Last Updated on December 3, 2025 by Bilal Hasdemir

Cerebrovascular disease significantly contributes to global illness and mortality. Ischemic stroke happens when a blood clot blocks blood flow to the brain blood clot in brain.
The first line treatment for ischemic stroke is using thrombolytic agents like alteplase and tenecteplase. These drugs break down the clot, allowing blood to flow again to the brain. It’s very important to start this treatment quickly to help the patient.
Key Takeaways
- Cerebrovascular disease includes conditions like ischemic and hemorrhagic strokes.
- The first line treatment for ischemic stroke involves thrombolytic therapy.
- Alteplase and tenecteplase are commonly used thrombolytic agents.
- Timely administration of thrombolytic agents improves patient outcomes.
- CVA is the medical abbreviation for cerebrovascular accident.
Cerebrovascular disease significantly contributes to global illness and mortality.
It’s important to understand cerebrovascular disease to tackle its big impact on health. This disease affects the blood vessels that supply the brain. It leads to serious problems, like stroke.
Definition and Pathophysiology
Cerebrovascular disease significantly contributes to global illness and mortality. brain. This can cause less blood flow or even a rupture. The disease is complex, involving many factors like blood vessels, inflammation, and cells.
Stroke is a big part of this disease. It can be ischemic or hemorrhagic, with ischemic being more common. The health stroke scale helps measure how severe a stroke is.
Knowing how the disease works helps doctors find better treatments. This includes using tPA (tissue plasminogen activator) for some strokes.
CVA Medical Abbreviation Explained
The term CVA stands for cerebrovascular accident, or stroke. It happens when the brain doesn’t get enough blood. This can cause brain damage. CVAs are divided into ischemic and hemorrhagic types, each needing different treatments.
“The timely recognition of stroke symptoms and appropriate medical intervention are critical in minimizing brain damage and improving patient outcomes.”
Prevalence and Impact in the United States
Cerebrovascular disease significantly contributes to global illness and mortality.
| Year | Stroke Incidence | Mortality Rate |
| 2019 | 795,000 | 37.9 per 100,000 |
| 2020 | 808,000 | 38.8 per 100,000 |
| 2021 | 823,000 | 39.2 per 100,000 |
The high number of strokes in the US shows we need to keep working on prevention and treatment. Early detection and effective care are key.
Types of Cerebrovascular Diseases
Cerebrovascular disease significantly contributes to global illness and mortality. to different strokes. These conditions are a big cause of illness and death worldwide.
Knowing the types of cerebrovascular diseases helps us understand them better. This knowledge guides how we treat them. The main types are ischemic stroke, hemorrhagic stroke, transient ischemic attack (TIA), and cerebrovascular ischemia.
Ischemic Stroke and Cerebral Infarction
Ischemic stroke happens when a brain blood vessel gets blocked. This cuts off blood flow to a brain area. The brain tissue then gets damaged because it lacks oxygen and nutrients. Ischemic strokes make up about 87% of all strokes.
The blockage is usually caused by a clot. Thrombotic strokes are clots that form in the brain. Embolic strokes are clots that travel to the brain from elsewhere in the body.
Hemorrhagic Stroke
Hemorrhagic stroke happens when a brain blood vessel bursts. This causes bleeding in or around the brain. It’s less common than ischemic stroke but can be more severe. Hemorrhagic strokes are divided into intracerebral hemorrhage and subarachnoid hemorrhage.
Intracerebral hemorrhage is bleeding directly into the brain. Subarachnoid hemorrhage is bleeding into the space around the brain.
Transient Ischemic Attack (TIA)
A transient ischemic attack, or “mini-stroke,” is a short episode of brain ischemia without lasting damage. TIAs have symptoms like a stroke but go away within 24 hours, usually sooner.
TIAs are a sign that a stroke might happen. They need urgent medical attention. Quick action can stop a full stroke from happening.
Cerebrovascular Ischemia
Cerebrovascular ischemia means less blood flow to the brain, which can damage tissue. It can affect the whole brain or just a part of it.
The damage from ischemia depends on how long and how severe it is. Understanding this is key to finding good treatments.
Risk Factors for Cerebrovascular Disease
Cerebrovascular disease can be caused by many factors. Some can be changed, while others cannot. Knowing these factors helps us prevent and manage the disease better.
Modifiable Risk Factors
Modifiable risk factors are things we can change. They include lifestyle choices and medical conditions. Changing these can lower the risk of cerebrovascular disease. Key factors include:
- Hypertension: High blood pressure can harm brain blood vessels, leading to stroke.
- Diabetes Mellitus: Diabetes can damage blood vessels and nerves, increasing disease risk.
- Hyperlipidemia: High cholesterol and triglycerides can cause artery blockages, raising stroke risk.
- Smoking: Smoking harms the heart and blood vessels, increasing disease risk.
- Obesity and Physical Inactivity: Being overweight or inactive can lead to conditions that increase disease risk.
Non-Modifiable Risk Factors
Non-modifiable risk factors are things we can’t change. But knowing them helps us understand who’s at higher risk. These include:
- Age: Risk increases with age, after 55.
- Family History: A family history of stroke or cerebrovascular disease raises risk.
- Genetic Predisposition: Some genetic conditions increase disease risk.
- Gender: Men are generally at higher risk, but women’s risk increases after menopause.
Cardiovascular Connections
Heart and blood vessel health are linked to cerebrovascular disease. Heart conditions can affect brain blood supply. For example, atrial fibrillation can cause blood clots leading to stroke. So, managing heart health is key to preventing cerebrovascular disease.
Recognizing Stroke Symptoms
Knowing the signs of a stroke is key for quick action. Spotting stroke symptoms early can greatly help patients by getting them to the hospital fast.
BE-FAST Acronym for Stroke Detection
The BE-FAST acronym helps remember stroke symptoms. It stands for Balance, Eyes, Face, Arm, Speech, and Time. It’s a quick way to spot a stroke and call for help.
BE-FAST covers many symptoms, like balance problems and speech issues. It also reminds us of the need for fast medical help.
Left-Sided vs. Right-Sided Stroke Symptoms
Strokes on the left side of the brain often cause speech problems. Strokes on the right side can lead to spatial issues and neglect of the left side of the body.
Knowing these differences helps doctors treat strokes better. They need to understand these variations to give the right care.
Frontal Lobe CVA Symptoms
A stroke in the frontal lobe can cause many problems. These include changes in personality and motor weakness on the opposite side of the body.
It can also affect speech and language if the dominant side is hit. Spotting these symptoms is important for effective treatment.
How to Tell If Someone Has Had a Stroke
To see if someone has had a stroke, look for BE-FAST signs. Check for balance issues, vision problems, and weakness. Also, watch for speech troubles and note when symptoms started.
If you think someone has had a stroke, call for help FAST. Quick medical care is vital for better outcomes.
Diagnostic Procedures for Cerebrovascular Disease
Diagnosing cerebrovascular disease requires several steps. These steps help find out the type, how severe it is, and where it is. This information is key for deciding how to treat it.
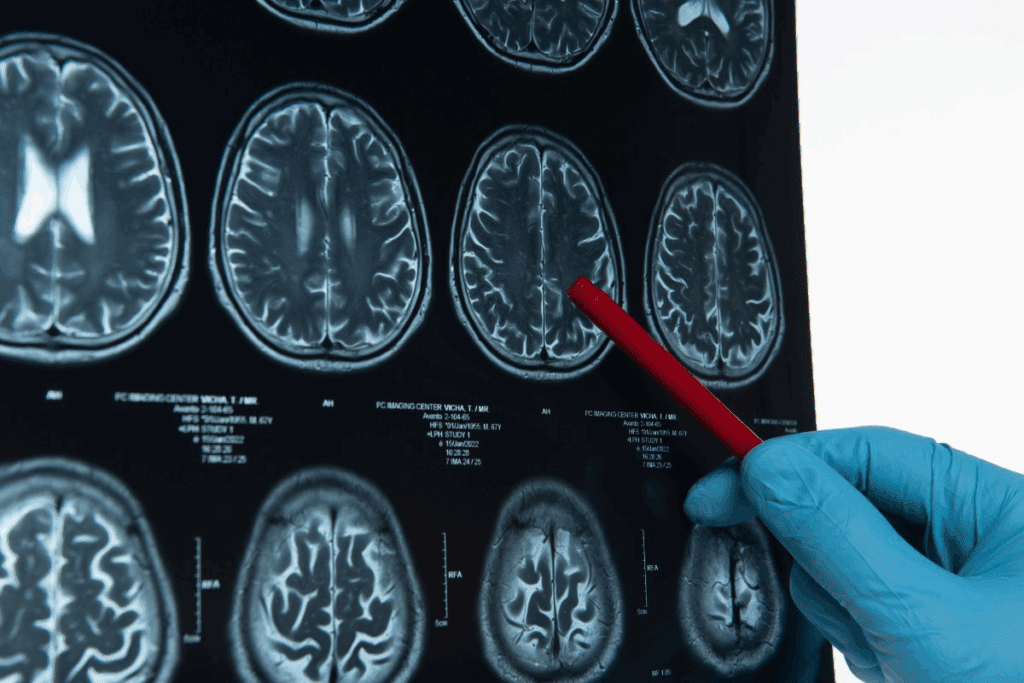
Imaging Techniques
Imaging is a big part of diagnosing cerebrovascular disease. CT scans and MRI scans are used to see the brain and its blood vessels. CT scans are fast and good for emergencies because they can spot bleeding right away.
MRI scans give detailed pictures of the brain. They help find areas where blood flow is low.
Other imaging methods include:
- CT angiography to see the blood vessels and find blockages.
- MR angiography for detailed blood vessel images without contrast.
- Carotid ultrasound to check blood flow in the carotid arteries.
Clinical Assessment Tools
Clinical tools add to imaging by checking how well a patient’s brain is working. The National Institutes of Health Stroke Scale (NIHSS) helps doctors see how bad a stroke is. It looks at things like how awake someone is, their vision, speech, and how well they can move.
Other tools include:
- The Modified Rankin Scale (mRS) to see how much someone can do on their own.
- The Barthel Index to check how well someone can do daily tasks.
By using both imaging and clinical tools, doctors can accurately diagnose cerebrovascular disease. They can then create a good treatment plan for patients.
Emergency First-Line Treatments for Ischemic Stroke
Emergency treatments for ischemic stroke have greatly improved. These treatments include using thrombolytic agents.
Tissue Plasminogen Activator (tPA) Administration
Tissue Plasminogen Activator (tPA) is a key treatment for acute ischemic stroke. Alteplase, a type of tPA, has been shown to improve outcomes when given quickly.
- Alteplase dissolves the blood clot causing the stroke.
- Its effectiveness depends on how quickly it is given.
Alteplase: Mechanism and Dosing
Alteplase is given through an IV, with the dose based on the patient’s weight. The standard dose is 0.9 mg/kg, with a maximum of 90 mg.
- The first 10% of the dose is given as a bolus over 1 minute.
- The rest is infused over 60 minutes.
Tenecteplase as an Alternative Treatment
Tenecteplase is another thrombolytic agent being studied as an alteplase alternative. It has a simpler dosing regimen and may offer better outcomes for some patients.
- Tenecteplase is given as a single bolus dose.
- It is being considered more for stroke treatment.
TPA Time Windows and Protocols
The time window for tPA administration is key. Guidelines suggest treatment within 4.5 hours of stroke onset. Timely intervention is vital for the best results.
| Time Window | Treatment Eligibility |
| 0-3 hours | Eligible for tPA treatment |
| 3-4.5 hours | Eligible with careful patient selection |
Understanding Blood Clot in Brain Treatment
Treating blood clots in the brain requires knowing how clots form and dissolve. Blood clots in the brain, or cerebral thrombosis, block blood flow. This is a serious emergency that needs quick action.
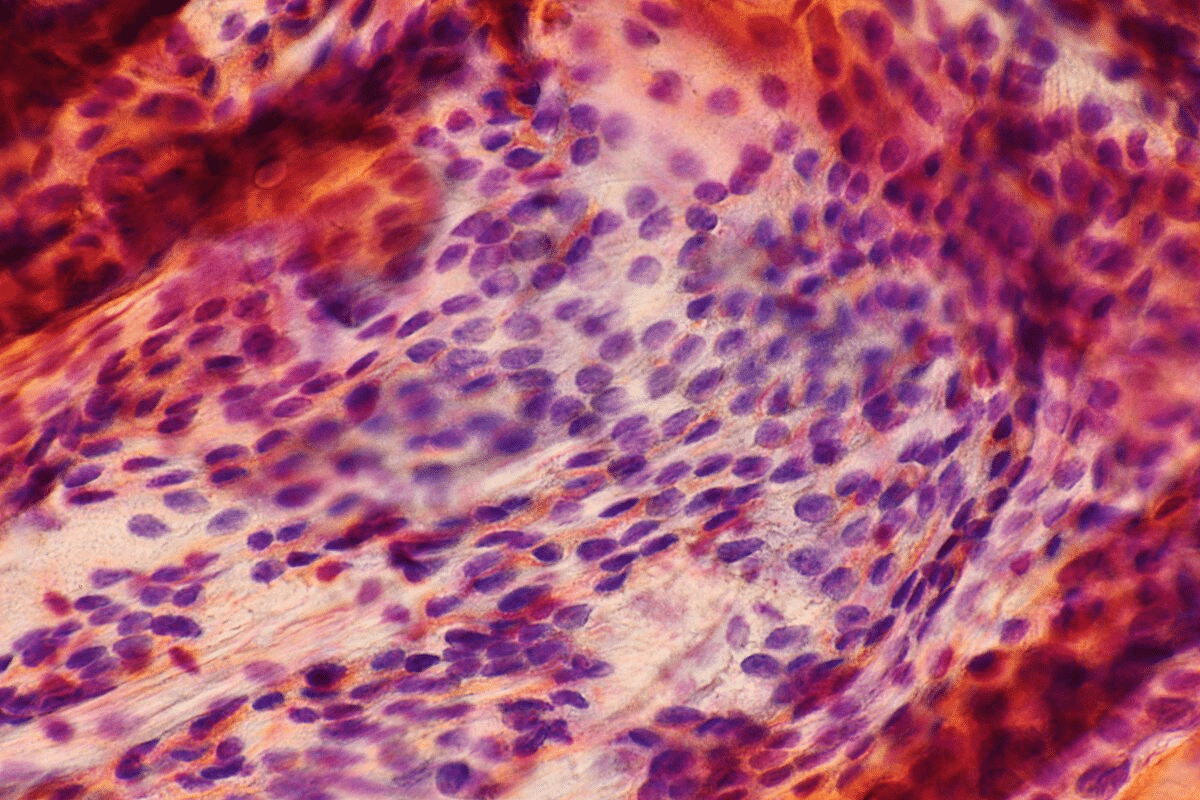
Mechanism of Clot Formation in Cerebral Vessels
Clots in brain vessels form through complex processes. Changes in blood flow, vessel injury, and blood composition play roles. Understanding these is key to effective treatments.
Several factors can trigger clot formation in the brain, including:
- Atherosclerosis, or the buildup of plaque in the arteries
- Cardiac conditions, such as atrial fibrillation
- Blood disorders that increase clotting tendency
Clot-Busting Medications and Their Efficacy
Clot-busting drugs, or thrombolytics, are vital for treating acute ischemic stroke. Alteplase, a tPA, dissolves clots and restores blood flow. It’s a cornerstone in treatment.
The success of these drugs depends on several factors. Time from stroke onset and patient health are critical. Using alteplase within a 4.5-hour window can greatly improve outcomes.
Surgical Interventions for Persistent Clots
When drugs fail, surgery may be needed. Mechanical thrombectomy removes the clot from the vessel. It’s highly effective in certain cases, improving outcomes significantly.
Treatment Outcomes and Prognosis
Treatment results vary based on several factors. These include treatment timing, clot size and location, and patient health. Quick treatment with drugs or surgery can greatly improve survival and reduce disability risk.
A leading neurologist notes, “The key to treating blood clots in the brain is quick diagnosis and action. Using the latest in thrombolytic therapy and mechanical thrombectomy is essential.” This shows the need for a complete treatment plan.
“Time is brain” is a mantra in stroke treatment, highlighting the critical need for swift action in treating cerebral blood clots.
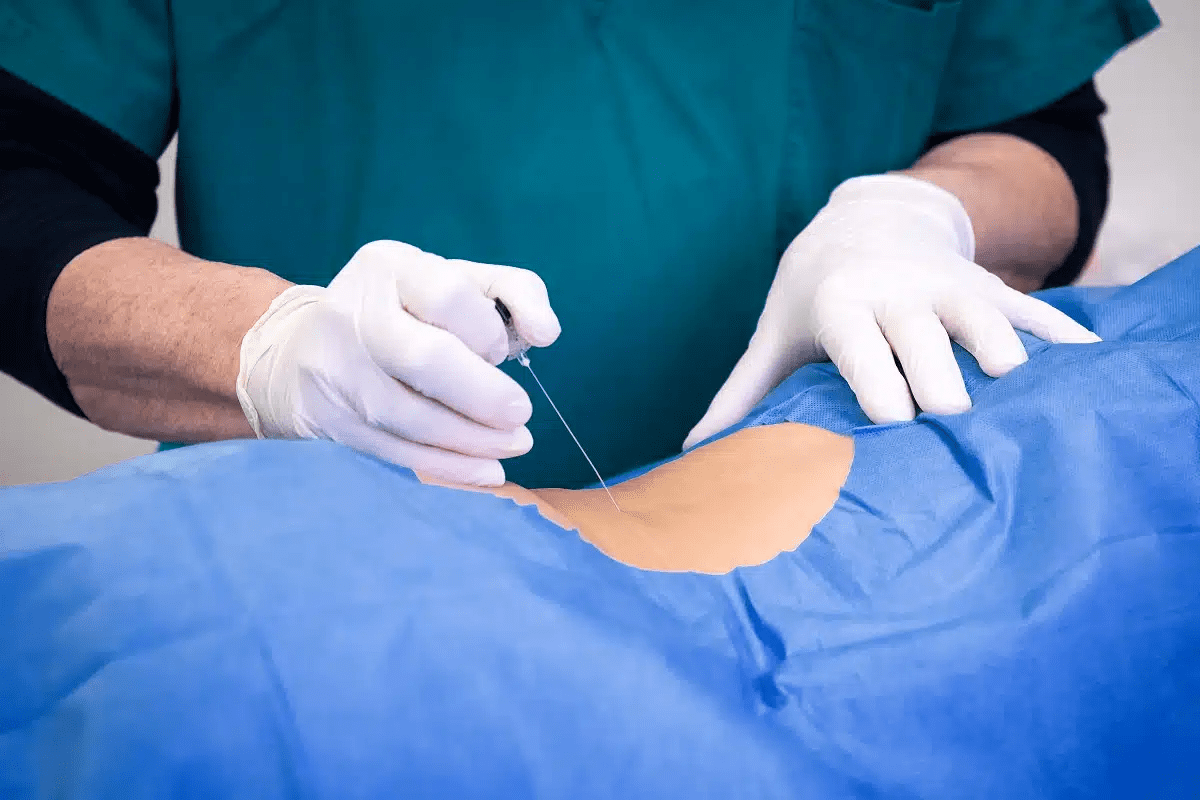
Mechanical Thrombectomy Procedures
Mechanical thrombectomy is a complex medical procedure. It aims to remove blood clots from the brain. This is key in treating acute ischemic stroke, helping patients by bringing blood back to the brain.
Candidate Selection Criteria
Choosing the right patients for mechanical thrombectomy is vital. The decision is based on how long ago the stroke happened, the clot’s size and location, and the patient’s health.
- Time elapsed: The sooner, the better.
- Clot size and location: Larger clots in main arteries are targeted.
- Patient’s health: Age, other health issues, and starting health level are considered.
Procedure Details and Techniques
The procedure uses a catheter to reach the clot. A device is then used to remove or break down the clot.
| Technique | Description | Advantages |
| Stent Retriever | A stent is deployed to engage the clot, then retrieved. | High success rate, effective for large vessel occlusions. |
| Aspiration Thrombectomy | A catheter is used to aspirate the clot directly. | Quick procedure, effective for certain clot types. |
Outcomes and Success Rates
The success of mechanical thrombectomy is seen in how well the clot is removed. It’s also measured by how well the patient does afterward, like less disability and death.
“Mechanical thrombectomy has revolutionized the treatment of acute ischemic stroke, significantly improving patient outcomes when used appropriately.” –
AHA/ASA Guidelines
Complications and Risks
While safe, mechanical thrombectomy has risks. These include problems with blood vessels, bleeding, and issues with the procedure itself.
- Vascular complications: Dissection or perforation of vessels.
- Hemorrhage: Symptomatic intracranial hemorrhage is a serious risk.
- Procedural difficulties: Challenges in navigating the catheter or deploying the device.
It’s important for doctors to understand these points. Patients should also know the possible benefits and risks.
First-Line Treatments for Hemorrhagic Stroke
The first step in treating hemorrhagic stroke is a mix of medical care and surgery. These methods help control bleeding and manage blood pressure.
Medical Management Strategies
Medical care for hemorrhagic stroke aims to keep the patient stable. It controls blood pressure and prevents more problems. Doctors use medicines to manage blood pressure, stop seizures, and lower brain pressure.
Key medical management strategies include:
- Managing blood pressure to prevent further bleeding
- Administering anticonvulsants to prevent seizures
- Using medications to reduce intracranial pressure
Surgical Interventions for Bleeding Control
Surgery is often needed to stop bleeding and remove blood clots. This helps relieve brain pressure. Surgical options include craniotomy, clipping, or coiling.
Surgical interventions can significantly improve outcomes by:
- Reducing intracranial pressure
- Preventing further bleeding
- Improving survival rates
Controlling Blood Pressure in Acute Phase
Keeping blood pressure in check is key in the early stages of hemorrhagic stroke. This helps prevent more bleeding. Doctors use special medicines to manage blood pressure.
| Strategy | Description | Benefits |
| Managing Blood Pressure | Using antihypertensive medications to control blood pressure | Reduces risk of further bleeding |
| Monitoring | Continuous monitoring of blood pressure and neurological status | Allows for prompt adjustments in treatment |
Care Plan for Hemorrhagic Stroke
A good care plan for hemorrhagic stroke covers acute care, rehab, and long-term management. It meets the patient’s physical, cognitive, and emotional needs.
Components of a care plan may include:
- Acute care management in a stroke unit
- Rehabilitation therapy to regain lost functions
- Long-term management of risk factors and secondary prevention
Preventive Medications and Therapies
Preventive medications and therapies are key to lowering stroke risk. They target various risk factors for cerebrovascular disease.
Antiplatelet Medications
Antiplatelet drugs like aspirin and clopidogrel prevent platelet clumping. This is good for those who’ve had an ischemic stroke or TIA.
Aspirin is often the first choice because it stops platelets from activating. But, the right drug depends on the patient’s health and how they react to different medicines.
Anticoagulants for Stroke Prevention
Anticoagulants like warfarin, dabigatran, rivaroxaban, and apixaban prevent strokes in people with atrial fibrillation. They stop the coagulation process, reducing clot risk.
Choosing an anticoagulant depends on the patient’s kidney function, bleeding risk, and drug interactions.
Statins and Other Preventive Drugs
Statins lower cholesterol and have anti-inflammatory effects, helping prevent strokes. They reduce LDL cholesterol, slowing atherosclerosis.
Other drugs, like blood pressure medications, are also used to prevent strokes. High blood pressure is a major stroke risk factor.
Plaque Removal Strategies
Plaque removal strategies aim to clear atherosclerotic plaque from blood vessels. Carotid endarterectomy removes plaque from the carotid arteries, improving brain blood flow.
Carotid artery stenting involves placing a stent to keep the artery open. The choice between these depends on the patient’s health, plaque extent, and other factors.
Emerging Treatments and Research
New research is bringing hope for better treatments for cerebrovascular disease. This field is growing fast, with many promising areas to explore.
Neuroprotective Agents in Development
Neuroprotective agents are being made to protect the brain after a cerebrovascular event. They aim to lessen the impact of stroke and help patients recover better. Some key strategies include:
- Antioxidants: To fight oxidative stress
- Anti-inflammatory agents: To lower inflammation
- Agents promoting neural recovery: To boost brain flexibility
Stem Cell Therapy for Cerebrovascular Repair
Stem cell therapy is a new hope for treating cerebrovascular disease. It could repair or replace damaged brain areas. Ongoing research focuses on:
- Ensuring stem cell therapies are safe and effective
- Finding the best ways to deliver stem cells to damaged areas
- Improving stem cell survival and integration
Extended Treatment Windows Research
Traditionally, stroke treatments have had short time windows. But research aims to extend these, helping more patients. This includes:
- Using advanced imaging to check patient eligibility later
- Creating treatments that work even when given later
Cerebrovascular Perfusion Enhancement Techniques
Boosting blood flow to the brain is key in treating cerebrovascular disease. New methods to improve blood flow are being explored, such as:
- Vasodilators: To widen blood vessels and improve flow
- Angioplasty and stenting: To mechanically widen blood vessels
- Novel pharmacological agents: To increase cerebral blood flow
These new treatments and research areas offer great hope for better managing cerebrovascular disease. As research advances, we can expect more innovative therapies, improving patient outcomes.
Conclusion
Cerebrovascular disease significantly contributes to global illness and mortality.ckness and death. We need good stroke treatment and prevention plans.
Managing this disease well is key. We must diagnose and treat patients quickly and effectively. Knowing the different types and risks helps us target our efforts better.
New ways to help people recover from strokes have made a big difference. Tools like the stroke test help catch problems early. This is very important.
Stroke support groups also play a big role. They offer emotional support and help to patients and their families. This shows we need to tackle cerebrovascular disease in many ways.
FAQ
What is cerebrovascular disease?
Cerebrovascular disease affects the blood vessels that supply the brain. It includes ischemic and hemorrhagic strokes.
What is the first line treatment for ischemic stroke?
For ischemic stroke, the first treatment is thrombolytic therapy. This includes drugs like alteplase or tenecteplase.
What is the CVA medical abbreviation?
CVA stands for cerebrovascular accident or stroke.
What are the symptoms of a stroke?
Stroke symptoms can be remembered with the BE-FAST acronym. It covers balance, eyes, face, arm, speech, and time.
What is the difference between ischemic and hemorrhagic stroke?
Ischemic stroke happens when a blood vessel is blocked. Hemorrhagic stroke occurs when a blood vessel ruptures.
What are the risk factors for cerebrovascular disease?
Risk factors include hypertension and diabetes. Non-modifiable factors are age and family history.
Cerebrovascular disease significantly contributes to global illness and mortality.
Diagnosis uses imaging like CT and MRI scans. It also involves the National Institutes of Health Stroke Scale (NIHSS).
What is the role of tPA in stroke treatment?
tPA is a clot-dissolving agent. It’s used to treat acute ischemic stroke and improve outcomes.
What is mechanical thrombectomy?
Mechanical thrombectomy removes brain clots. It’s often used with thrombolytic therapy.
How can stroke be prevented?
Preventive steps include medications like antiplatelets and statins. Lifestyle changes and managing risk factors also help.
What are the emerging treatments for cerebrovascular disease?
New treatments include neuroprotective agents and stem cell therapy. They aim to improve outcomes for cerebrovascular disease.
References
The Lancet. Thrombolysis for Acute Ischemic Stroke Treatment. Retrieved from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31037-4/fulltext