target specific proteins on cancer cells, making them easier for the immune system to destroy.
Knowing about these methods is important for finding the best treatment for patients. Immunotherapy uses the immune system’s power to offer hope for many cancer types.
Targeted Therapy: The Precision Medicine Approach
Targeted therapy has changed how we fight cancer, giving hope to those with certain genetic changes. It’s a treatment that finds and attacks cancer cells, keeping healthy cells safe.
How Targeted Therapies Identify and Attack Cancer Cells
Targeted therapies find specific traits in cancer cells, like genetic changes or proteins. They use this info to create treatments that hit those traits. This method is more precise and effective than old chemotherapy, which harms both cancer and healthy cells.
For example, some therapies block proteins that help cancer grow. Others send substances to cancer cells, marking them for the immune system to destroy or delivering a poison that kills them.
Common Classes of Targeted Therapies
There are many types of targeted therapies, each working in its own way. Some of the most well-known include:
- Monoclonal Antibodies: These are made in labs to help the immune system fight cancer cells.
- Tyrosine Kinase Inhibitors: These drugs stop enzymes that help cancer cells grow and survive.
- Cancer Growth Inhibitors: These therapies cut off the blood supply to tumors, starving them of nutrients.
Targeted therapy is a game-changer for those with specific genetic changes. It offers a custom treatment that can greatly improve results. By understanding how targeted therapy works and its different types, we see its vital role in cancer treatment.
Efficacy Comparison: Survival and Response Rates
Looking at how well immunotherapy and targeted therapy work in cancer treatment is key. We can learn a lot by checking out clinical trial results. This helps us see which treatment might be better for different cancers.
Immunotherapy Survival Statistics in Clinical Trials
Immunotherapy has shown great promise in trials. For example, pembrolizumab monotherapy gave a 5-year survival rate of 23.2% for advanced NSCLC with high PD-L1 expression. This is a big win, beating traditional chemotherapy.
Some important facts from immunotherapy trials are:
- It has led to better survival rates in cancers like melanoma and NSCLC.
- It has also helped patients live longer without their cancer getting worse.
- Some patients have seen their cancer completely or partially disappear.
Targeted Therapy Outcomes Across Cancer Types
Targeted therapy has also been very effective in treating certain cancers. It works by focusing on specific genetic changes or biomarkers. This leads to better results for patients, like higher response rates in cancers with specific genetic changes.
Some key points about targeted therapy are:
- It has shown high response rates in cancers with specific genetic mutations.
- It has helped patients live longer without their cancer getting worse.
- It has also improved overall survival rates in some cancers.
Head-to-Head Comparisons Where Available
While we don’t have many direct comparisons, the data we do have is interesting. Immunotherapy and targeted therapy both have their advantages. Sometimes, one is better, and sometimes the other is.
For example, a study found that pembrolizumab was better than chemotherapy for NSCLC patients with high PD-L1 expression. This kind of comparison helps us figure out the best treatment for different patients.
Patient Selection and Biomarker Considerations
Picking the right treatment for cancer is all about understanding each patient’s unique needs. Cancer is complex, so treatments must be tailored to fit each person’s situation.
Predictive Biomarkers for Immunotherapy Response
Biomarkers help doctors know who will benefit from immunotherapy. PD-L1 expression is a key marker, but it can change due to many factors.
New biomarkers like tumor mutational burden (TMB) and microsatellite instability (MSI) are also promising. TMB, in particular, has been linked to better results with certain treatments.
Genetic Testing for Targeted Therapy Eligibility
Genetic tests are vital for finding the right targeted therapy. Next-generation sequencing (NGS) helps find specific mutations in tumors. For instance, EGFR mutations in lung cancer and HER2 amplifications in breast cancer guide treatment.
Genetic testing helps doctors tailor treatments to match each tumor’s unique traits. This approach boosts the chance of success and lowers the risk of side effects.
Strategies for Therapy Selection in Clinical Practice
Choosing the right therapy is a team effort. It involves looking at the tumor, the patient’s health, and other factors. Biomarker-based treatment decisions are becoming more common, helping doctors make better choices.
To make the best decisions, doctors need to keep up with new research and guidelines. They also must consider each patient’s unique situation and preferences.
Side Effects and Quality of Life Impact
When looking at cancer treatment options, it’s key to know about the side effects of immunotherapy for cancer and targeted therapy. Both have changed how we fight cancer. But they also have side effects that can affect a patient’s quality.
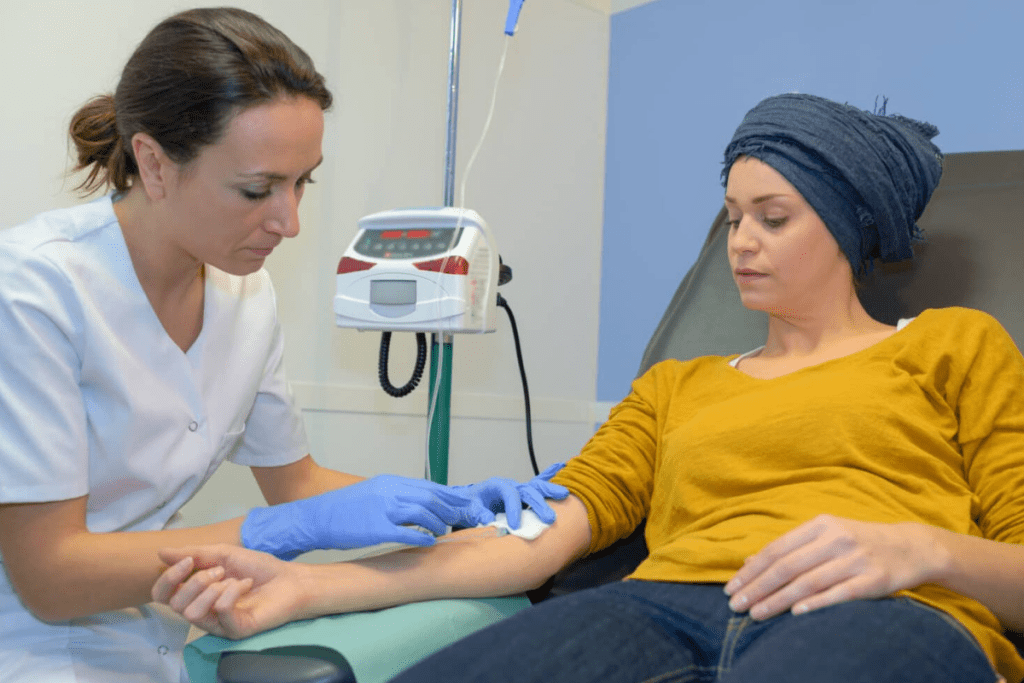
Immune-related Adverse Events
Immunotherapy uses the immune system to fight cancer. But it can cause immune-related adverse events (irAEs). These happen when the immune system attacks healthy tissues. Common irAEs include skin rash, diarrhea, and fatigue.
In severe cases, irAEs can affect the lungs, liver, or endocrine system. Long-term autoimmune complications are a worry with immunotherapy. They can lead to chronic conditions that need ongoing care.
Targeted Therapy Toxicity Profiles
Targeted therapy aims to hit cancer cells without harming normal cells. But it can cause side effects. The type of side effect depends on the drug and its target. Common issues include skin problems, high blood pressure, and stomach issues.
Some targeted therapies can also harm the heart or liver.
Long-term Complications and Management Strategies
Both immunotherapy for cancer and targeted therapy can lead to long-term issues. For immunotherapy, managing chronic irAEs is key. For targeted therapy, watching for late-onset toxicities is important.
Managing these complications involves adjusting doses, using other drugs to lessen side effects, and regular check-ups. This helps catch any problems early.
Patient Quality of Life Considerations
The choice between immunotherapy for cancer and targeted therapy must consider about quality of life. The severity of side effects, how well the treatment works, and the patient’s health and wishes are important. Doctors and patients work together to find the best treatment plan.
Cancer Types and Optimal Treatment Selection
Choosing the right treatment for cancer is key. Different cancers respond better to different therapies. As we learn more about therapies for cancer, picking the best treatment for each cancer type is more important.
Cancers Where Immunotherapy Shows Superior Outcomes
Immunotherapy has changed the game for some cancers, giving patients new hope. Immunotherapy cancer treatment works well for melanoma, lung cancer, and bladder cancer. For tough cancers, it can increase response rates up to 58%.
Melanoma, a skin cancer, has seen big wins with immunotherapy. Treatments like checkpoint inhibitors have greatly improved survival rates for advanced melanoma patients.
Malignancies Best Treated with Targeted Approaches
Targeted therapy is a game-changer for some cancers, thanks to genetic mutations. It works wonders for HER2-positive breast cancer, EGFR-mutated lung cancer, and BRAF-mutated colorectal cancer.
Targeted therapy is precise, reducing harm to healthy cells and side effects. It’s a great choice for cancers with clear targets.
Combination Strategies for Specific Cancer Types
Using both immunotherapy and targeted therapy together is showing promise. For example, mixing these treatments can make them more effective for some cancers.
Researchers are constantly studying these combinations. They aim to find the best mix for each cancer type, aiming to improve patient results.
The Future of Cancer Immunotherapy
Cancer immunotherapy is set to change how we treat cancer. The field is growing fast, with many new ideas showing promise. We’re on the edge of a new era in cancer treatment, thanks to immunotherapy.
Next-Generation Immune Checkpoint Inhibitors
New immune checkpoint inhibitors are being made to work better. These new agents aim to fix the problems of current treatments, like resistance and side effects. Researchers are looking into novel checkpoint molecules beyond PD-1 and CTLA-4.
“The next generation of checkpoint inhibitors is a big step in fighting cancer,” “By targeting new paths and mixing therapies, we might see better results and longer lives.”
Novel Combination Approaches
Researchers are exploring new ways to mix different immunotherapies. They’re also looking at combining immunotherapy with other treatments, like targeted therapy or chemotherapy. These combination approaches aim to make treatments more effective and fight resistance.
- Combining checkpoint inhibitors with other immunotherapies, such as cancer vaccines or CAR-T cell therapy.
- Pairing immunotherapy with targeted therapies to enhance tumor killing and reduce resistance.
- Integrating immunotherapy with conventional treatments like chemotherapy and radiation therapy.
Biomarker Development for Improved Patient Selection
Finding reliable biomarkers is key to knowing who will benefit from immunotherapy. Scientists are working hard to find new biomarkers. This will help doctors make better treatment choices.
Genomic and transcriptomic analyses are helping find these biomarkers. For example, tumor mutational burden (TMB) and microsatellite instability (MSI) are showing promise for predicting how well treatments will work.
Addressing Resistance Mechanisms
Overcoming resistance to immunotherapy is a big challenge. Understanding how resistance happens is vital. Researchers are studying how tumors and the immune system interact to cause resistance.
To fight resistance, scientists are looking at combining therapies, finding new targets, and trying different dosing schedules.
As we keep moving forward in cancer immunotherapy, the future looks bright. With all the research and development happening, we’re likely to see big improvements in cancer treatment soon.
Conclusion: Personalizing Cancer Treatment Decisions
Personalized cancer treatment is key to the best results. Knowing about immunotherapy helps doctors choose the right treatment for each patient.
Immunotherapy has changed cancer treatment, giving hope to many. Seeing how well immunotherapy works helps doctors fine-tune treatment plans.
We’ve looked at the good and bad of immunotherapy and targeted therapy. A personalized approach is vital. It considers each patient’s unique needs and the cancer’s type.
As we learn more about cancer and treatments, making treatment plans just for each patient will continue to be important. This ensures top-notch care for everyone.
FAQ
What is immunotherapy for cancer?
Immunotherapy for cancer uses the body’s immune system to fight cancer. It helps the immune system find and attack cancer cells.
How does immunotherapy work?
Immunotherapy uses different methods to boost the immune system. This includes checkpoint inhibitors, cancer vaccines, and adoptive T-cell therapy. These methods help the immune system fight cancer cells.
What is targeted therapy?
Targeted therapy is a precise way to treat cancer. It focuses on specific cancer cells by targeting genetic mutations or proteins. This helps stop cancer cells from growing and surviving.
What are the major types of immunotherapy approaches?
The main types of immunotherapy are checkpoint inhibitors, cancer vaccines, adoptive T-cell therapy, and cytokines. These methods help the immune system attack cancer cells.
What are the common classes of targeted therapies?
Common targeted therapies include tyrosine kinase inhibitors, monoclonal antibodies, and small-molecule inhibitors. These treatments target specific genetic mutations or proteins in cancer cells.
How do I know if immunotherapy is working?
Signs that immunotherapy is working include smaller tumors, better symptoms, and longer survival. Your doctor will check how you’re doing and adjust your treatment as needed.
What are the side effects of immunotherapy?
Side effects of immunotherapy can include skin rash, diarrhea, and fatigue. Your doctor will watch for these and help you manage them.
Can immunotherapy be used in combination with other treatments?
Yes, immunotherapy can be used with other treatments like chemotherapy and radiation. Combining treatments can improve results and increase response rates.
How is patient selection determined for immunotherapy?
Choosing patients for immunotherapy depends on several factors. These include the type of cancer, specific biomarkers, and the patient’s health. Your doctor will consider these to decide if immunotherapy is right for you.
What is the role of biomarkers in immunotherapy?
Biomarkers are key in predicting how well immunotherapy will work. For example, PD-L1 expression helps identify patients likely to benefit from immunotherapy.
References
Dailah, H. G. (2024). Potential role of immunotherapy and targeted therapy in cancer treatment. Current Oncology Reports, 26(2), 62.