Last Updated on October 20, 2025 by
Cause of Hepatoblastoma is a rare, malignant liver tumor that mainly hits young kids, usually under five. It’s the top liver cancer in kids, affecting about 1.5 children per million each year.
We’re all worried about childhood liver cancer because knowing its causes is key to catching it early. Most cases don’t have a clear cause yet. But scientists are working hard to find out what genetic and developmental factors lead to this serious disease in kids.
Key Takeaways
- Liver cancer in children is extremely rare, with hepatoblastoma being the most common type.
- It mainly affects kids under the age of five.
- Understanding the causes and risk factors is key for early detection and treatment.
- Research is ongoing to find genetic and developmental risk factors.
- Early detection greatly improves the chances of survival for kids with hepatoblastoma.
Understanding Hepatoblastoma: A Rare Pediatric Liver Cancer
Hepatoblastoma is a rare liver cancer that mainly hits infants and young kids. It’s key to know what it is, how it shows up, and its impact on young people.
Definition and Clinical Presentation
Hepatoblastoma is a liver tumor that mostly shows up in kids under 3. Symptoms include belly pain, a big mass in the right upper belly, and unexpected weight loss. It can also cause loss of appetite and tiredness.
Early detection is key for better treatment and survival chances. The exact reasons for hepatoblastoma are not fully known. But, being very underweight at birth is a known risk factor.

Incidence and Age Distribution
Hepatoblastoma is a very rare cancer, making up about 1% of all childhood cancers. It’s the most common liver cancer in kids. It’s most common in kids under 18 months, with most cases found in the first two years.
Thanks to better treatments and early detection, survival rates have gone up. We keep watching and studying this disease to help kids live better lives.
Genetic Predisposition as a Primary Cause
Genetic predisposition is key in the development of hepatoblastoma, a rare liver cancer in children. Certain genetic syndromes and chromosomal abnormalities are major risk factors for this disease.
Hereditary Factors
Hereditary factors greatly increase the risk of hepatoblastoma. Familial adenomatous polyposis (FAP) and Beckwith-Wiedemann syndrome are two genetic conditions that raise this risk. Children with these syndromes get regular screenings for hepatoblastoma, helping catch it early.
Other hereditary conditions, like hemihyperplasia and Simpson-Golabi-Behmel syndrome, also raise the risk of hepatoblastoma. These conditions highlight the need for genetic counseling and monitoring in families with such histories.
Chromosomal Abnormalities
Chromosomal abnormalities, such as trisomy 18, are linked to a higher risk of hepatoblastoma. Extra or missing genetic material can disrupt normal cell function, leading to cancerous growth.
- Trisomy 18 is a known risk factor for hepatoblastoma.
- Other chromosomal abnormalities may also contribute to the development of this cancer.
- Genetic testing can help identify individuals at higher risk.
As research digs deeper into the genetics of hepatoblastoma, the role of genetic predisposition becomes clearer. Understanding these factors helps in creating targeted screening programs and preventive measures for high-risk groups.

Recent studies show that children with certain genetic syndromes may benefit from regular hepatoblastoma screenings. This proactive approach can lead to earlier detection and more effective treatments.
“The identification of genetic risk factors for hepatoblastoma has significant implications for clinical practice, enabling targeted surveillance and potentially improving outcomes for children at highest risk.”
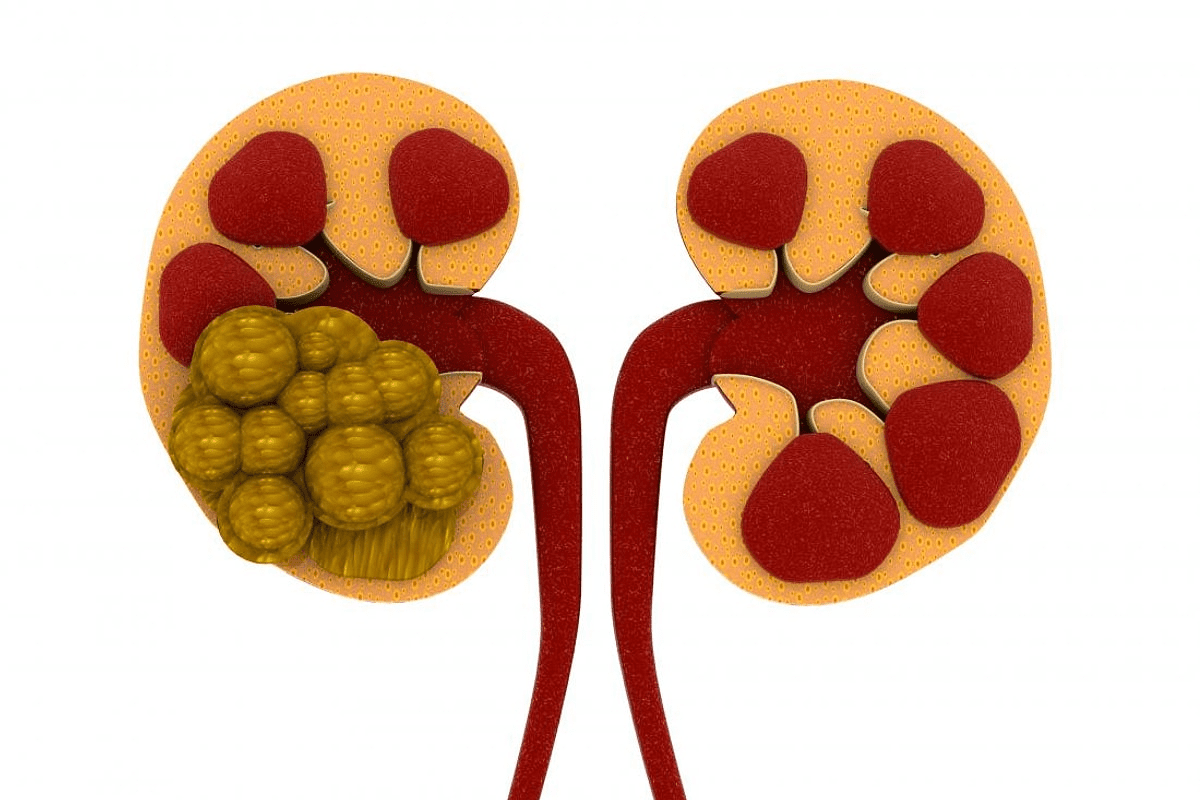
Recent Study on Hepatoblastoma
Known Risk Factors for Hepatoblastoma
Several risk factors increase the chance of getting hepatoblastoma in kids. Knowing these factors helps find and treat this rare liver cancer early.
Very Low Birth Weight
Children born very light, under 1,000 grams, face a higher risk of hepatoblastoma. Very low birth weight is a big risk that needs careful watching.
A study in a top medical journal linked very low birth weight to more cases of hepatoblastoma. We must think about this risk when looking at a child’s overall risk.
Premature Birth
Premature birth, often with very low birth weight, also raises the risk of hepatoblastoma. Premature babies face many health problems, including a higher chance of this rare cancer.
- Premature birth can cause many health issues.
- Very low birth weight is a big risk for hepatoblastoma.
- It’s important to watch premature babies with very low birth weight closely.
Parental Age and Family History
Older parental age and a family history of certain genetic disorders or cancers also raise the risk. We should look at these factors when checking a child’s risk.
- Older parents may increase the risk.
- A family history of genetic disorders can play a role.
- Genetic counseling might help families with such histories.

Understanding these risk factors helps us spot kids at higher risk. While we can’t prevent all cases, knowing these factors leads to early detection and better treatment.
Genetic Syndromes Linked to Hepatoblastoma Development
Research has found certain genetic syndromes linked to a higher risk of hepatoblastoma. Kids with these conditions are more likely to get this rare liver cancer. Knowing these genetic risks is key for early detection and treatment of hepatoblastoma.

Beckwith-Wiedemann Syndrome
Beckwith-Wiedemann syndrome is a genetic disorder that raises the risk of tumors, including hepatoblastoma. It’s marked by overgrowth and a higher chance of childhood cancer. Kids with this syndrome need regular checks for hepatoblastoma and other tumors.
Familial Adenomatous Polyposis
Familial adenomatous polyposis (FAP) is a genetic condition linked to a higher risk of hepatoblastoma. FAP causes many polyps in the colon, leading to colorectal cancer if not treated. The link between FAP and hepatoblastoma shows the need for genetic screening and watchful waiting in FAP families.
Trisomy 18 and Other Chromosomal Disorders
Trisomy 18, or Edwards syndrome, is a chromosomal disorder linked to a higher risk of hepatoblastoma. Other chromosomal issues may also lead to this liver cancer. Kids with these conditions need close monitoring and follow-up care to catch any signs of hepatoblastoma.
The discovery of genetic syndromes linked to hepatoblastoma highlights the role of genetic testing and surveillance. By understanding these genetic factors, doctors can offer targeted screening and early intervention. This could help improve the outlook for kids at risk of hepatoblastoma.
Molecular Mechanisms Behind Hepatoblastoma
Understanding hepatoblastoma’s molecular roots is key to finding better treatments. Recent studies show how disruptions in growth-regulation pathways play a big role. Other molecular mechanisms also contribute to the disease.
Disruptions in Growth-Regulation Pathways
Hepatoblastoma develops due to problems in pathways that control growth and development. Genetic mutations in these pathways cause cells to grow out of control, a sign of cancer. The Wnt/β-Catenin signaling pathway is often affected in this disease.
Wnt/β-Catenin Signaling Abnormalities
The Wnt/β-Catenin pathway is vital for cell growth and fate. Abnormalities in this pathway, often from CTNNB1 gene mutations, are common in hepatoblastoma. These issues cause β-Catenin to build up, leading to genes that help cells grow and survive being turned on.
Immune System Involvement
The immune system has a complex role in hepatoblastoma. It can fight cancer cells but tumors can hide from it. Knowing how the immune system and hepatoblastoma interact is key for new treatments.
Studying hepatoblastoma’s molecular roots helps us understand the disease better. It also guides the creation of targeted treatments. By focusing on specific genetic and molecular changes, we can make treatments more effective. This could lead to better survival rates for patients with hepatoblastoma.
Environmental and Prenatal Factors Under Investigation
The exact cause of hepatoblastoma is not yet known. Researchers are looking into environmental and prenatal factors. They are trying to find out what causes this rare liver cancer in kids.
Maternal Exposures During Pregnancy
Some studies link maternal exposure to toxins during pregnancy with hepatoblastoma in children. Exposure to harmful substances like pesticides and heavy metals is being studied. These might increase the risk of this cancer.
Research shows that tobacco smoke and chemicals in the workplace may also be linked. But, more research is needed to understand these connections better.
Perinatal Influences
Very low birth weight and premature birth are linked to a higher risk of hepatoblastoma. These factors might cause the disease through genetic and epigenetic changes.
The role of parental age at conception is also being looked into. Some studies suggest a link between older parents and a higher risk of the disease.
Research Limitations in Identifying Environmental Causes
Finding environmental causes of hepatoblastoma is hard. The disease is rare, and studying environmental exposures is complex. This makes it tough to do definitive studies.
The multifactorial nature of hepatoblastoma makes it hard to pinpoint specific environmental risks. Current research often has small sample sizes and relies on past data.
As we keep looking into hepatoblastoma, understanding environmental and prenatal factors is key. This will help us learn more about this disease.
Sporadic Cases of Hepatoblastoma: The Mystery Remains
Most cases of hepatoblastoma happen without a known cause. This makes it hard for doctors and scientists to find and treat this rare liver cancer in kids.
Idiopathic Cases Without Identifiable Cause
Many times, hepatoblastoma appears without any known genetic or environmental factors. These cases are hard to understand because they don’t fit into any clear patterns. Scientists are looking into new ways to study these cases, like advanced genetic tests and environmental studies.
A recent study, found in this research paper, shows growing interest in the molecular causes of sporadic hepatoblastoma. It points out how complex the disease is and how much more research is needed.
Current Research Directions
Researchers are looking into how maternal exposures and environmental toxins might play a role. They’re also studying the genetics of sporadic cases to find possible mutations. New imaging techniques, like hepatoblastoma radiology, help them understand the disease better.
Studies are also looking at the link between very low birth weight and premature birth and hepatoblastoma. While these factors increase risk, they don’t explain all cases. So, the search for more risk factors goes on.
Challenges in Determining Causation
Finding the cause of sporadic hepatoblastoma is tough. The disease is rare, making big studies hard. The possible causes are complex and hard to pin down. But, scientists keep working to find the causes to help diagnose and treat the disease better.
In summary, while we’ve made progress in understanding hepatoblastoma, the sporadic cases are a big mystery. More research is needed to find out why this rare and complex disease happens.
Conclusion: Progress in Understanding and Treating Hepatoblastoma
There have been big steps forward in treating hepatoblastoma, a rare liver cancer in kids. Now, more than 80% of kids with localized disease can survive. This is thanks to new treatments.
Doctors use surgery, chemotherapy, and liver transplants to help kids. Finding out why liver cancer happens in kids is key to better treatments. This research is ongoing.
We must keep talking about liver cancer in kids and support families. This way, we can help kids with hepatoblastoma live better lives. It’s all about improving their quality of life.
FAQ
What is hepatoblastoma?
Hepatoblastoma is a rare liver tumor that mainly affects kids under five. It’s the most common liver cancer in children.
What are the common symptoms of hepatoblastoma?
Symptoms include swelling in the belly, loss of appetite, and weight loss. Kids might also feel tired and have belly pain.
What are the known risk factors for developing hepatoblastoma?
Risk factors include being very underweight at birth, premature birth, and certain genetic syndromes. These include Beckwith-Wiedemann syndrome and familial adenomatous polyposis.
How does genetic predisposition contribute to hepatoblastoma?
Genetics play a big role in hepatoblastoma. Certain genetic syndromes and chromosomal issues can raise the risk of getting the disease.
What is the role of the Wnt/β-Catenin signaling pathway in hepatoblastoma?
The Wnt/β-Catenin pathway is often broken in hepatoblastoma. This helps the disease grow and spread.
Are there any environmental factors that contribute to hepatoblastoma?
Some studies hint at environmental and prenatal factors. But more research is needed to confirm these risks.
What is the prognosis for children diagnosed with hepatoblastoma?
Thanks to better treatments, the outlook for kids with hepatoblastoma has gotten better. Survival chances depend on the disease’s stage and spread.
How is hepatoblastoma treated?
Treatment includes surgery, chemotherapy, and sometimes liver transplant. It depends on the disease’s extent and stage.
What is the importance of early detection in hepatoblastoma?
Catching it early is key to better treatment and survival chances. Regular checks and screenings are vital for at-risk kids.
References
- National Cancer Institute. (2025). Hepatoblastoma Treatment (PDQ ®)”Patient Version. National Cancer Institute. https://www.cancer.gov/types/liver/patient/hepatoblastoma-treatment-pdq
- American Cancer Society. (2024). Childhood Liver Cancer. American Cancer Society. https://www.cancer.org/cancer/types/childhood-liver-cancer.html
- U.S. National Library of Medicine. (2023). Hepatoblastoma. MedlinePlus. https://medlineplus.gov/ency/article/001354.htm