Keeping blood sugar levels in check is a big job. It involves more than just what we eat. At Liv Hospital, we believe in teaching our patients everything they need to know to keep their glucose levels healthy. Learn the crucial link between dehydration and blood sugar. Discover 7 hidden things that can cause unexpected glucose spikes quickly.
Some things can make blood sugar go up without us even noticing. It’s important to know what these are. We know that it’s not just about food; stress and some medicines can also affect it.
By tackling these issues, people can take better care of their health. We’ll look at what can make blood sugar levels rise. We aim to help you keep your levels in a healthy range.
Key Takeaways
- Many things other than food can affect blood sugar levels.
- Dehydration and stress are big reasons for blood sugar spikes.
- Knowing what affects you personally is key to managing blood sugar.
- Teaching patients everything they need to know is important for healthy glucose levels.
- Everyday things, like some medicines, can also change blood sugar levels.
The Complex Nature of Blood Sugar Regulation

Blood sugar regulation is a complex process. It involves many physiological mechanisms working together. This ensures our bodies have a steady supply of energy and prevents damage from too much glucose.
How Your Body Normally Manages Glucose Levels
Our bodies manage glucose levels through a balance of insulin production and sensitivity. When we eat carbs, they turn into glucose that enters our bloodstream. The pancreas then releases insulin to help cells absorb glucose.
This balance keeps our blood sugar levels healthy. The liver, kidneys, and cells’ sensitivity to insulin all play a role. When these work well, they help keep our blood sugar stable.
Why Blood Sugar Stability Matters for Overall Health
Stable blood sugar levels are key for our health. Fluctuations can cause fatigue, dizziness, and confusion. Long-term, high blood sugar can lead to serious problems like nerve damage and heart disease.
Stable blood sugar also helps our metabolism. It lowers the risk of type 2 diabetes and metabolic syndrome. Knowing what affects blood glucose helps us stay healthy.
Common Misconceptions About Blood Sugar Fluctuations
Many think only sugary foods raise blood sugar. But dehydration, stress, and some medications can also affect it. It’s also wrong to think blood sugar spikes only worry people with diabetes.
Actually, blood sugar rises are normal for everyone. Understanding this can help us manage our health better. Dehydration, for example, can make glucose levels spike because it reduces blood volume.
Dehydration and Blood Sugar: The Hidden Connection

Dehydration and blood sugar levels are closely linked, yet often overlooked. It’s key for managing glucose levels. Dehydration can affect how our bodies regulate blood sugar, leading to serious health issues if not managed well.
The Concentration Effect: How Water Loss Affects Glucose Readings
When we lose water, our blood glucose concentration goes up. This is because there’s less fluid in our bodies. So, even if glucose levels don’t change, our readings can appear higher due to dehydration.
For instance, dehydration can make our bodies produce less insulin. It also causes our liver to release stored glucose into the bloodstream. This makes managing blood sugar even harder.
Research Evidence on Dehydration and Hyperglycemia
Studies have found a strong link between dehydration and high blood sugar. They show that not drinking enough water can lead to hyperglycemia. This highlights the need for enough hydration to keep blood sugar stable.
Hydration Status | Average Blood Glucose (mg/dL) | Hyperglycemia Incidence (%) |
Adequately Hydrated | 120 | 15 |
Mildly Dehydrated | 140 | 25 |
Severely Dehydrated | 180 | 40 |
How Much Water You Need to Maintain Stable Blood Sugar
How much water do you need for stable blood sugar? The answer varies by person. Generally, aim for eight glasses a day. But, this can change based on your climate, activity level, and health.
Key factors to consider:
- Climate: Hot and humid places need more water.
- Physical Activity: More water is needed with more activity.
- Overall Health: Some health issues can affect how much water you need.
Psychological Stress: The Cortisol-Glucose Relationship
When we feel stressed, our body goes into “fight or flight” mode. This releases hormones that make our blood sugar levels go up. This is meant to be a quick fix to deal with threats. But, with chronic stress, we stay in this high blood sugar state for too long.
How Stress Hormones Trigger Blood Sugar Spikes
Cortisol, known as the “stress hormone,” is key in our stress response. It tells the liver to release glucose into the blood, causing a spike. This gives us quick energy to face the stress.
Cortisol’s Role: Cortisol not only raises blood sugar but also helps store fat, mainly in the belly. This makes it harder for glucose to be used by the body.
Acute vs. Chronic Stress Effects on Insulin Sensitivity
Acute stress can make it harder for glucose to get into cells. This is usually okay for healthy people. But, for those with diabetes or prediabetes, it can cause big blood sugar spikes.
Chronic stress, though, can lead to long-term insulin resistance. This is a big risk for type 2 diabetes. The constant presence of cortisol and other stress hormones messes with insulin signals.
“Chronic stress can have a profound impact on glucose metabolism, leading to insulin resistance and increasing the risk of developing type 2 diabetes.”
Dr. Elizabeth R. Marino, Endocrinologist
Measuring the Impact of Stress on Your Blood Sugar
To see how stress affects your blood sugar, track your stress and glucose levels. Mindfulness, meditation, and exercise can help reduce stress’s impact on blood sugar.
- Keep a stress diary to track when you feel stressed and how it correlates with your blood sugar levels.
- Use a continuous glucose monitor (CGM) to get detailed insights into your glucose fluctuations.
- Practice stress-reducing techniques, such as yoga or deep breathing exercises.
Understanding the link between stress and blood sugar helps us manage our glucose better. This improves our health and well-being.
Physical Pain and Inflammatory Responses
Pain makes our body’s stress response kick in, which can raise blood sugar levels. This link between pain, inflammation, and glucose is key to managing blood sugar well.
The Science Behind Pain-Induced Blood Sugar Elevation
Pain releases stress hormones like cortisol and adrenaline. These hormones get our body ready to fight or flee, raising blood glucose. This helps us deal with threats quickly. But, long-term pain can keep these hormones high, hurting blood sugar control.
Key Players in Pain-Induced Blood Sugar Elevation:
- Cortisol: Known as the “stress hormone,” it helps release glucose from stored energy.
- Adrenaline: This hormone also breaks down glycogen to glucose, raising blood sugar.
- Inflammatory Cytokines: Pain and inflammation release cytokines. These can mess with insulin signaling, making it hard for glucose to get into cells.
Inflammatory Pathways That Disrupt Glucose Metabolism
Inflammation is a natural response to injury or infection. But, long-term inflammation can harm glucose metabolism. It can cause insulin resistance, where cells don’t respond well to insulin, leading to high blood sugar.
Inflammatory Marker | Effect on Glucose Metabolism | Potential Outcome |
C-reactive Protein (CRP) | Increased insulin resistance | Elevated blood sugar levels |
Interleukin-6 (IL-6) | Disrupted insulin signaling | Impaired glucose uptake in cells |
Tumor Necrosis Factor-alpha (TNF-alpha) | Inhibition of insulin receptor substrate | Increased glucose production in the liver |
For example, a sunburn can cause pain, leading to higher stress hormones and blood sugar. It’s important to manage these conditions well to keep blood sugar stable.
Managing Pain to Prevent Blood Sugar Fluctuations
Managing pain well is key to avoiding blood sugar swings. This can include medical treatments, lifestyle changes, and alternative therapies.
Strategies for Managing Pain and Blood Sugar:
- Check your blood sugar often, when you’re in pain.
- Work with your doctor to adjust your treatment plan as needed.
- Try stress-reducing activities like meditation or deep breathing.
- Do regular physical activity that fits your health.
- Eat a balanced diet that helps with pain and glucose control.
Understanding the link between pain, inflammation, and blood sugar helps us manage these factors better. This improves our overall health and well-being.
Problematic Foods That Cause Unexpected Insulin Spikes
Knowing which foods cause insulin spikes is key to controlling blood sugar. Carbohydrates have the biggest impact on blood sugar. But, not all carbs are the same, and some can lead to sudden insulin spikes.
Hidden Carbohydrates in “Healthy” Foods
Even “healthy” foods can have hidden carbs that raise blood sugar. Fruits like bananas and mangoes have natural sugars. Starchy veggies like potatoes and corn also cause blood sugar spikes. Some whole grain products, like certain bread and cereals, are high in carbs too.
To keep blood sugar in check, it’s important to read labels. We should also watch portion sizes to avoid too many carbs.
The Glycemic Index vs. Glycemic Load Explained
The glycemic index (GI) shows how fast foods raise blood sugar. Foods are ranked from 0 to 100, with higher numbers meaning quicker blood glucose increases. But, GI doesn’t consider serving size.
The glycemic load (GL) looks at GI and carb amount in a serving. This gives a clearer picture of a food’s blood sugar impact. For example, watermelon has a high GI but a low GL because it has little carb per serving.
Food Combinations That Amplify Blood Sugar Response
How we mix foods affects our blood sugar. Eating carbs with proteins and fats slows down glucose digestion and absorption. This reduces insulin spikes. For example, whole grain toast with avocado and eggs is better than toast alone.
But, mixing high-carb foods with high-GI foods can worsen blood sugar spikes. Being aware of these combinations helps manage blood sugar better.
Medications That Affect Blood Glucose Levels
Many people don’t know that some medicines can change their blood sugar levels. It’s key to manage blood sugar for health. But, it’s also important to know how different medicines can affect how our body uses glucose.
“Some medicines can make blood sugar go up, even if you don’t have diabetes,” says Dr. Emily Chen, an endocrinologist. “Knowing this can help you keep your blood sugar in check.”
Common Prescription Drugs That Raise Blood Sugar
Many types of prescription medicines can make blood sugar go up. These include:
- Corticosteroids: Used to fight inflammation, like prednisone, can really raise blood sugar.
- Certain Psychiatric Medications: Some medicines for mental health, like clozapine and olanzapine, can make it harder for insulin to work.
- Beta-Blockers: Important for heart health, but some can mess with how the body uses insulin.
- Thiazide Diuretics: Help with high blood pressure, but can sometimes raise blood sugar too.
Over-the-Counter Medications and Their Glucose Effects
It’s not just prescription drugs that can change blood sugar. Some over-the-counter (OTC) medicines can too:
- Decongestants: Pseudoephedrine in cold medicines can raise blood sugar.
- Certain Supplements: Supplements like niacin, for cholesterol, can also affect how we use glucose.
Talk to your doctor before stopping any medicine. They can help you understand how it affects your blood sugar and adjust your treatment.
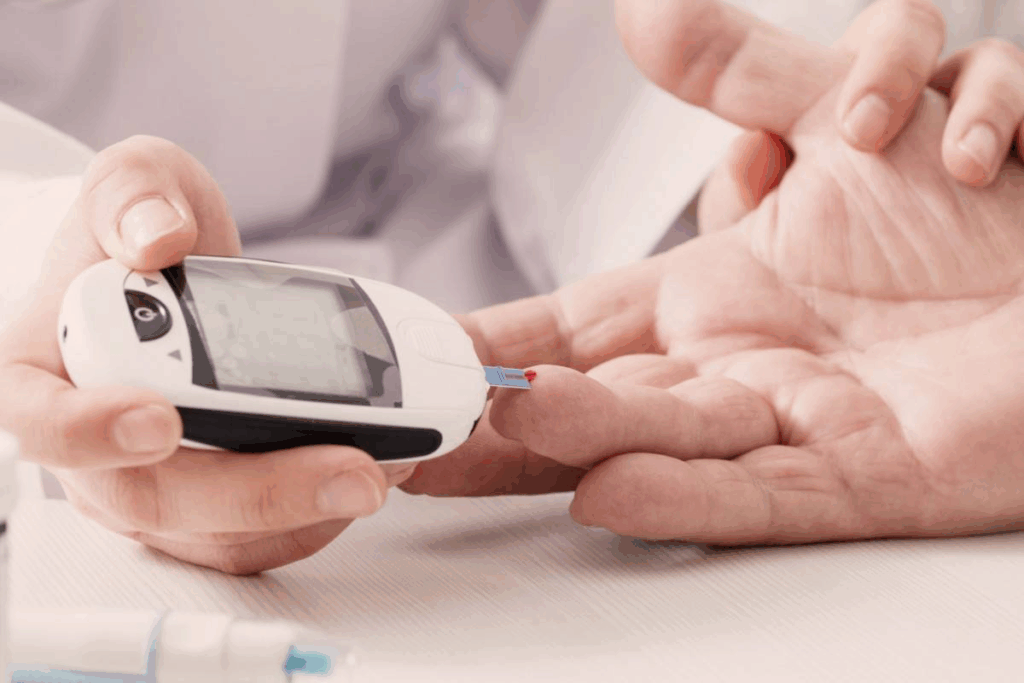
Working With Your Doctor to Minimize Medication-Induced Spikes
If your medicines affect your blood sugar, working with your doctor is key. Here’s what you can do:
- Monitor Your Blood Sugar: Keep an eye on your blood sugar to spot any changes.
- Communicate with Your Doctor: Tell your doctor about any changes in your medicine or blood sugar.
- Adjust Your Treatment Plan: Your doctor might need to change your diabetes plan or medicines to avoid blood sugar spikes.
Being proactive and informed can help you manage how medicines affect your blood sugar.
Sleep Deprivation and Disrupted Circadian Rhythms
Sleep is key to our health, and not getting enough can mess with how our body handles sugar. It affects our glucose metabolism in many ways. When we don’t sleep well, our body’s health can suffer.
Impaired Glucose Tolerance Due to Poor Sleep Quality
Poor sleep makes it tough for our body to control blood sugar. Studies show that not sleeping well can cause blood sugar to swing wildly. It also makes our body less responsive to insulin.
“Sleep deprivation affects glucose tolerance by altering the body’s insulin sensitivity.” This is a big worry for people with diabetes or those at risk of getting it.
The Connection Between Sleep Duration and Insulin Resistance
How long we sleep affects how well our body uses insulin. Not sleeping enough can make our body’s cells less responsive to insulin. This leads to high blood sugar levels. People who sleep well tend to have better insulin sensitivity.
“The relationship between sleep duration and insulin sensitivity is well-established, with shorter sleep durations associated with reduced insulin sensitivity.”
Shift Work and Its Impact on Blood Sugar Regulation
Shift work messes with our body’s natural rhythm and can affect blood sugar. Workers with odd schedules might see blood sugar levels go up and down. This can raise the risk of getting metabolic disorders like type 2 diabetes.
To fight the effects of shift work on blood sugar, it’s important to stick to a regular sleep schedule. Also, living a healthy lifestyle helps a lot.
Hormonal Fluctuations Beyond Insulin
Other hormonal changes can also affect blood sugar levels. Insulin is key for glucose control, but other hormones help keep blood sugar stable too.
Menstrual Cycle Phases and Blood Sugar Variability
The menstrual cycle can change blood glucose levels for many women. Hormonal shifts, like changes in estrogen and progesterone, can make insulin work less well. This can lead to higher blood sugar levels, mainly in the luteal phase after ovulation.
Thyroid Hormone Imbalances and Glucose Metabolism
The thyroid gland is important for metabolism, including glucose. Both too much and too little thyroid hormone can affect blood sugar. Too much can make the liver produce more glucose, raising blood sugar. Too little can slow down glucose use.
Growth Hormone and Cortisol: The Nighttime Blood Sugar Effect
Growth hormone and cortisol, or stress hormones, can greatly impact blood sugar, mainly at night. Growth hormone spikes during deep sleep can make insulin less effective, raising morning blood sugar. Cortisol, which follows a daily cycle, can also affect glucose use, more so if stress levels are high.
Effective Strategies to Prevent and Manage Blood Sugar Spikes
To keep blood sugar levels stable, it’s important to use a few key strategies. These include staying hydrated, managing stress, making dietary changes, and being active. By doing these things, you can keep your blood sugar levels steady and improve your health.
Hydration Guidelines for Optimal Glucose Control
Drinking enough water is key to keeping blood sugar levels stable. Dehydration can make blood sugar levels go up, leading to spikes. It’s best to drink at least eight glasses of water a day, but this can vary based on how active you are and your personal needs.
A study found that even a little dehydration can raise blood sugar levels a lot.
“Adequate hydration is essential for glucose regulation and overall metabolic health.”
Stress Reduction Practices That Improve Insulin Sensitivity
Stress can raise blood sugar levels by releasing stress hormones like cortisol. Practices like meditation, yoga, or deep breathing can help lower stress and improve insulin sensitivity. This helps manage blood sugar spikes.
- Meditation and mindfulness practices
- Yoga and tai chi
- Deep-breathing exercises
These activities not only reduce stress but also make your body more sensitive to insulin. This helps keep blood sugar levels stable.
Dietary Approaches for Stable Blood Sugar
Eating a balanced diet is essential for stable blood sugar levels. Choose whole, unprocessed foods like vegetables, fruits, whole grains, lean proteins, and healthy fats.
Food Group | Examples | Benefits |
Vegetables | Leafy greens, broccoli, bell peppers | Rich in fiber, vitamins, and minerals |
Fruits | Berries, citrus fruits, apples | High in antioxidants and fiber |
Physical Activity Timing for Maximum Glucose Benefit
Regular exercise is important for managing blood sugar levels. The timing of your workouts can also affect how well they lower blood sugar.
Doing physical activity after meals can help lower blood sugar spikes. Try a short walk or light exercise after eating for the best results.
Conclusion: Taking Control of Your Blood Sugar Through Awareness
Awareness is key to managing blood sugar levels effectively. By understanding the complex factors that influence glucose metabolism, individuals can take control of their blood sugar and improve their overall health.
Managing type 2 diabetes requires a holistic approach. This includes stress management, staying hydrated, and eating a balanced diet. By using effective strategies, like stress reduction and healthy eating, people can keep their blood sugar stable.
We’ve looked at factors that can raise blood sugar, like dehydration, stress, and some medications. Being aware of these and taking steps to prevent them can help keep blood sugar levels steady.
By knowing how to manage blood sugar and using practical strategies, we can help people take charge of their health. Effective blood sugar control is possible with awareness, lifestyle changes, and sometimes medical help.
FAQ
What spikes blood sugar levels?
Many things can make blood sugar levels go up. This includes dehydration, stress, certain foods, and some medicines. Sleep deprivation and hormonal changes also play a role.
Does dehydration affect blood sugar levels?
Yes, dehydration can make blood sugar levels higher. It does this by making the blood more concentrated with glucose.
Can stress increase glucose levels?
Yes, stress can make glucose levels go up. This happens because stress hormones like cortisol are released. These hormones can cause blood sugar spikes.
What foods cause insulin spikes?
Foods high in carbs, with a high glycemic index or glycemic load, can cause insulin spikes. Examples include refined grains and sugary drinks. Even some “healthy” foods with hidden carbs can have this effect.
Can pain raise blood sugar levels?
Yes, physical pain can increase blood sugar levels. This is because pain triggers inflammatory responses. These responses can disrupt how glucose is metabolized.
How much water is needed to maintain stable blood sugar levels?
The amount of water needed varies by person. But staying hydrated is key for controlling glucose levels.
Can certain medications affect blood glucose levels?
Yes, some medications can impact blood glucose levels. This includes prescription and over-the-counter drugs. It’s important to talk to your doctor to avoid spikes.
How does sleep deprivation impact blood sugar regulation?
Lack of sleep can harm how well glucose is tolerated. It can also increase insulin resistance. Both lead to blood sugar fluctuations.
Can hormonal fluctuations affect blood sugar levels?
Yes, changes in hormones can affect blood sugar levels. This includes menstrual cycle phases, thyroid hormone imbalances, and changes in growth hormone and cortisol levels.
What are effective strategies for preventing and managing blood sugar spikes?
To prevent and manage blood sugar spikes, stay hydrated and reduce stress. Eat a balanced diet and exercise regularly. Be mindful of your medication use and get enough sleep.
Reference
National Center for Biotechnology Information. Blood Sugar Spikes: Dehydration, Stress, and Other Factors. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28739050/