Last Updated on December 3, 2025 by Bilal Hasdemir

Every year, thousands of people face a medical emergency called a stroke. This is often due to a blocked artery in the brain. We aim to help you spot the warning signs.
A stroke can cause serious harm, like brain damage or even death. Recognizing symptoms early is crucial for effective treatment. Sudden numbness or weakness in the face or limbs, usually on one side, is a key sign. You might notice sudden numbness in your face or arm weakness signs that are quite alarming.
Other signs include leg paralysis or trouble speaking. Quick medical assistance is critical in these situations.
The definition of CVA medical event often involves a blocked artery. Learn the critical symptoms you must know. Get the facts fast.
Key Takeaways
- Recognize the warning signs of a stroke, such as sudden numbness or weakness.
- Understand that a blocked artery can lead to severe brain damage.
- Timely medical attention is crucial in treating a stroke.
- Be aware of symptoms like arm weakness, speech difficulty, and leg paralysis.
- Seek immediate help if you or someone else experiences these signs.
Understanding Cerebral Artery Blockages
Before exploring symptoms, it’s important to understand the definition of CVA medical, which stands for Cerebrovascular Accident. A CVA occurs when blood flow to a part of the brain is interrupted, either by a blockage or bleeding. In most cases, this blockage prevents oxygen and nutrients from reaching brain tissue, causing damage or death to brain cells.
Quick medical assistance is critical in these situations.
What Happens When a Brain Artery Becomes Blocked
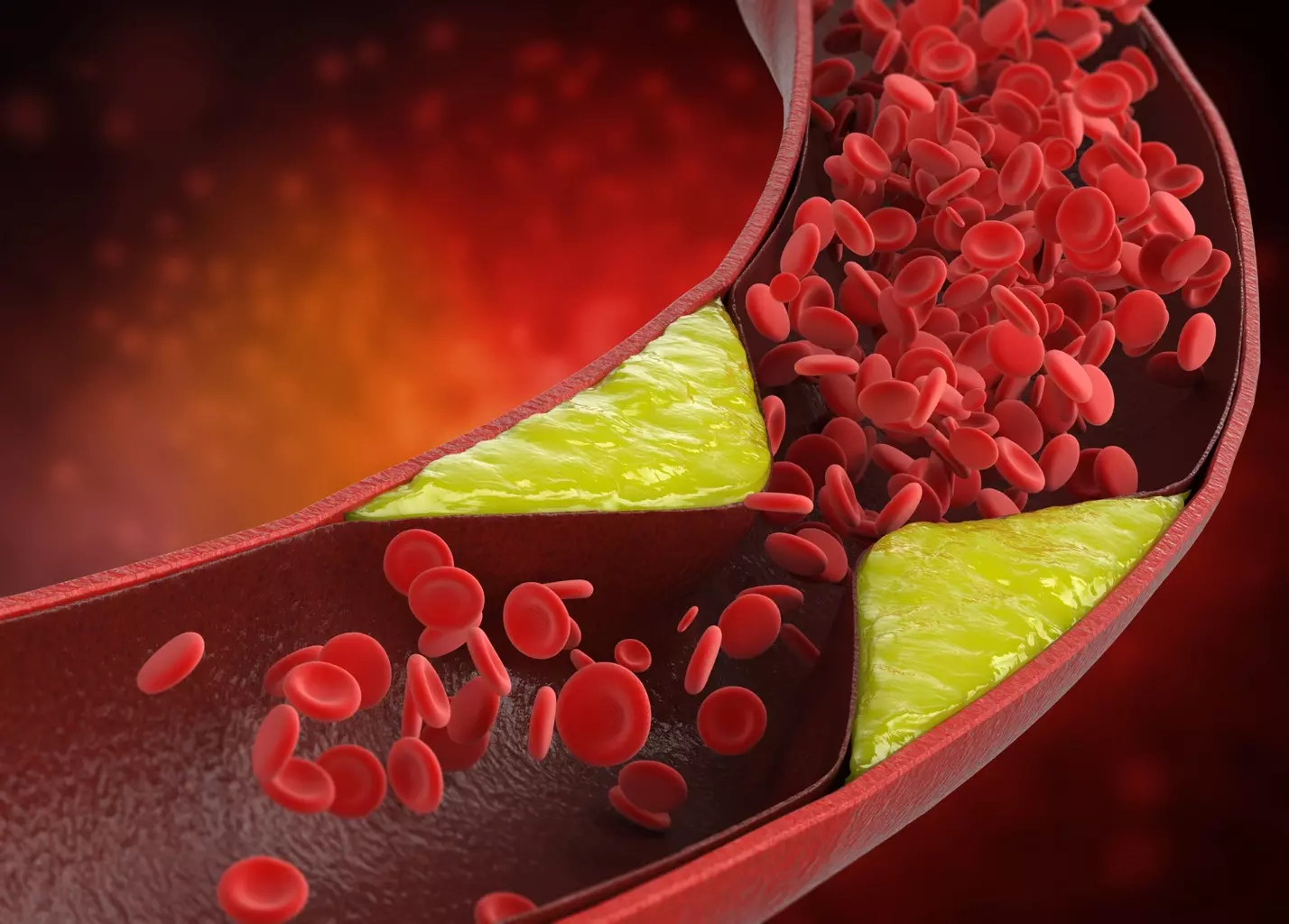
When a brain artery gets blocked, the tissue it supplies stops receiving oxygen and essential nutrients. This condition, often called cerebral ischemia, leads to brain cell damage or death. The extent of harm depends on where and how severe the blockage is. Immediate medical care can reduce long-term complications and improve recovery.
A CVA can be caused by a blood clot, fatty deposits in artery walls, or a clot that travels from another part of the body to the brain — known as an embolism. Understanding the definition of CVA medical helps identify these causes and underscores the need for prompt action.
Types of Cerebral Artery Blockages
There are several types of cerebral artery blockages, each with distinct features:
- Thrombotic Stroke: A blood clot forms within a brain artery.
- Embolic Stroke: A clot or debris forms elsewhere and travels to the brain.
- Atherosclerotic Blockage: Plaque buildup narrows or fully blocks an artery.
These are all categorized under the broader definition of CVA medical, which covers any condition disrupting normal blood flow in the brain.
Importance of Immediate Recognition
Recognizing the signs of a cerebral artery blockage early is essential. Fast treatment can restore blood flow, protect brain function, and improve outcomes. Acting quickly can be the difference between full recovery and lasting impairment.
If you or someone you know experiences symptoms of a CVA, get emergency help right away.
Blocked Brain Artery Symptoms: An Overview
It’s vital to recognize the warning signs of a blocked brain artery to prevent severe complications. These symptoms may vary depending on which part of the brain is affected.
Primary Warning Signs
Symptoms can appear suddenly and may include:
- Sudden numbness or weakness on one side of the body
- Difficulty speaking or understanding language
- Vision problems, such as double vision or vision loss in one eye
- Dizziness, imbalance, or lack of coordination
These are hallmark indicators of a CVA — understanding the definition of CVA medical helps people identify these early warning signs and take life-saving action.
How Symptoms Develop Over Time
Symptoms can appear within minutes or gradually worsen over hours. Some may resolve temporarily, as in a Transient Ischemic Attack (TIA), but these episodes are strong predictors of a full stroke.
Recognizing how symptoms progress and knowing the definition of CVA medical are both crucial for timely intervention and improved recovery chances.
| Symptom Development Pattern | Description | Clinical Implication |
| Acute Onset | Symptoms appear suddenly | Emergency medical attention required |
| Stuttering Onset | Symptoms fluctuate, may improve or worsen | Close monitoring necessary |
| Progressive Onset | Symptoms gradually worsen over time | Urgent medical evaluation needed |
Symptom Variations by Blockage Location
Where the blockage is in the brain artery affects the symptoms. For example, a blockage in the middle cerebral artery might cause aphasia, weakness, or vision problems. On the other hand, a blockage in the vertebral or basilar artery could lead to dizziness, double vision, or trouble with balance and coordination.
Knowing these differences is vital for diagnosing and treating the condition right. We’ll go into more detail about the different locations and their symptoms.
Sudden Numbness and Facial Drooping
When a brain artery gets blocked, you might feel sudden numbness or weakness in your face. This is a serious sign that needs quick attention. We’ll look at facial numbness and drooping, including patterns and related sensory issues.
Facial Numbness Patterns
Facial numbness can show up in different ways, depending on where and how bad the blockage is. Sudden numbness face can happen on one side or both. It might feel like tingling or pain too.
The numbness might go away quickly. But if it doesn’t, or if you have trouble speaking or walking, get help right away.
One-Sided Facial Drooping
A blocked brain artery can cause one side of your face to droop. This happens when the muscles on one side get weak or paralyzed. It can really change how you look and talk.
The drooping can be mild or very severe. It might just be a little droop or a big weakness on one side of your face.
Sensory Deficits in the Face
People with a blocked brain artery might also have other sensory deficits in their face. These can include feeling less touch, temperature, or pain. Some might feel tingling, burning, or prickling instead.
| Symptom | Description | Severity |
| Facial Numbness | Sudden loss of sensation in the face | Mild to Severe |
| One-Sided Facial Drooping | Weakness or paralysis of facial muscles on one side | Moderate to Severe |
| Sensory Deficits | Reduced or abnormal sensations in the face | Mild to Severe |
Arm and Leg Weakness or Paralysis
A blocked brain artery can cause sudden weakness or paralysis in the limbs. This usually happens on one side of the body. It’s a sign that needs quick medical help. We’ll look at how arm and leg weakness or paralysis relate to blocked brain arteries.
Hemiparesis and One-Sided Weakness
Hemiparesis is weakness on one side of the body, affecting the arm, leg, or both. It’s a common sign of a blocked brain artery. The weakness can be mild or severe, making daily tasks hard.
One-sided weakness often comes with other neurological problems. It’s important to know that hemiparesis affects more than just muscle strength. It can also impact coordination and balance.
Complete Paralysis Symptoms
In some cases, a blocked brain artery can cause complete paralysis of the arm or leg. This is called hemiplegia, a severe form of the problem. Complete paralysis can lead to significant disability and needs quick medical help.
Paralysis can start suddenly. It’s key to spot the signs early. We’ll talk about what makes paralysis more severe and its effects on patients.
Timing and Progression of Weakness
The timing and how weakness progresses are key in diagnosing a blocked brain artery. Symptoms can appear suddenly or slowly. Knowing when weakness starts helps doctors find the cause and the right treatment.
We’ve made a table to highlight the main points about arm and leg weakness or paralysis from a blocked brain artery:
| Symptom | Description | Clinical Significance |
| Hemiparesis | Weakness on one side of the body | Common symptom of cerebral artery blockage |
| Complete Paralysis | Total loss of motor function in arm or leg | Severe manifestation requiring immediate attention |
| Progression of Weakness | Symptoms can develop suddenly or gradually | Critical for determining underlying cause and treatment |
It’s vital to recognize the signs of arm and leg weakness or paralysis for timely medical care. We stress the need for quick medical help if you or someone you know shows these symptoms.
Speech and Language Difficulties
A blocked brain artery can cause sudden and severe speech and language problems. These issues can be very distressing for those who experience them.
Slurred Speech Patterns
Slurred speech, or dysarthria, is a common symptom. It happens when brain areas controlling speech muscles are affected.
Aphasia and Communication Problems
Aphasia is a significant speech and language issue caused by a blocked brain artery. It makes speaking, reading, writing, and understanding language hard.
Word-Finding Difficulties
Word-finding difficulties, or anomia, are a big part of aphasia. People know what they want to say but can’t find the right words.
| Symptom | Description | Impact |
| Slurred Speech | Unclear speech due to muscle control issues | Difficulty being understood |
| Aphasia | Difficulty with language processing | Challenges in communication, reading, and writing |
| Word-Finding Difficulties | Struggling to find the right words | Frustration and communication barriers |
Speech and language problems from a blocked brain artery are complex. It’s important to understand these symptoms for timely and effective help.
Vision Changes and Disturbances
Blocked brain arteries can cause a range of vision problems. These can be minor or severe. They are important signs of a blockage and its effect on the brain.
Vision Loss in One Eye
Vision loss in one eye, or monocular vision loss, happens when a brain artery is blocked. This affects the blood supply to the eye or the visual pathway. It can start suddenly and may last a short time or be permanent.
Key aspects to consider:
- Sudden onset is a red flag for a potential stroke.
- The extent of vision loss can vary from partial to complete blindness in the affected eye.
- Immediate medical attention is crucial to prevent permanent damage.
Double Vision Experiences
Double vision, or diplopia, can also occur from a blocked brain artery. It happens when nerves controlling eye movements are affected. This leads to misalignment of the eyes and seeing two images instead of one.
The causes can be complex:
- Nerve palsy or weakness due to ischemia.
- Mechanical issues with eye movement.
- Brainstem or cranial nerve involvement.
Visual Field Defects and Their Significance
Visual field defects are when part of the usual field of vision is lost. This can happen due to a blocked brain artery affecting the visual pathways. These defects can be hemianopia (half-vision loss) or quadrantanopia (quarter-vision loss), among others.
| Type of Visual Field Defect | Description | Common Cause |
| Hemianopia | Loss of half of the visual field | Blockage affecting the optic radiation or visual cortex |
| Quadrantanopia | Loss of a quarter of the visual field | Lesion in the visual pathway |
| Altitudinal Defect | Loss of the upper or lower half of the visual field | Ischemia or lesion affecting the visual pathway |
Understanding these vision changes is key for early detection and treatment of blocked brain arteries. Quick medical evaluation can greatly improve outcomes and prevent severe consequences.
Balance and Coordination Problems
A blocked brain artery can mess up the body’s balance and coordination. This leads to symptoms that can really affect how we move and live. It can make everyday life harder.
Dizziness and Vertigo Sensations
Dizziness and vertigo are common signs of a blocked brain artery. Dizziness feels like you’re lightheaded or unsteady. Vertigo makes it seem like you or the world around you is spinning. Both can make daily tasks hard to do.
Trouble Walking or Maintaining Posture
When balance and coordination are off, walking and staying upright can be tough. This raises the chance of falling and getting hurt. It’s hard to move around smoothly or stay balanced.
Coordination Loss in Limbs
Loss of coordination in limbs can make you clumsy or unable to do fine motor tasks. This symptom is tough because it affects how we move and do daily tasks like getting dressed or eating.
If you notice dizziness, vertigo, trouble walking, or coordination loss, get help right away. These signs might mean a blocked brain artery. Quick medical care can really help.
Cognitive and Mental Changes
A blocked brain artery can lead to various mental changes. These can range from mild confusion to severe disorientation. It’s important to understand these changes for both patients and their families.
Confusion and Disorientation
One immediate effect is confusion and disorientation. Patients might struggle to understand their surroundings or recognize people. They may also find it hard to follow conversations.
This confusion can quickly develop over a short time. In some cases, it can also cause agitation or restlessness.
Memory Lapses and Cognitive Impairment
Memory lapses are common symptoms. Patients might forget recent events or have trouble learning new things. Cognitive impairment can vary, affecting daily life and independence.
Managing these memory issues is crucial for patients and their caregivers. It requires strategies to help improve these functions.
Behavioral and Personality Changes
Behavioral and personality changes can also happen. These might include uncharacteristic mood swings, apathy, or irritability. These changes can be hard for loved ones to see.
It’s important to remember that these changes are due to the blocked artery, not a personal failing. This understanding helps in providing support and care.
Recognizing these changes as symptoms of a blocked brain artery is key. Seeking medical help early is crucial. It can greatly improve survival and quality of life.
Severe Headache and Pain Patterns
A severe headache might mean a blocked brain artery, which could be a stroke. If your headache is much worse or different, it could be serious. It’s key to know if it’s something more than just a headache.
Characteristics of Stroke-Related Headaches
Headaches from a stroke start suddenly and are very severe. They feel like the worst headache you’ve ever had, like a thunderclap. You might also feel sick to your stomach, vomit, or be very sensitive to light or sound.
- Sudden onset, often described as “explosive”
- Severe pain, usually on one side of the head
- Associated symptoms like confusion, difficulty speaking, or weakness
Differentiating from Migraines and Tension Headaches
Telling a stroke headache from migraines or tension headaches is hard. But, stroke headaches often have other symptoms that migraines or tension don’t. Knowing the difference is important for getting the right help.
| Headache Type | Characteristics | Associated Symptoms |
| Stroke-related | Sudden, severe, often one-sided | Confusion, weakness, difficulty speaking |
| Migraine | Pulsating, moderate to severe | Nausea, vomiting, sensitivity to light/sound |
| Tension | Dull, band-like pressure around the head | Mild sensitivity to light or sound |
When Headache Indicates Emergency
If a headache means you might be having a stroke, you need to act fast. If you have a headache with confusion, trouble speaking, or sudden weakness, call for emergency help. Spotting these signs can save a life.
- Call emergency services right away if you think you’re having a stroke.
- Tell them as much as you can about your symptoms and when they started.
- Do what the emergency responders tell you to do.
Symptoms by Artery Location
The location of an artery blockage in the brain greatly affects the symptoms. Different arteries carry blood to different parts of the brain. A blockage can cause various neurological problems, depending on the area affected.
Carotid Artery Blockage Symptoms
The carotid arteries are two major arteries in the neck. They supply blood to the brain. A blockage in the carotid artery can cause symptoms like:
- Transient monocular blindness (temporary blindness in one eye)
- Hemiparesis or hemiplegia (weakness or paralysis on one side of the body)
- Aphasia (speech difficulties)
- Facial drooping
These symptoms happen because the carotid artery feeds a big part of the brain’s hemispheres. A blockage can reduce blood flow to areas that control movement, speech, and vision.
Vertebral and Basilar Artery Symptoms
The vertebral and basilar arteries supply blood to the back parts of the brain. Symptoms of a blockage in these arteries include:
| Symptom | Description |
| Dizziness or vertigo | Sensation of spinning or loss of balance |
| Double vision | Seeing two images of a single object |
| Dysarthria | Slurred or difficult speech |
| Ataxia | Loss of coordination and balance |
A blockage in these arteries can lead to serious problems, like locked-in syndrome or coma. This shows the need for quick medical help.
“The symptoms of vertebral and basilar artery occlusions can be particularly challenging to diagnose due to their non-specific nature, often mimicking other conditions.”
Middle Cerebral Artery Blockage Signs
The middle cerebral artery (MCA) is a big artery often affected by blockages. Symptoms of an MCA blockage include:
- Hemiparesis or hemiplegia
- Aphasia (if the dominant hemisphere is affected)
- Spatial neglect
- Visual field defects
An MCA blockage can cause big problems with thinking and moving, depending on the hemisphere affected.
Knowing the specific symptoms of different artery blockages is key for quick diagnosis and treatment. We stress the importance of recognizing these signs to get the right care.
Transient Ischemic Attacks: Warning Mini-Strokes
TIAs, or ‘mini-strokes,’ are short episodes that might signal a bigger stroke. They show stroke-like symptoms but these go away in 24 hours, often sooner.
Differentiating TIAs from Strokes
The main difference between a TIA and a stroke is how long symptoms last. TIAs are short and don’t cause lasting brain damage. But, they’re serious because they might lead to a bigger stroke.
It’s key to know the difference between TIAs and strokes for the right medical care. We’ll look at how TIA symptoms can differ and why they’re important to notice.
Duration and Patterns of TIA Symptoms
TIA symptoms are like a stroke’s but last only a few minutes to hours. They might include sudden numbness, trouble speaking, or vision problems. These symptoms are short-lived.
How often and how long TIA symptoms last can vary. Some people have one TIA, while others have many in a short time. Spotting these patterns is vital for quick medical help.
Why TIAs Should Never Be Ignored
TIAs are a warning that a stroke might happen soon. People who have a TIA are more likely to have a stroke within a few days to a week. So, it’s crucial to get medical help right away if you think you’re having a TIA.
We stress that TIAs should never be ignored. Quick medical check-ups can stop a stroke or make it less severe. Knowing the signs of a TIA and acting fast can save lives.
When to Seek Emergency Medical Attention
It’s key to spot the signs of a blocked brain artery early. A stroke needs quick action to lessen damage and better outcomes.
FAST Assessment Technique
The FAST method is a quick way to spot stroke signs. FAST means Face, Arm, Speech, and Time.
- Face: Ask the person to smile. Does one side of their face droop?
- Arm: Ask the person to raise both arms. Does one arm drift downward?
- Speech: Ask the person to repeat a simple sentence. Is their speech slurred or hard to understand?
- Time: Time is crucial. If they show any symptoms, call for help right away.
Critical Time Windows for Treatment
Quick medical help is vital for recovery. For ischemic strokes, clot-busting drugs like tPA work best within hours of symptoms starting.
Knowing when to get treatment can greatly improve patient results. Every second matters with a blocked brain artery.
What to Tell Emergency Responders
When you call for help, give clear details. Be ready to talk about symptoms, when they started, and any health history.
- State where you are and the emergency.
- Give the patient’s age and any health issues.
- Include any medicines they’re taking.
Being ready and knowing what to say helps emergency teams help better.
Diagnosis of Blocked Brain Arteries
Figuring out if brain arteries are blocked needs a detailed plan. This includes first checks, advanced scans, and blood tests. We’ll dive into these steps to see how they help spot and treat blockages in brain arteries.
Initial Assessment Techniques
First, doctors look at a patient’s past health and do a physical check. They search for signs like sudden numbness or trouble speaking. These could mean a stroke or a mini-stroke.
Clinical evaluation is key to figuring out how serious the problem is. Doctors check the brain’s function, look for risk factors like high blood pressure, and review the patient’s overall health.
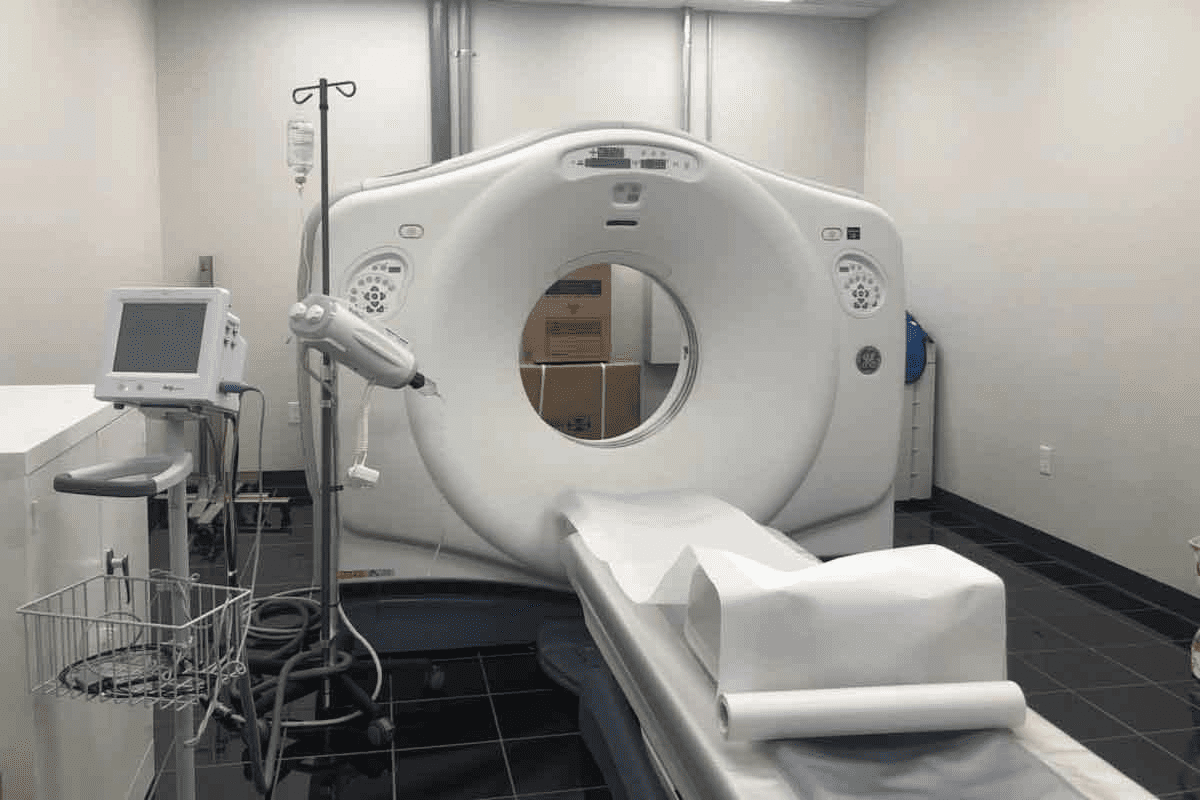
Imaging Studies and Their Findings
Scans are vital for spotting blocked brain arteries. MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) angiography give clear views of the brain’s blood vessels. They help find blockages or narrowing.
| Imaging Technique | Key Findings | Clinical Utility |
| MRI Angiography | Detailed images of blood vessels, stenosis, or occlusion | High sensitivity for detecting vascular abnormalities |
| CT Angiography | Rapid assessment of cerebral vasculature, useful in emergencies | Quick and accurate for identifying large vessel occlusions |
| Carotid Ultrasound | Evaluation of carotid artery stenosis or plaque | Non-invasive, useful for screening and monitoring |
These scans help us not just find the problem but also plan the right treatment.
Laboratory Tests and Biomarkers
Lab tests are crucial in figuring out what’s causing the blockage. They check for things like high cholesterol or diabetes. These tests help us understand the patient’s health better.
Biomarkers like troponin and D-dimer give clues about the heart and possible blood clots. Tests like complete blood count (CBC) and electrolyte panels also help. They check the patient’s overall health and find any other health issues that might be causing the blockage.
By combining the results of first checks, scans, and lab tests, we can accurately find blocked brain arteries. Then, we can create a treatment plan that fits the patient’s needs.
Treatment Approaches for Cerebral Artery Blockages
Cerebral artery blockages need quick and thorough treatment. This includes emergency actions, medicines, and surgery. The right treatment depends on the blockage’s location, how bad it is, and the patient’s health.
Emergency Interventions
Quick action is key when a cerebral artery blockage happens. We focus on treatments that quickly get blood flowing again. Some emergency steps include:
- Intravenous thrombolysis: Giving clot-busting drugs through a vein to break up the blockage.
- Mechanical thrombectomy: Using a catheter to remove the clot from the artery.
These steps are urgent, showing the need for fast medical help if you think you have a blockage.
Medication Therapies
Medicine is vital in treating cerebral artery blockages. It helps in the first stages and prevents future problems. We often give:
- Antiplatelet agents: To stop platelets from sticking together and forming clots.
- Anticoagulants: To stop new clots from forming and old ones from getting bigger.
- Statins: To lower cholesterol and prevent more blockages.
These medicines are key in managing blockages and lowering stroke risk.
Surgical and Endovascular Procedures
Sometimes, surgery or endovascular methods are needed for blockages. These include:
- Carotid endarterectomy: Surgery to remove plaque from the carotid arteries.
- Angioplasty and stenting: Procedures to open narrowed arteries and keep them open with a stent.
These options depend on the patient’s condition and the blockage’s details.
Effective treatment for cerebral artery blockages needs a detailed plan for each patient. By using emergency actions, medicines, and sometimes surgery, we can greatly improve patient outcomes.
Recovery and Rehabilitation Process
The journey to recovery after a stroke is key to getting back lost functions and improving life quality. Every person’s path is different, and recovery times can vary a lot.
Timeline for Recovery
The time it takes to recover from a stroke varies a lot. Most people see big improvements in the first few months. But, with the right therapy, recovery can take a year or more.
Knowing the recovery timeline is important for setting goals and planning therapy. The first 30 days are often the most critical for big improvements.
Physical and Occupational Therapy
Physical and occupational therapy are key in stroke recovery. Physical therapy helps improve movement, strength, and coordination. It helps patients do daily tasks again.
- Physical therapists help with walking, balance, and physical function.
- Occupational therapy teaches skills for daily living, like dressing and bathing.
These therapies are customized for each person. They work together to help patients reach their goals.
Speech and Cognitive Rehabilitation
Speech and cognitive rehabilitation are vital for many stroke survivors. Speech therapy helps with communication, like speaking clearly and understanding others.
- Speech therapists help patients communicate better.
- Cognitive therapy improves memory, attention, and solving problems.
These therapies help overcome challenges and improve life quality.
A complete rehabilitation program includes physical, occupational, speech, and cognitive therapies. This approach can greatly improve recovery for stroke survivors.
Prevention Strategies for Brain Artery Blockages
We can lower the risk of brain artery blockages by making lifestyle changes and using medical treatments. It’s key to keep our heart healthy and avoid strokes.
Lifestyle Modifications
Healthy choices are key to avoiding brain artery blockages. Regular physical activity keeps blood vessels healthy. We should do at least 150 minutes of moderate exercise or 75 minutes of vigorous exercise weekly.
Eating a balanced diet is also important. Foods like fruits, veggies, whole grains, and lean proteins help. We should also watch our intake of bad fats and sodium.
Medical Management of Risk Factors
Managing risk factors is crucial. Hypertension is a big risk, and we need to control it. Working with our doctor to keep blood pressure in check is vital.
Managing diabetes is also key. Keeping blood sugar levels right helps avoid artery problems. This can be done through diet, exercise, and medication.
Monitoring and Follow-Up Recommendations
Regular check-ups with our doctor are important. We need to keep an eye on blood pressure, cholesterol, and sugar levels. Early detection helps us act fast and improve our health.
People with a history of heart disease or risk factors might need more frequent checks. We should work with our doctor to create a plan for monitoring.
By making lifestyle changes, managing risk factors, and getting regular check-ups, we can lower the risk of brain artery blockages. This helps keep our heart healthy.
Conclusion
Knowing the signs of blocked brain arteries is key to getting help fast. We talked about symptoms like sudden numbness, weakness in arms and legs, trouble speaking, and vision changes. Spotting these signs early can help prevent serious damage.
Preventing blocked brain arteries is also important. Making healthy lifestyle choices, managing health conditions, and watching for risk factors can help. It’s vital to know your risk and take steps to prevent strokes.
By being aware of symptoms and taking prevention steps, we can fight strokes. Keeping informed and taking action is crucial for brain health. Let’s all work together to protect our brains.
FAQ
What are the common symptoms of a blocked brain artery?
Symptoms include sudden numbness or weakness in the face, arm, or leg. You might also have trouble speaking or understanding speech. Vision changes, dizziness, and severe headaches are other signs.
How does a blocked brain artery affect the body?
A blocked artery can cause a stroke. This can damage the brain. It might lead to paralysis, speech problems, and memory loss.
What is the difference between a stroke and a Transient Ischemic Attack (TIA)?
A stroke is more serious, causing permanent damage. A TIA is temporary, lasting less than 24 hours. It’s a warning sign for a stroke.
What is the FAST assessment technique?
FAST helps spot stroke symptoms quickly. It stands for Face, Arm, Speech, and Time. Check for drooping, weakness, slurring, and call for help right away.
How quickly should I seek medical attention if I experience stroke symptoms?
Get help fast if you have stroke symptoms. Quick treatment is key to lessening brain damage.
What diagnostic tests are used to confirm a blocked brain artery?
Tests include CT or MRI scans and lab tests for biomarkers. They help see how bad the blockage is.
What are the treatment options for a blocked brain artery?
Treatments include emergency thrombolysis and medicines to stop clots. Surgery or endovascular procedures may also be used to open the artery.
How long does recovery from a stroke take?
Recovery time varies. It depends on the stroke’s severity and the success of therapy. This includes physical, occupational, and speech therapy.
What lifestyle changes can help prevent brain artery blockages?
Eating well, exercising, and managing blood pressure and cholesterol are key. Not smoking also helps.
Can a blocked brain artery be prevented?
While some risks can’t be changed, managing conditions like high blood pressure and cholesterol helps. A healthy lifestyle also reduces risk.
What are the signs of a blocked carotid artery?
Signs include TIAs or mini-strokes. Symptoms are temporary blindness, weakness or numbness, and speech trouble.
How are TIAs related to blocked brain arteries?
TIAs are warning signs before a stroke. They show a temporary blockage or reduced blood flow in a brain artery.
What is the role of rehabilitation after a stroke?
Rehabilitation helps patients regain lost functions. It improves their quality of life through various therapies.
References
National Institutes of Health. Stroke symptoms early recognition crucial for effective treatment. Retrieved from https://www.nhlbi.nih.gov/health/stroke