Last Updated on December 3, 2025 by Bilal Hasdemir
surgical critical care
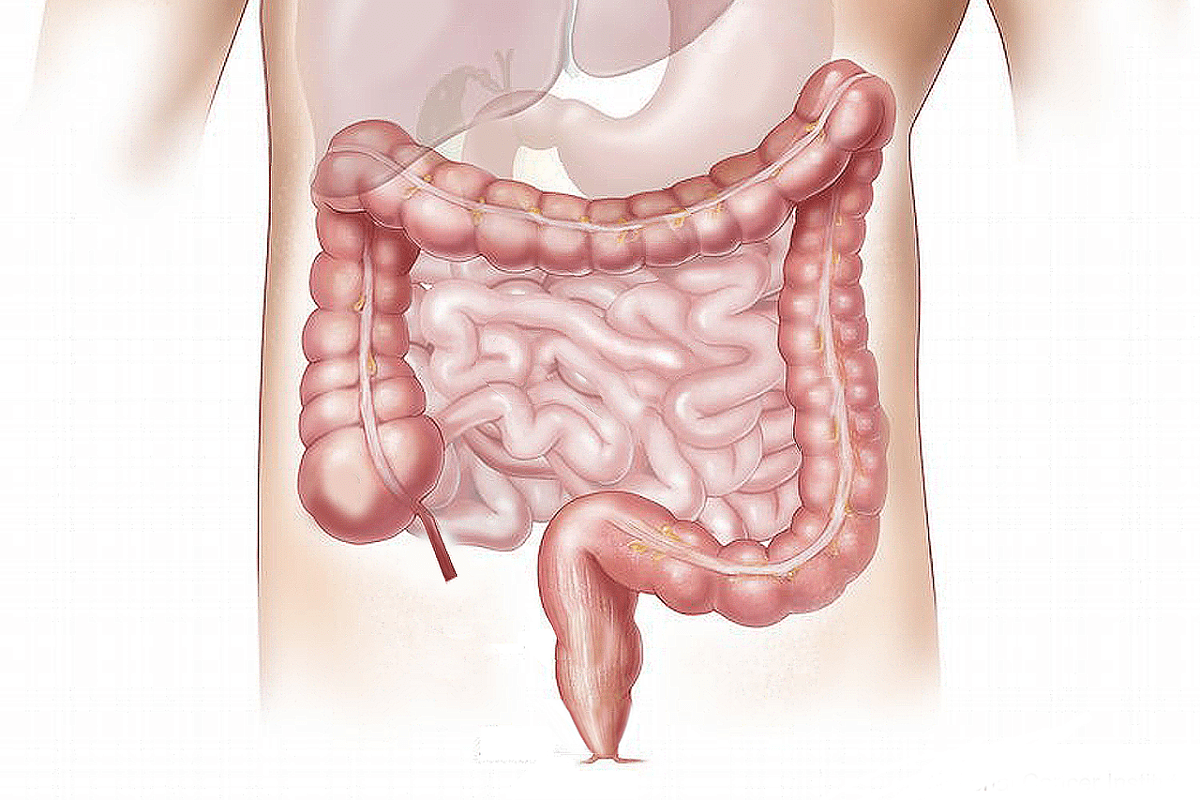
Trauma surgeons are key in saving lives, with over 200,000 deaths from trauma in the U.S. each year. Trauma surgery is important for treating severe injuries. But, it’s not the same as surgical critical care. These two fields have different roles in patient care. Is surgical critical care the same as trauma surgery? We explain the crucial differences. Get the essential facts on these specialties.
Trauma surgeons do emergency surgeries for people with serious injuries or illnesses. They fix trauma caused by injuries and illnesses. Surgical critical care, however, deals with the care of very sick patients in the ICU. It ensures they get the care needed to get better.
Key Takeaways
- Trauma surgery and surgical critical care are distinct medical specialties.
- Trauma surgeons specialize in emergency surgeries for critical injuries or illnesses.
- Surgical critical care focuses on ICU management for critically ill patients.
- Both specialties are crucial in treating patients with critical illnesses.
- Understanding the difference between these specialties can improve patient outcomes.
Defining Surgical Critical Care and Trauma Surgery
A dimly lit surgical theater, the air thick with tension. In the foreground, a team of skilled surgeons perform a complex trauma procedure, their scrubs stained with blood as they work intently to save a critically injured patient. Bright surgical lamps cast a stark illumination, highlighting the precision of their movements and the gravity of the situation. In the middle ground, monitors display vital signs and diagnostic scans, providing the medical team with crucial real-time data. The background is a blur of activity, with nurses and technicians assisting in the delicate operation. The atmosphere is one of focused intensity, where every second counts in the race to stabilize the patient and provide the highest level of surgical critical care.
Surgical critical care and trauma surgery are two important areas in medicine. They both deal with serious cases but in different ways. Each has its own main goals and methods.
Core Focus of Surgical Critical Care
Surgical critical care focuses on caring for very sick patients in an ICU setting. It involves a detailed approach to severe conditions. This includes:
- Monitoring and supporting vital organ functions
- Managing complex medical conditions
- Coordinating care among multidisciplinary teams
- Implementing evidence-based practices to improve patient outcomes
Specialists in surgical critical care are key in keeping patients stable and preventing more harm.
Primary Responsibilities in Trauma Surgery
Trauma surgery deals with injuries from accidents. Trauma surgeons do:
- Assessing the severity of injuries upon patient admission
- Performing emergency surgical procedures to stabilize patients
- Managing post-operative care to ensure proper recovery
- Collaborating with other healthcare professionals to provide comprehensive care
Trauma surgery needs a lot of skill and quick thinking in emergency situations.
In summary, surgical critical care and trauma surgery are both vital for treating critical cases. They have different focuses and tasks. Knowing these differences helps us understand the complex care these specialists offer.
Historical Development of Both Specialties

High-contrast clinical illustration depicting the historical progression of trauma surgery, showcased against a muted backdrop of vintage medical equipment and architectural elements. In the foreground, a collage of surgical implements and techniques from different eras, rendered in a technical, anatomical style. The middle ground features shadowy silhouettes of surgeons from bygone times, performing groundbreaking procedures. The background is a somber, dimly lit space reminiscent of an old operating theater, with dramatic lighting casting dramatic shadows. The overall tone conveys the gravity, innovation, and evolution of this critical medical specialty.
Surgical critical care and trauma surgery have unique beginnings. These specialties have grown thanks to medical science, technology, and the hard work of pioneering surgeons.
Evolution of Surgical Critical Care
The field of surgical critical care grew from the need for better care after surgery. Advances in ICU management and new monitoring tools have been key. These changes have greatly improved patient care.
Now, surgeons get special training in surgical critical care. This training focuses on teamwork in the ICU. Surgeons work with other healthcare professionals to give the best care.
Training Pathways: How Surgeons Enter Each Field
A surgical fellowship training room, illuminated by soft, even lighting. In the foreground, a team of surgeons intently focused on a complex procedure, their hands steady and their movements precise. The middle ground features state-of-the-art medical equipment, including advanced diagnostic tools and specialized surgical instruments. In the background, a panoramic view of a modern hospital setting, with clean lines and a sterile, professional atmosphere. The overall scene conveys a sense of intense focus, dedication, and the pursuit of medical excellence, embodying the essence of surgical critical care training.
Becoming a specialist in Surgical Critical Care or Trauma Surgery takes hard work and dedication. Surgeons must go through many educational and clinical steps to get the right skills.
Surgical Critical Care Fellowship Requirements
To specialize in Surgical Critical Care, surgeons first finish a general surgery residency. Then, they do a Surgical Critical Care fellowship. These fellowships are very competitive and offer deep training in caring for very sick surgical patients.
Fellowship programs in Surgical Critical Care teach a lot, like how to monitor blood flow and manage breathing. Surgeons learn to work with teams in intensive care units to give top-notch care.
Trauma Surgery Training Pathway
The path to becoming a Trauma Surgeon is also tough. Trauma surgeons start with a general surgery residency. They get trauma experience through emergency surgery and trauma service rotations.
Many trauma surgeons get extra training through fellowship programs in Trauma Surgery or Acute Care Surgery. These programs teach how to handle trauma patients and do complex surgeries needed in trauma care.
To be certified in Trauma Surgery, surgeons get a certificate from groups like the American Association for the Surgery of Trauma. This shows they are experts in trauma care.
Day-to-Day Responsibilities Compared
A brightly lit, modern intensive care unit (ICU) with a team of medical professionals diligently monitoring and caring for critically ill patients. In the foreground, a nurse adjusts the settings on a high-tech medical device, their face a study in concentration. In the middle ground, a doctor reviews a patient’s chart, their brow furrowed with thought. The background reveals a panoramic view of the ICU, with rows of beds, specialized equipment, and the quiet hum of life-saving machinery. The scene conveys a sense of order, precision, and the unwavering commitment of the medical staff to providing the best possible care.
It’s important to know what surgical critical care and trauma surgery professionals do every day. Both need a lot of skill and must make quick decisions. But, their daily tasks are quite different.
Typical Day in Surgical Critical Care
A surgical critical care specialist spends their day in the ICU with very sick patients. They:
- Watch patients’ vital signs and change treatment plans as needed
- Manage life-saving treatments like breathing machines and dialysis
- Work with a team to give patients the best care
- Make tough decisions quickly, often under a lot of pressure
Good ICU management is key. It needs a deep understanding of critical care and the ability to manage tasks well.
Routine Responsibilities in Trauma Surgery
Trauma surgeons work in emergency rooms. Their day is filled with:
- Checking patients when they come in and figuring out how bad their injuries are
- Doing emergency surgeries to keep patients stable
- Making fast decisions based on the patient’s condition and what they know
- Working with other doctors to give patients the best care right away
The ability to do emergency procedures well is crucial. It greatly affects how patients do. Trauma surgeons must also be good at patient monitoring. They need to spot changes in a patient’s condition fast and act quickly.
In summary, surgical critical care specialists and trauma surgeons both play key roles in patient care. But, their daily tasks show their different areas of expertise. Knowing these differences helps us understand the complexity of their work and the skills needed to be great in these fields.
The Surgical Critical Care Environment
A modern surgical ICU monitoring system, illuminated by warm, diffused lighting. In the foreground, a high-resolution display shows real-time vitals and waveforms, meticulously tracking the patient’s vital signs. The middle ground features a array of medical equipment, including infusion pumps, ventilators, and specialized monitoring devices, all seamlessly integrated to provide comprehensive care. The background depicts a spacious, sterile environment with clean, white walls and muted tones, creating a calming, professional atmosphere conducive to critical care.
The ICU is key in surgical critical care. It’s where we manage very sick patients. A team of experts works together to give top-notch care.
ICU Management Principles
Managing the ICU well means following some important rules. Patient-centered care is the top priority. We make choices that are best for the patient.
We also use evidence-based practice. This means we apply the newest research to our care plans.
Good ICU management also means planning and teamwork. This includes:
- Checking how sick each patient is and using the right resources
- Putting in place steps to stop infections from spreading
- Working with other hospital teams for complete care
| ICU Management Aspect | Description | Benefits |
| Patient-Centered Care | Care tailored to individual patient needs | Improved patient outcomes, enhanced patient satisfaction |
| Evidence-Based Practice | Clinical decisions guided by latest research | Better clinical outcomes, reduced variability in care |
| Infection Control | Measures to prevent hospital-acquired infections | Reduced morbidity, mortality, and healthcare costs |
Technology and Monitoring Systems
The ICU uses advanced monitoring systems to watch over patients. These include:
- Hemodynamic monitoring to check heart function
- Respiratory monitoring for patients with breathing problems
- Neurological monitoring to spot early brain issues
These tools help us catch problems early and act fast. They help us give our patients the best care possible.
Trauma Surgery: From Emergency Department to Operating Room
A detailed scene of a trauma surgery process, set in a well-lit operating room. In the foreground, a team of skilled surgeons and nurses perform delicate procedures on a patient, their faces focused and determined. The middle ground captures the hustle and bustle of the room, with various medical equipment and instruments meticulously arranged. In the background, a view through a large window reveals the emergency department, where medical staff attend to incoming patients. The scene is imbued with a sense of urgency and precision, conveying the critical nature of trauma surgery.
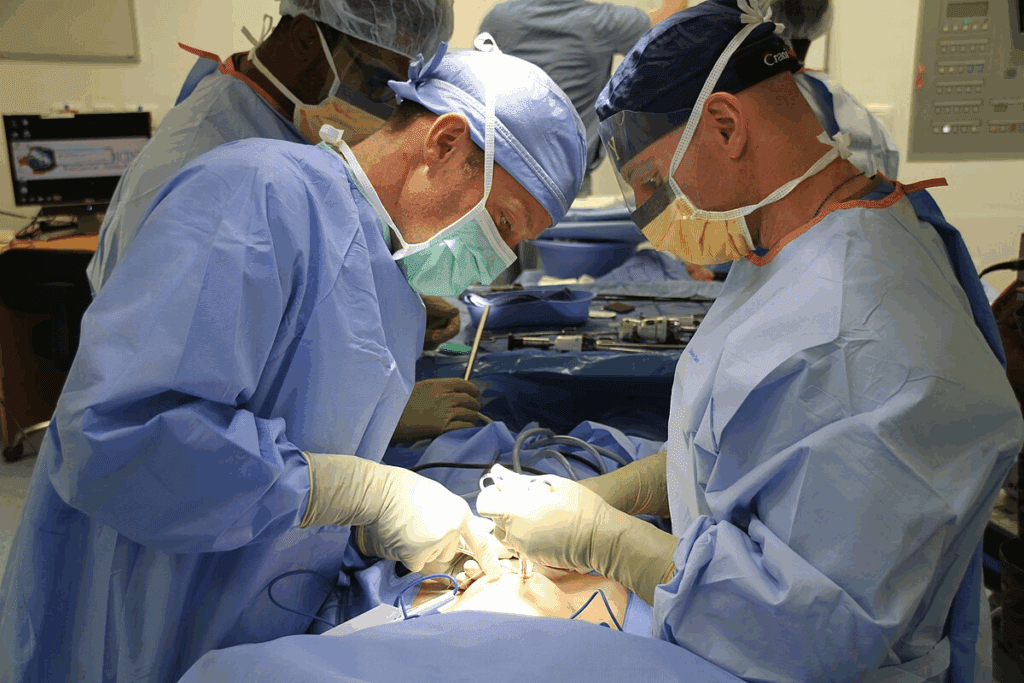
The journey of a trauma patient from the emergency department to the operating room is complex. It needs expertise, quick decisions, and precise actions. Trauma surgeons are key, handling everything from the first check-up to emergency surgeries.
Initial Assessment and Resuscitation
When trauma patients arrive, they get a quick check to find serious injuries. Trauma surgeons team up with the emergency department to focus on the most urgent needs. They use resuscitation techniques like fluids and blood transfusions to keep the patient stable.
The Advanced Trauma Life Support (ATLS) protocol helps guide this initial phase. Effective communication among the team is crucial. It makes sure everyone knows the patient’s status and the planned treatments.
Emergency Surgical Procedures
When surgery is needed, trauma surgeons must act fast and make quick decisions. They perform various surgeries, like exploratory laparotomy, to fix damaged areas. The main goal is to stop bleeding, prevent more damage, and stabilize the patient.
Surgical techniques in trauma surgery are very specialized. They often involve temporary fixes to stabilize the patient before more detailed repairs. Advanced surgical technologies, like intraoperative ultrasound, help in treating complex injuries.
In summary, trauma surgery is a challenging field. It demands technical skill, the ability to work under pressure, and making fast, critical decisions. The journey from the emergency department to the operating room shows the complexity and importance of trauma care.
Acute Care Surgery: The Evolving Hybrid Model
Detailed scene of a modern acute care surgery suite, showcasing the intricate, high-tech environment where critical care procedures are performed. In the foreground, a surgical team in sterile gowns and masks hover over an operating table, their hands skillfully wielding precision instruments. The middle ground reveals advanced medical equipment, monitors, and diagnostic tools, bathed in a cool, blue-tinted lighting. In the background, a series of glass-walled rooms allow for observation and consultation, reflecting the collaborative, multidisciplinary nature of acute care surgery. The atmosphere conveys a sense of urgency, focus, and a relentless pursuit of saving lives through the seamless integration of emergency, trauma, and critical care.
Acute care surgery blends trauma surgery, surgical critical care, and emergency general surgery. This mix offers a deeper way to handle urgent surgical needs. It’s changing how we give surgical care, especially in emergencies.
Integration of Emergency General Surgery
Emergency general surgery is a big part of acute care surgery. It deals with urgent issues like appendicitis and cholecystitis. This approach makes care for patients more efficient and effective.
The benefits of this mix are clear:
- Patients get better care because of quick actions
- Teams work better together
- Resources are used more wisely in emergencies
Relationship to Both Trauma and Critical Care
Acute care surgery is closely tied to trauma surgery and surgical critical care. The skills from these areas are vital for handling complex cases. For example, trauma resuscitation and critical care methods are used in treating acute surgical issues.
Some key areas of overlap are:
- Resuscitation techniques from trauma care
- Strategies for managing post-operative critical care
- Surgical methods useful in trauma and emergency general surgery
Understanding these connections helps us see the full scope of acute care surgery. It shows its importance in today’s surgical field.
Managing Critical Illness in Surgical Patients
Critical illness in surgical patients is a big challenge. It needs careful management strategies. Surgical patients can get very sick, like sepsis or organ failure, and need special care.
Critical illness in these cases is risky. Quick and effective care is key. We’ll look at how surgical critical care tackles these issues, focusing on organ support and sepsis management.
Organ Failure and Support Systems
Organ failure is a big worry for critically ill surgical patients. We use advanced life-support systems to help. For example, mechanical ventilation helps with breathing problems, and renal replacement therapy helps with kidney issues.
Managing organ failure takes a team effort. Intensivists, surgeons, and other experts work together. We tailor care to each patient’s needs.
Sepsis Recognition and Management
Sepsis is a serious condition that can harm the body’s own tissues and organs. We focus on catching sepsis early and treating it fast. This includes giving antibiotics quickly and finding and fixing the infection source.
The management of sepsis is all about a detailed plan. This includes supporting the heart and blood, controlling infections, and watching for complications. We follow the best sepsis care practices to help our patients.
We use advanced systems and proven methods to help critically ill surgical patients. Our goal is to give them the best care possible, focusing on their needs.
Trauma Centers: Structure and Surgical Roles
It’s key to know how trauma centers are set up and what surgical roles they have. These centers are ranked from Level I to Level V, with Level I being the top. This ranking shows how well they can handle trauma cases.
Level I-V Trauma Center Requirements
Trauma centers fall into five levels, each needing different care levels. Level I trauma centers offer the most care. They have trauma surgeons on call 24/7 and many specialties.
- Level I: Comprehensive care, including research and education.
- Level II: Provides initial definitive care for trauma patients.
- Level III: Offers prompt assessment, resuscitation, and stabilization.
- Level IV: Provides initial evaluation, stabilization, and possible transfer.
- Level V: Offers stabilization and transfer to a higher-level facility.
Surgical Critical Care Within Trauma Systems
Surgical critical care is crucial in trauma systems. It ensures critically ill or injured patients get the right care. Trauma surgeons team up with intensivists and others to manage these patients.
The role of surgical critical care in trauma centers includes:
- Early recognition and management of potential complications.
- Advanced life-support measures, including mechanical ventilation and hemodynamic monitoring.
- Coordination with multidisciplinary teams to optimize patient outcomes.
Understanding trauma centers’ structure and roles helps us see the complexity and teamwork needed for trauma care.
Procedural Skills: What Each Specialist Performs
Critical care specialists and trauma surgeons handle complex surgeries. They get extensive training in many surgical skills.
Common Procedures in Surgical Critical Care
Surgical critical care specialists manage critically ill patients with various procedures. Some common ones are:
- Central line placements for monitoring and fluid resuscitation
- Bronchoscopy for diagnosing and managing respiratory issues
- Bedside ultrasound to check heart function and manage fluids
- Tracheostomy for long-term airway access
These tasks need precision and a deep understanding of the patient’s health. This shows the specialized skills of surgical critical care specialists.
Typical Trauma Surgery Operations
Trauma surgeons handle emergency surgeries for acute injuries. Some common operations are:
- Damage control laparotomy to stop bleeding and prevent infection
- Thoracotomy for thoracic injuries, including cardiac arrest
- Vascular repair and reconstruction for major blood vessel injuries
- Fasciotomy to prevent limb loss from compartment syndrome
Trauma surgeons must be skilled in these critical surgical procedures. Their work is vital for saving lives and preventing disability.
The wide range of skills needed in surgical critical care and trauma surgery shows their advanced training. Their ability to handle complex surgeries under pressure is key to providing the best patient care.
Post-Operative Care: The Critical Intersection
Surgical critical care is key in managing patients after surgery. It helps them recover safely. Good post-operative care is essential to avoid complications and aid in healing.
Immediate Post-Operative Management
Right after surgery, patients need close watch for issues like bleeding or breathing problems. Surgical critical care teams are trained to spot and handle these problems quickly. This ensures the best results for patients.
“The quality of post-operative care greatly affects patient recovery and long-term health,” highlights the need for careful management during this time.
Long-term Critical Care After Major Surgery
Patients who have major surgery often need care for a long time. We provide full support, looking after the surgical site and the patient’s overall health.
Long-term care deals with possible long-term issues like infections or organ problems. Our teams work with patients and their families to tailor care. This ensures the best recovery for each person.
As we improve in surgery and care, teamwork between surgical teams, critical care experts, and others is vital. Together, we can make patient outcomes better and improve life quality for those having major surgery.
Certification and Credentialing Differences
Becoming a specialist in surgical critical care or trauma surgery has its own path. Both areas need hard work and dedication. But, the ways to get certified are different.
Board Certification in Surgical Critical Care
Surgeons in surgical critical care get certified by the American Board of Surgery (ABS). They first finish a surgical residency. Then, they do a fellowship in surgical critical care. The ABS certifies them for managing critically ill patients.
Key requirements for certification in Surgical Critical Care include:
- Completion of a general surgery residency program approved by the Accreditation Council for Graduate Medical Education (ACGME)
- Completion of a surgical critical care fellowship program approved by the ACGME
- Passing the Surgical Critical Care certification examination administered by the ABS
Trauma Surgery Qualifications
Trauma surgeons get their skills through residency and sometimes a fellowship in trauma surgery. There’s no specific board certification for trauma surgery. But, they can show their skills through education and professional activities.
Qualifications for trauma surgeons may include:
- Completion of a general surgery residency program
- Fellowship training in trauma surgery or acute care surgery
- Participation in continuing education programs focused on trauma care
Let’s look at the differences in certification and training:
| Aspect | Surgical Critical Care | Trauma Surgery |
| Board Certification | Available through the American Board of Surgery | No separate certification; often part of general surgery or acute care surgery training |
| Fellowship Training | Required for certification in Surgical Critical Care | Optional but highly recommended for trauma surgery specialization |
| Residency Training | Must complete general surgery residency | Must complete general surgery residency |
It’s key to know these differences for surgeons and hospitals. As surgery evolves, the need for specialized training and certification grows.
The Multidisciplinary Approach in Both Fields
In both surgical critical care and trauma surgery, teamwork is key. We work together to meet our patients’ complex needs. This teamwork is crucial for quality care.
Team Composition in the Surgical ICU
The Surgical Intensive Care Unit (ICU) has a diverse team. This team includes intensivists, surgeons, nurses, and more. Each member brings their skills to help patients fully.
Nurses play a big role in the ICU. They watch over patients closely and give treatments. Their constant watch helps catch any changes quickly.
Trauma Team Dynamics
In trauma surgery, teamwork is just as important. Trauma teams have surgeons, emergency doctors, nurses, and others. They work fast and together to handle emergencies.
Good communication and clear roles make the trauma team strong. This teamwork is key in saving lives during emergencies.
| Team Member | Role in Surgical ICU | Role in Trauma Team |
| Surgeons | Perform surgeries, oversee patient care | Lead trauma team, perform emergency surgeries |
| Nurses | Primary caregivers, monitor patients | Assist in initial assessment, provide ongoing care |
| Respiratory Therapists | Manage ventilators, respiratory care | Assist in managing ventilation during initial resuscitation |
Understanding these teams shows the teamwork needed in both fields. It’s all about working together for the best care.
Career Trajectories and Professional Opportunities
Surgeons in surgical critical care and trauma surgery have many career paths. They can work in academics or directly with patients. As healthcare changes, these surgeons face new challenges and chances to grow.
Academic vs. Clinical Paths
Surgeons can choose between academic and clinical careers. Academic roles involve research, teaching, and helping develop new medical practices. Clinical paths focus on patient care and using current medical knowledge.
Academic careers let surgeons do research, publish papers, and speak at conferences. They also teach and mentor future doctors.
Clinical careers offer rewards like directly helping patients and working with other healthcare teams. These roles can be in hospitals or private practices.
Evolving Roles in Healthcare Systems
Healthcare systems are changing, bringing both challenges and opportunities for surgeons. Policy changes, new technologies, and patient needs shape their roles.
Surgeons must keep up with medical research and technology. They also help shape healthcare policies and practices in their workplaces.
By knowing the different career paths and how healthcare is evolving, surgeons can make smart choices. They can also make a big impact in their field.
Future Trends: How Both Fields Are Evolving
Looking ahead, surgical critical care and trauma surgery are set for big changes. New technologies and training methods will shape these fields. These updates will bring new ways to care for patients.
Technological Advancements
New tech is changing surgical critical care and trauma surgery. Advanced monitoring systems and artificial intelligence (AI) are making ICUs better. AI quickly sorts through data, helping doctors make better choices.
Telemedicine is also growing, letting experts help from afar. This makes care more accessible. Plus, minimally invasive surgery cuts down recovery times and boosts success rates for trauma patients.
Changing Training Models
Training for surgeons is changing too. Simulation-based training lets surgeons practice in a safe space. This method improves skills and lowers the chance of mistakes.
There’s also more focus on interdisciplinary training. Surgeons, nurses, and others learn together. This teamwork is key in the fast-paced world of surgical critical care and trauma surgery.
These new training methods will help surgeons become more skilled. They’ll be ready for the challenges of today’s surgery.
Conclusion: Distinct Yet Complementary Specialties
We’ve looked into the roles of surgical critical care and trauma surgery. These specialties work together for critically ill patients. Surgical critical care manages the care of these patients. Trauma surgery focuses on the immediate care of injured patients.
There’s a clear overlap between these specialties. They share the goal of giving the best care possible. Trauma surgeons and surgical intensivists work together for a smooth care process.
These specialties form a key part of patient care. They start with the first steps in trauma surgery and continue in surgical critical care. This teamwork helps healthcare providers give top-notch care to patients with complex needs.
Understanding the unique yet connected roles of surgical critical care and trauma surgery shows the importance of teamwork. This approach helps improve patient outcomes.
FAQ
What is the primary difference between surgical critical care and trauma surgery?
Surgical critical care deals with life-threatening conditions in surgical patients. Trauma surgery focuses on emergency surgeries for injuries.
What kind of training is required for surgeons to specialize in surgical critical care or trauma surgery?
Surgeons need a surgical residency first. Then, they get fellowship training in either field.
How do the day-to-day responsibilities of surgical critical care specialists and trauma surgeons differ?
Critical care specialists manage ICU patients. Trauma surgeons handle emergency surgeries and initial patient checks.
What is the role of surgical critical care in managing sepsis and organ failure?
Specialists in surgical critical care are key in treating sepsis and organ failure. They use advanced treatments and life-support systems.
What is acute care surgery, and how does it relate to trauma surgery and surgical critical care?
Acute care surgery combines trauma and critical care. It focuses on emergency surgeries and care for critically ill patients.
What are the typical procedural skills required for surgical critical care specialists?
Specialists are trained in procedures like central line placement and ventilator management. These help critically ill patients.
How do trauma centers operate, and what roles do surgical critical care and trauma surgery play within these systems?
Trauma centers have different levels (I-V) based on their capabilities. Surgical critical care and trauma surgery are crucial in patient care, from start to recovery.
What is the importance of post-operative care in surgical patients, and how does surgical critical care contribute to this phase?
Post-operative care is key to prevent complications and ensure recovery. Surgical critical care specialists are vital in managing patients after surgery, providing close monitoring and support.
What are the certification and credentialing requirements for surgical critical care and trauma surgery specialists?
Board certification in surgical critical care is through fellowship programs and exams. Trauma surgery qualifications involve additional training and experience.
How do multidisciplinary teams function in surgical ICU and trauma settings?
Teams in surgical ICU and trauma settings include surgeons, intensivists, nurses, and more. They work together to care for critically ill patients.
What career trajectories are available to surgeons specializing in surgical critical care or trauma surgery?
Surgeons can choose academic or clinical paths. They can lead, research, teach, or work in administration and policy.
How are technological advancements influencing the practice of surgical critical care and trauma surgery?
New technologies, like better monitoring and minimally invasive surgery, improve care and outcomes in both fields.
What changes are occurring in training models for surgical critical care and trauma surgery?
Training is evolving with new technologies, simulation, and competency-based assessments. This prepares surgeons for these specialties better.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6407564/