The Canadian Cancer Society says a stem cell transplant might be used for kids with leukemia. This is when a child’s stem cells or bone marrow get leukemia.
This treatment replaces the damaged stem cells. It could save a child’s life. Knowing about stem cell transplants in pediatric leukemia treatment helps families a lot.
Key Takeaways
- Stem cell transplants are a treatment option for childhood leukemia.
- Damaged stem cells or bone marrow can be replaced through this process.
- Understanding the treatment options is vital for families.
- The role of stem cell transplants in pediatric leukemia treatment is significant.
- Families should be aware of the possible benefits and risks.
Understanding Pediatric Leukemia

It’s important to understand pediatric leukemia to treat it well. This cancer affects the blood and bone marrow. It’s caused by abnormal white blood cells growing too much. It’s the top cancer in kids, with two main types.
Types of Childhood Leukemia: ALL and AML
Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML) are the main types in kids. ALL is the most common, making up 80% of cases. AML is more aggressive and needs strong treatment.
Knowing the difference between these types is key for the right treatment.
Standard Pediatric Oncology Care Approaches
Pediatric oncology care for leukemia is all-inclusive. It includes chemotherapy, targeted therapy, and supportive care. Treatments are based on the leukemia type and risk.
Risk stratification helps make treatment fit each child’s needs. This way, treatment is not too little or too much. Thanks to pediatric oncology care advances, more kids are surviving leukemia.
The Role of Bone Marrow Transplants in Leukemia Treatment
Bone marrow transplants are key for kids with leukemia. They replace bad bone marrow with good cells. This could be a cure for the disease.
What is a Bone Marrow Transplant?
A bone marrow transplant replaces bad bone marrow with good. Healthy stem cells are given to the body. These cells then make healthy blood cells.
How Transplants Work Against Leukemia
Transplants fight leukemia by first killing bad cells with chemo or radiation. Then, healthy stem cells are given. These cells help rebuild the bone marrow and immune system. This can cure leukemia by getting rid of cancer cells.
Difference Between Bone Marrow and Stem Cell Transplant for Kids
Bone marrow and stem cell transplants are not the same. Bone marrow transplants use bone marrow cells. Stem cell transplants use stem cells from bone marrow, blood, or umbilical cord. For kids, stem cell transplants are more common and flexible.
Key aspects of bone marrow transplants for leukemia:
- Replacing diseased bone marrow with healthy cells
- Using chemotherapy or radiation to destroy cancerous cells
- Introducing healthy stem cells to rebuild the bone marrow and immune system
- Differences between bone marrow and stem cell transplants
The American Cancer Society says a stem cell transplant (SCT) can cure childhood leukemia. It replaces the blood-forming stem cells and immune system in the bone marrow.
When is a Bone Marrow Transplant Necessary?
To know if a bone marrow transplant is needed for kids with leukemia, we look at how severe the disease is and how well it responds to first treatments. This transplant is considered when the leukemia is at high risk or has come back.
High-Risk Leukemia Indicators
Some kids with leukemia may need a bone marrow transplant. This is true for those with certain genetic problems, very high white blood cell counts at the start, or if they don’t do well with first chemotherapy. The Canadian Cancer Society says stem cell transplants are often used for AML because it tends to come back more than ALL.
Key high-risk factors include:
- Genetic mutations such as MLL gene rearrangements
- Poor response to initial induction chemotherapy
- High minimal residual disease (MRD) levels after treatment
Relapse Treatment in Children
Relapse is a big worry in kids with leukemia, and treatment choices are often few. A bone marrow transplant can be a good option for kids who have relapsed, mainly if it happens after first chemotherapy.
“For children with relapsed or refractory leukemia, a bone marrow transplant offers a second chance at remission and potentially a cure.”
Treatment-Resistant Cases
When leukemia doesn’t respond to usual treatments, a bone marrow transplant might be an option. This is true for kids with AML, which is harder to treat with chemotherapy than ALL.
| Leukemia Type | Relapse Rate | Transplant Consideration |
| ALL | Lower | Less common |
| AML | Higher | More common |
Understanding these points helps doctors decide when a bone marrow transplant is needed for kids with leukemia. This gives them the best shot at successful treatment and remission.
Types of Bone Marrow Transplants for Pediatric Leukemia
Bone marrow transplants are a key treatment for kids with leukemia. Knowing the different types is important. The type chosen can greatly affect the outcome.
Autologous Transplants
Autologous transplants use the patient’s own stem cells. This method is less common for leukemia because it risks bringing back cancer. Yet, it might be an option if the patient’s bone marrow is healthy.
Allogeneic Transplants
Allogeneic transplants use stem cells from another person. They are often used for kids with leukemia. The American Cancer Society calls this an allogeneic SCT.
Related Donors
Related donors are family members who match the patient. Siblings are usually the best match because they share similar genes.
Unrelated Donors
Unrelated donors are people who aren’t related but match. Registries like the National Marrow Donor Program help find these donors.
Haploidentical Transplants
Haploidentical transplants use donors who are half-matched, often a parent. This method is becoming more popular. It offers hope to patients without a fully matched donor.
The Donor Match Leukemia Process
Finding a donor match for leukemia involves several steps. This includes HLA testing and searching for donors. For kids with leukemia, a bone marrow transplant can save their life. But, it needs a donor who is a good match.
HLA Testing for Kids
HLA testing is key to finding a compatible donor. The Canadian Cancer Society says donors and recipients are matched through HLA typing. This test looks at the unique markers on white blood cells, important for the immune system.
By comparing these markers, doctors can see if a transplant will likely work.
Donor Search Process: Family Members vs. Registries
The donor search process looks at both family members and registries. First, doctors test family members like parents and siblings to see if they match. If no family member is a match, the search goes to unrelated donors in registries like the National Marrow Donor Program (NMDP).
This search can take a long time. But, it’s very important to find the right donor.
Challenges in Donor Matching for Diverse Populations
Finding a donor match is harder for patients from diverse ethnic backgrounds. Different ethnic groups have different HLA markers. This makes it tough to find a match for patients with mixed or less common ethnicities.
There are ongoing efforts to make donor registries more diverse. This aims to increase the chances of finding a match for all patients.
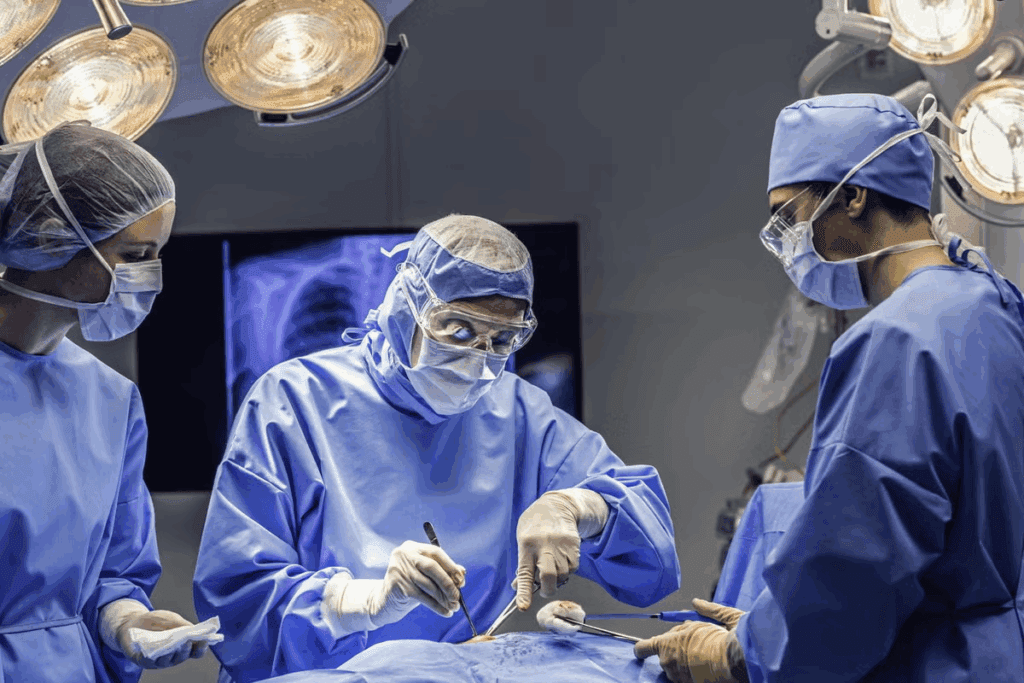
Bone Marrow Transplant Leukemia: The Procedure
A bone marrow transplant is a lifesaving treatment for many children with leukemia. It involves careful preparation and execution. The process is complex and requires a detailed approach to ensure the best outcomes.
Pre-Transplant Evaluation and Preparation
Children with leukemia must undergo a thorough evaluation before the transplant. This evaluation assesses their overall health and suitability for the transplant. It includes tests to check organ function, infection status, and any other health issues.
Conditioning Regimens: Chemotherapy and Transplant
The American Cancer Society explains that before a stem cell transplant, high-dose chemotherapy is used. It destroys the bone marrow and leukemia cells. Then, healthy stem cells are infused into the body. This conditioning regimen is key to eradicating cancer cells and preparing the body for the new stem cells.
Conditioning Regimen Components
| Treatment | Purpose |
| High-dose Chemotherapy | Destroy leukemia cells and bone marrow |
| Stem Cell Infusion | Replace damaged marrow with healthy stem cells |
The Transplant Process
The transplant process involves infusing healthy stem cells into the patient’s bloodstream. These stem cells migrate to the bone marrow and start producing new blood cells.
“The success of a bone marrow transplant depends on various factors, including the patient’s overall health, the match quality of the donor, and the effectiveness of the conditioning regimen.”
Immediate Post-Transplant Care
After the transplant, patients need close monitoring for complications. These include graft-versus-host disease (GVHD), infection, or graft failure. Immediate post-transplant care involves a team of healthcare professionals. They work together to manage these risks and ensure a smooth recovery.
Risks and Complications of Pediatric Bone Marrow Transplants
Children getting bone marrow transplants face many risks and complications. Experts say treatment can cause side effects. Some are minor, but others can be serious or even life-threatening.
Short-Term Complications
Short-term issues can happen during or right after the transplant. These include infections, bleeding, and reactions to the treatment. It’s important to watch closely and provide supportive care during this time.
Graft-Versus-Host Disease Management
Graft-versus-host disease (GVHD) is a big problem. It happens when the donated marrow or stem cells attack the child’s body. To manage GVHD, doctors use immunosuppressive medications and keep a close eye on the child.
Long-Term Effects on Growth and Development
Long-term effects can affect a child’s growth and development. Problems like growth hormone deficiency and thyroid issues can occur. It’s key to have ongoing care to handle these issues.
Immune Recovery in Kids Post-Transplant
After the transplant, immune recovery is very important. Kids may be more prone to infections because their immune system is weak. To help, doctors use growth factors and antibiotics to prevent infections.
| Complication | Description | Management Strategies |
| Graft-Versus-Host Disease | Donated cells attack the recipient’s body | Immunosuppressive medications, monitoring |
| Infections | Bacterial, viral, or fungal infections post-transplant | Prophylactic antibiotics, isolation techniques |
| Growth and Development Issues | Hormonal deficiencies, developmental delays | Hormone replacement therapy, developmental support |
Transplant Success Rate for Kids and Long-Term Outcomes
Bone marrow transplants are a key treatment for kids with leukemia. They offer hope for a long life. The success of these transplants depends on many factors. It’s important for families and doctors to understand these.
Factors Affecting Leukemia Remission Treatment Success
The success of leukemia treatment in kids depends on several things. These include the type of leukemia, the stage at diagnosis, and the patient’s health. The American Cancer Society says the transplant’s success also depends on the donor and recipient’s match.
Survival Statistics by Leukemia Type
Survival rates for kids with leukemia differ by type. For example, kids with Acute Lymphoblastic Leukemia (ALL) have a better chance of survival. The American Cancer Society has detailed survival rates for each type of leukemia.
| Leukemia Type | 5-Year Survival Rate |
| ALL | 90% |
| AML | 65-70% |
Pediatric Cancer Recovery and Quality of Life After Transplant
Recovery from a bone marrow transplant for kids with cancer is a long journey. It’s not just about the immediate time after the transplant. It also includes long-term care. The quality of life for these kids can be affected by several factors.
Doctors closely watch the long-term outcomes of kids who have had bone marrow transplants. They work hard to prevent complications and improve their quality of life.
Alternative and Complementary Treatments
Children with leukemia might find help in new treatments. These options aim to make treatment better and safer. They help kids live better lives and sometimes offer new ways to fight the disease.
Advanced AML Pediatric Therapy Protocols
Advanced AML therapy for kids includes strong chemotherapy and sometimes a bone marrow transplant. These plans are made to help kids live longer. They are based on the leukemia’s genetic makeup.
CAR T Therapy as an Alternative
CAR T-cell therapy is a new way to fight leukemia. It uses the body’s immune system to attack cancer cells. This method can be more effective than old treatments for some kids.
Targeted Therapy for Children with Specific Leukemia Types
Targeted therapy uses drugs to attack specific parts of leukemia cells. Doctors say it’s used for some leukemia types. It’s a more focused way to treat the disease.
These new treatments give kids with leukemia new hope. They offer better and safer ways to fight the disease.
Conclusion: Supporting Families Through the Transplant Journey
Going through a bone marrow transplant for pediatric leukemia is tough for families. The Canadian Cancer Society stresses the need for full support during this time. Knowing how bone marrow transplants work in treating leukemia is key for making smart choices about care.
Helping families means more than just medical care. It’s also about emotional and mental support. The transplant process, from start to finish, needs a team effort to treat pediatric leukemia well. With the right resources and support, families can handle the tough parts better.
The main aim of treating pediatric leukemia is to get the child better and improve their life quality. By grasping the transplant process and having the right support, families can get through it more smoothly.
FAQ
What is the role of bone marrow transplants in pediatric leukemia treatment?
Bone marrow transplants are key in treating pediatric leukemia. They are most important for kids with high-risk or relapsed leukemia. The transplant replaces damaged bone marrow with healthy cells, aiming for remission.
How is a donor match found for a bone marrow transplant?
Donor matching starts with HLA testing to find compatible donors. The search can include family members or unrelated donors from registries. A good match is vital for transplant success.
What are the different types of bone marrow transplants available for pediatric leukemia?
There are three main types of bone marrow transplants. Autologous uses the child’s own cells, allogeneic uses a donor’s cells, and haploidentical uses a partially matched family member’s cells. Each type has its own benefits and risks.
What are the different types of bone marrow transplants available for pediatric leukemia?
There are three main types of bone marrow transplants. Autologous uses the child’s own cells, allogeneic uses a donor’s cells, and haploidentical uses a partially matched family member’s cells. Each type has its own benefits and risks.
References
Identifying the typical minimum age and discussing the role of Bone marrow transplant leukemia treatment.
https://pubmed.ncbi.nlm.nih.gov/8932789/