Researchers have made big strides in understanding embryonic stem cells. They can treat many medical conditions. Studies show these cells can help develop new treatments for serious diseases.
Parkinson’s disease and type 1 diabetes might be treated with embryonic stem cells. Parkinson’s affects millions and type 1 diabetes damages the pancreas. Regenerative medicine brings new hope to those suffering.
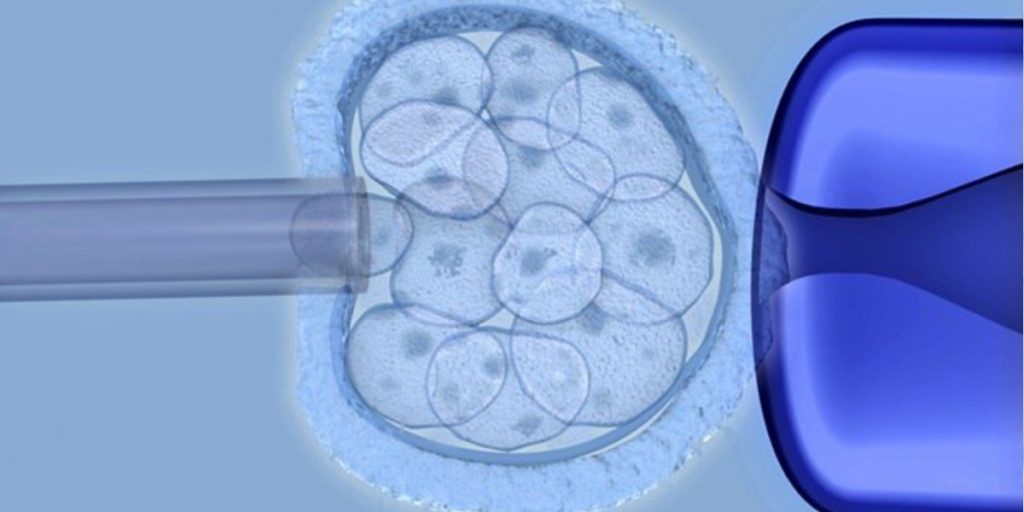
Embryonic stem cells can turn into any cell in the body. This makes them very useful for medical research and treatments.
These cells come from embryos and can grow and change into different cell types. They are pluripotent, which means they can become any type of body cell. This is why they’re so important for fixing damaged tissues.
These cells are special because of where they come from and what they can do. They’re taken from the inner part of an early embryo. Their pluripotency sets them apart from other stem cells.
Embryonic stem cells can become any cell type, including the three main layers of the body. This is key for fixing damaged tissues and treating diseases.
| Cell Type | Derived From | Potential Applications |
| Embryonic Stem Cells | Inner cell mass of blastocyst | Regenerative medicine, tissue repair |
| Adult Stem Cells | Various adult tissues | Tissue repair, limited differentiation |
| Induced Pluripotent Stem Cells | Reprogrammed adult cells | Regenerative medicine, personalized therapy |
These cells can grow into many types of cells. This means they could help with diseases like Parkinson’s, diabetes, and heart problems. Their ability to fix damaged tissues is a big plus for medical research.
Understanding the differences between embryonic stem cells and other types is key. Embryonic stem cells are special because they can turn into any cell in the body. This is called pluripotency.
Adult stem cells, or somatic stem cells, live in adult tissues. They can turn into different cell types, but not as many as embryonic stem cells. For example, bone marrow stem cells can make different blood cells but not cells from other tissues.
Another big difference is how many times they can divide. Embryonic stem cells can keep dividing forever in a lab. Adult stem cells can only divide a few times. This makes embryonic stem cells great for making lots of cells for therapy.
Induced pluripotent stem cells (iPSCs) are made from adult cells that are changed to be like embryonic stem cells. They can turn into any cell type, just like embryonic stem cells. But, they might remember where they came from, which could affect how they change into different cells.
iPSCs are special because they can come from a patient’s own cells. This lowers the chance of the body rejecting them. But, making iPSCs is hard and can cause genetic changes. This is a concern for using them in treatments.
In short, embryonic stem cells, adult stem cells, and iPSCs are all different. Embryonic stem cells are special because they can turn into any cell and keep dividing forever. Knowing these differences helps us move forward with stem cell treatments.
Stem cell therapy is a key part of regenerative medicine. It offers new ways to fix and grow tissues. This method uses stem cells’ special abilities to treat many health issues.
Cellular regeneration is a complex process. It involves stem cells turning into specific cells to fix damaged tissues. Stem cell therapy uses this to help tissues work right again.
The ways it works include:
Studies show stem cells can fix damaged tissues. They do this by releasing growth factors that help heal.
“The ability of stem cells to regenerate damaged tissues has opened new avenues for treating a range of diseases, from heart disease to neurological disorders.”
It’s important for transplanted stem cells to blend in with the host tissue. This means they move to the injury site and turn into the needed cells.
| Integration Process | Description |
| Cell Migration | Stem cells move to the injury site |
| Cell Differentiation | Stem cells turn into the needed cells |
| Tissue Integration | Transplanted cells blend with host tissue |
Good integration is key to fixing tissue function and getting good results.
Embryonic stem cell research has come a long way. It started in labs and now we see its use in treating diseases. This journey has brought us many discoveries and milestones.
In the 1960s, scientists found teratocarcinomas, tumors with many tissue types. This was the start of understanding stem cells’ power. In 1981, scientists first got embryonic stem cells from mouse embryos. This showed it was possible to grow these cells outside the body.
In 1998, James Thomson and his team made a big leap. They got human embryonic stem cells to grow in the lab. This opened doors for studying human development and finding new treatments.
Getting stem cell research from labs to treatments took time. Scientists had to do lots of tests to make sure these treatments were safe and worked. They faced many challenges, like making lots of stem cells and making sure they fit well in the body.
Now, we’re seeing the first steps in using stem cells to treat diseases like Parkinson’s and type 1 diabetes. These trials are checking if these treatments are safe and effective for people.
| Year | Milestone | Significance |
| 1960s | Discovery of teratocarcinomas | Understanding pluripotency |
| 1981 | Isolation of mouse embryonic stem cells | Demonstrated feasibility of culturing ESCs |
| 1998 | Isolation of human embryonic stem cells | Opened avenues for human developmental research |
Embryonic stem cell research has made huge strides. It’s moved from the lab to treating diseases. As we keep learning, the hope for these treatments grows.
Embryonic stem cells might change the game in treating Parkinson’s disease. This condition causes a loss of dopamine-producing neurons.
Parkinson’s disease mainly affects movement. It happens when dopamine-producing neurons in the brain’s substantia nigra are lost. This area is key for controlling movement.
The loss of dopamine causes symptoms like tremors, stiffness, and slow movement. Knowing how Parkinson’s works is key to finding good treatments.
Embryonic stem cells can turn into any cell type, including dopamine-producing neurons. This makes them a strong candidate for Parkinson’s treatment.

By using these stem cells to replace damaged neurons, researchers aim to boost dopamine levels. This could help reduce Parkinson’s symptoms.
Key Benefits of Embryonic Stem Cell Therapy for Parkinson’s Disease:
| Aspect | Current Treatment | Embryonic Stem Cell Therapy |
| Approach | Symptom management through medication and surgery | Replacement of damaged dopamine-producing neurons |
| Outcome | Temporary relief from symptoms | Potential long-term improvement in motor function |
| Limitation | Does not address underlying neuronal loss | Addresses the root cause by replacing lost neurons |
Scientists are working hard to grow new insulin-making beta cells for type 1 diabetes. This is done using embryonic stem cells. Type 1 diabetes happens when the body attacks and destroys these cells, forcing patients to take insulin shots for life.
Type 1 diabetes is when the body’s immune system mistakenly attacks the beta cells in the pancreas. This attack stops the body from making enough insulin. So, patients need to use insulin shots or pumps to keep their blood sugar levels right.
What starts this attack is not fully understood. But it’s thought that genes and the environment play a big part. Knowing how type 1 diabetes works is key to finding new treatments. These treatments aim to replace the lost beta cells and fix the immune system’s problem.
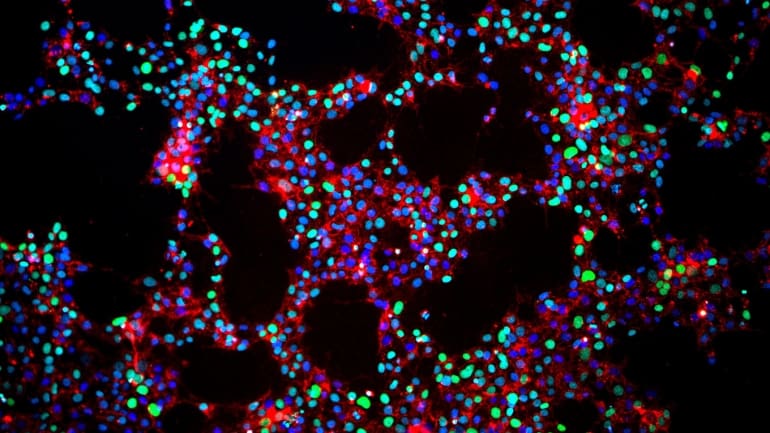
Embryonic stem cells are being looked at as a way to make new beta cells. They can turn into any cell type in the body. Scientists are trying to turn these stem cells into beta cells that can be given to people with type 1 diabetes.
There have been big steps forward in making these cells work right. Scientists have made insulin-producing cells that respond to sugar. These cells could help people with type 1 diabetes manage their blood sugar levels, maybe even curing the disease.
Creating these cells is a complex process. It starts with growing the stem cells, then turning them into pancreatic cells, and lastly into mature beta cells. Each step needs careful control to make sure the cells work as they should.
Comparison of Stem Cell Differentiation Protocols
| Protocol | Efficiency | Cell Maturity |
| Protocol A | 80% | High |
| Protocol B | 70% | Moderate |
| Protocol C | 90% | High |
The table shows how different protocols compare in making cells. Protocol C is the best, with the highest success rate and most mature cells. This makes it a strong candidate for use in treatments.
The journey of embryonic stem cell therapies from the lab to patients is long and detailed. It involves a lot of testing and getting approvals from regulators. This careful process is key to making sure these new treatments are safe and work well.
It all starts with a lot of research in the lab. Scientists do preclinical studies to learn about these cells. They find out how they work, how they can change into different types of cells, and if they are safe.
When the research looks promising, the therapy goes to clinical trials. These trials are done in phases, each with a specific goal:
One big challenge is making more cells while keeping them the same quality. Manufacturers have to make sure every batch of cells is the same in terms of what they are and how strong they are.
| Challenge | Description | Potential Solution |
| Cell Line Stability | Keeping cell lines stable over many uses | Using strong cell banking and quality control |
| Scalability | Producing more cells to meet demand | Creating bioreactors and large cell culture systems |
| Standardization | Making sure production is the same everywhere | Creating standard operating procedures (SOPs) |
Before these therapies can be sold, they need regulatory approval from places like the FDA in the U.S. They have to submit all the data from their lab and clinical trial work.
The approval process usually includes:
By understanding how embryonic stem cell therapies are developed, we see how complex and detailed the process is. It’s a journey that brings these new treatments to those who need them.
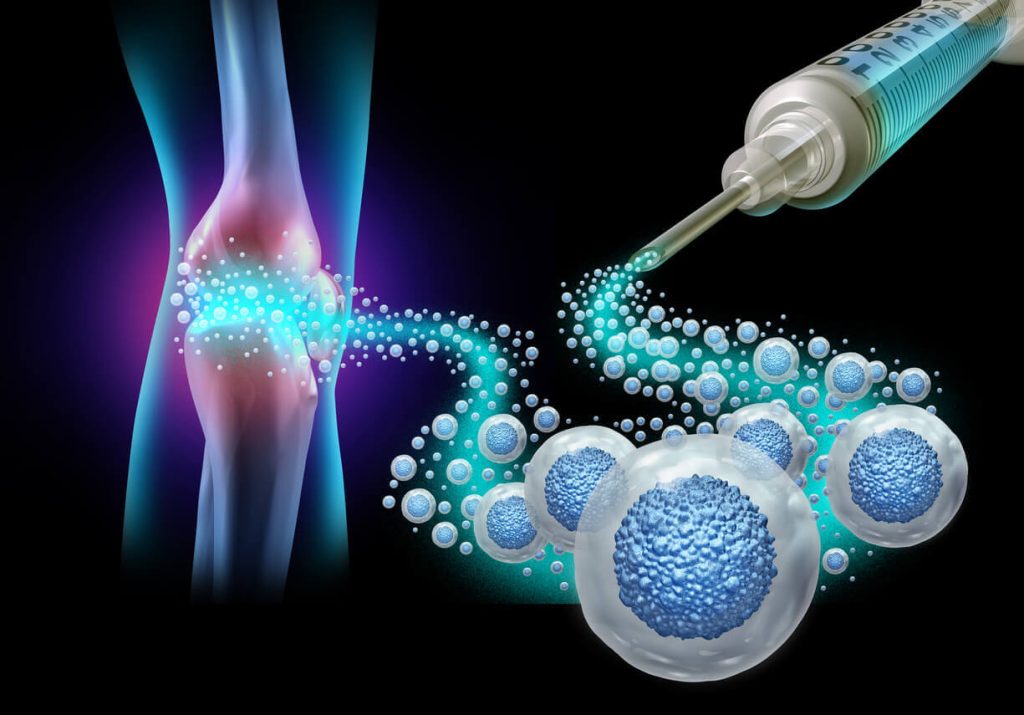
Stem cell therapy clinical trials are underway for many diseases. This includes Parkinson’s disease and type 1 diabetes. These trials help us understand if stem cell therapy is safe and works well. They bring us closer to new treatments for different health issues.
Parkinson’s disease is a main focus for stem cell therapy. Researchers are using embryonic stem cells to replace damaged brain cells. They are hopeful this could help symptoms and slow the disease.
Several trials are happening, using cell transplantation to put healthy cells in the brain. These studies check if the treatment is safe and works well over time.
Type 1 diabetes is also being studied with stem cell therapy. The goal is to make new insulin-producing cells. Embryonic stem cells might be able to turn into these cells.
Trials are looking at different ways to use stem cells, like transplanting them into patients. They are watching how patients react and making changes as needed.
Stem cell therapy trials are also looking at heart disease, spinal cord injuries, and other neurodegenerative disorders. Stem cells are versatile, giving hope for many health challenges.
As research goes on, more conditions will be studied. This could open up new treatment options. The results of these trials will guide the future of stem cell therapy.
Embryonic stem cells are showing great promise for fixing damaged hearts. They could be a game-changer in the fight against heart disease. This condition weakens the heart, often due to damage from heart attacks or other diseases.
Heart failure is tough to treat. Current methods mainly manage symptoms, not the root cause. It happens when the heart can’t pump enough blood, causing fatigue, swelling, and shortness of breath.
Key challenges include:
Embryonic stem cells might be the answer for fixing damaged hearts. They can turn into different cell types, including heart cells. This could replace damaged tissue and boost heart function.
Recent studies show these stem cell heart cells can blend into the host heart. This improves heart function in animal tests. But, there are hurdles to clear before they can help humans.
| Approach | Description | Potential Benefits |
| Cell Transplantation | Transplanting embryonic stem cell-derived cardiomyocytes into damaged heart tissue | Regeneration of heart tissue, improved cardiac function |
| Tissue Engineering | Using embryonic stem cells to engineer heart tissue for transplantation | Functional heart tissue replacement, improved cardiac function |
The field of using embryonic stem cells for heart repair is growing fast. Scientists are working hard to solve the technical and legal hurdles. This could lead to new treatments for heart disease.
Embryonic stem cells show great promise in treating many neurological disorders. They offer hope to patients and their families. Researchers are working hard to find new uses for these cells.
Spinal cord injuries can cause a lot of loss of function. Current treatments don’t work well. But, embryonic stem cells might change this.
These cells can turn into neural cells. Studies suggest they could fix damaged spinal cords. This could help animals and maybe humans too.
By transplanting these cells into injured areas, they might help the body heal. This is a new idea, but it could be very helpful. It could fix injuries that are currently permanent.
Multiple sclerosis attacks the central nervous system. It causes damage and loss of function. Embryonic stem cells might help by fixing this damage.
They could turn into cells that repair the damage. Scientists are studying how to use them for this purpose. This could be a big step forward in treating the disease.
| Condition | Current Treatment | Potential of Embryonic Stem Cells |
| Spinal Cord Injury | Limited rehabilitation options | Regeneration of damaged tissue |
| Multiple Sclerosis | Disease-modifying therapies | Remyelination and repair |
Other diseases like ALS and Huntington’s are also being looked at. Embryonic stem cells can become many types of neural cells. This makes them a great tool for fixing damaged brains.
Embryonic stem cell research brings up big ethical questions. These questions touch on moral, religious, and societal views. They are complex and need careful thought.
Using embryonic stem cells is a big debate because it means destroying human embryos. This is a big issue for many people. Different religions have different views, with some strongly against it and others seeing the benefits.
The moral status of the embryo is a key point in these debates. Some think an embryo is as valuable as a fully grown person. Others see its value as changing based on its development and use.
In the U.S., rules for embryonic stem cell research are tricky. They involve federal and state laws, plus guidelines from science and ethics groups. The Dickey-Wicker Amendment is a key law that stops federal money for research that destroys human embryos.
| Regulatory Body | Role in Embryonic Stem Cell Research |
| National Institutes of Health (NIH) | Provides funding for embryonic stem cell research under certain conditions. |
| Food and Drug Administration (FDA) | Oversees the approval of new therapies derived from embryonic stem cells. |
| State Governments | Some states have their own laws and regulations regarding embryonic stem cell research, which can be more permissive or restrictive than federal guidelines. |
One big challenge is balancing ethics with the hope for medical breakthroughs. Supporters say it could lead to big advances in disease treatment. Opponents stress the importance of respecting human embryos.
It’s important to keep talking among scientists, ethicists, policymakers, and the public. We need rules that are flexible for new science but also protect ethics.
Embryonic stem cell treatments offer hope for some medical conditions. But, getting these treatments can be hard. It depends on patient eligibility, clinical trial rules, and insurance.
Clinical trials for these treatments have strict rules. Patients must meet certain criteria. This includes the disease type and stage, overall health, and medical history.
For example, those with advanced Parkinson’s might qualify for trials. These trials use embryonic stem cells to make dopamine-producing cells.
Key factors influencing eligibility include:
Insurance for these treatments varies a lot. Some trials might be covered, while others aren’t. The high cost of treatments makes insurance very important.
Factors affecting insurance coverage include:
Where you live also affects access to these treatments. Trials and approved treatments are often in certain places. This can make it hard for patients in other areas.
Patients may need to consider:
It’s important for patients and healthcare providers to understand these factors. This helps them navigate the complex world of embryonic stem cell treatments.
Embryonic stem cell therapy is promising but faces big challenges. These include technical, safety, and immune issues. These obstacles make it hard to use these cells for treatment.
Producing high-quality embryonic stem cells on a large scale is tough. The process includes isolating cells, growing them, and changing them into specific types. Keeping the quality consistent is a big challenge.
Key technical challenges include:
| Technical Challenge | Description | Potential Solution |
| Cell Viability | Maintaining cell health during culture | Optimized culture media |
| Differentiation Consistency | Ensuring cells differentiate correctly | Standardized differentiation protocols |
| Scalability | Scaling up production without compromising quality | Bioreactor technology |
Safety is key in embryonic stem cell therapy. A big risk is tumor formation. Undifferentiated cells can grow into teratomas, which are tumors with different tissues.
“The risk of tumor formation is a major safety concern that must be addressed through rigorous preclinical testing and careful patient monitoring.” – Expert in Stem Cell Research
To lower this risk, researchers are working on:
Immune rejection is a big challenge in embryonic stem cell therapy. These cells may be seen as foreign by the immune system, leading to an immune response.
Ways to fight immune rejection include:
In conclusion, while embryonic stem cell therapy is promising, it’s important to tackle its challenges. Ongoing research aims to overcome these hurdles to fully use this therapy.
Scientists are looking into new ways to use stem cells because of the issues with embryonic stem cell therapy. These new methods aim to offer similar benefits without the ethical problems. They also try to solve practical challenges.
Induced pluripotent stem cells (iPSCs) are a big step forward in stem cell research. They turn adult cells, like skin or blood cells, into a pluripotent state. This means they can be made without using embryos, solving ethical issues.
Creating iPSCs involves adding special genes to adult cells. This makes them pluripotent. This technology is a big step towards personalized medicine. It lets doctors make cells that match a patient’s genes, reducing the chance of immune rejection.
Key benefits of iPSCs include:
Adult stem cells, also known as somatic stem cells, are another option. They are found in adult tissues and can turn into different cell types. But, they can’t turn into as many types as embryonic stem cells or iPSCs.
Adult stem cells are used in treatments for blood disorders and to repair tissues. They are good because they don’t often cause tumors. Also, using the patient’s own cells can reduce immune rejection problems.
Examples of adult stem cell applications include:
Gene therapy changes a patient’s cells to fight or prevent disease. When used with stem cells, it can make stem cells work better. It can fix genetic problems or give cells new functions.
Scientists are studying how to mix gene therapy with stem cells, like iPSCs and adult stem cells. This mix could treat genetic diseases better. It might even cure diseases that are hard to manage now.
Potential applications of gene therapy combinations include:
The field of embryonic stem cell medicine is growing fast. New technologies are key to its growth. Researchers are finding new ways to use embryonic stem cells for treatments.
New tech is making stem cell therapies better and safer. Gene editing technologies like CRISPR/Cas9 are being used. They help fix genetic problems and make cells work better.
Embryonic stem cell therapy is being looked at for more than just Parkinson’s and Type 1 diabetes. It’s being studied for heart disease, spinal cord injuries, and neurodegenerative disorders.
“The versatility of embryonic stem cells makes them an attractive option for regenerative medicine, promising to repair or replace damaged tissues across multiple disease states.” – A Stem Cell Researcher
Progress is being made, but when these therapies will be widely used is not set. Clinical trials are underway for many conditions. It’s thought that the first approved treatments will come in the next decade.
As we move forward, it’s important to keep up with safety and effectiveness. This ensures that these new therapies truly help patients.
Embryonic stem cell therapy is showing great promise for treating serious diseases like Parkinson’s and type1 diabetes. These cells can grow into many different types of cells, making them very useful for fixing damaged tissues. This is a big step forward in regenerative medicine.
As scientists keep working, we’re seeing more ways embryonic stem cells can help in hospitals. There are hurdles like technical issues and safety worries, but the progress is clear. It’s a big leap forward.
Understanding how stem cell therapy works is key to making it work better. We need to keep pushing past current limits and finding new ways to use these cells. This will help us reach their full power.
In short, stem cell therapy is a bright spot in medicine, giving hope to those with no other treatments. We must keep researching and improving to make the most of this technology.
Embryonic stem cells come from embryos and can turn into different cell types. They help fix damaged tissues and might cure diseases.
What is the difference between embryonic stem cells and adult stem cells?
Embryonic stem cells can become any cell type. Adult stem cells mostly turn into cells related to their original tissue.
What is stem cell therapy, and how does it work?
Stem cell therapy uses stem cells to fix or replace damaged tissues. These cells can blend with the host tissue, helping it heal.
What are the potentials of using embryonic stem cells to treat Parkinson’s disease?
They might replace damaged dopamine-producing neurons. This could greatly improve life for Parkinson’s patients.
Can embryonic stem cells be used to treat type1 diabetes?
Yes, they can make new insulin-producing beta cells. This could be a new way to manage or cure type1 diabetes.
What are the challenges in developing embryonic stem cell therapies?
Scaling up production and standardizing therapies are big challenges. Also, getting these therapies to market is tough.
Are there any ongoing clinical trials for stem cell therapy?
Yes, trials are ongoing for various conditions. This includes Parkinson’s disease and type1 diabetes.
What are the ethical considerations surrounding embryonic stem cell research?
Ethical debates include moral and religious views. Laws aim to balance these with medical progress.
How do induced pluripotent stem cells (iPSCs) compare to embryonic stem cells?
iPSCs come from adult cells and act like embryonic stem cells. They offer a different way to treat diseases.
What is the future of embryonic stem cell medicine?
New technologies will open more treatment options. Embryonic stem cell therapies might become common in the future.
What are the risks associated with embryonic stem cell therapy?
Risks include problems in cell production and safety issues like tumors. There are also concerns about immune rejection.
How can patients access embryonic stem cell treatments?
Patients can get treatments through clinical trials or approved therapies. They must meet certain criteria and have insurance.
Embryonic stem cells come from embryos and can turn into different cell types. They help fix damaged tissues and might cure diseases.
Embryonic stem cells can become any cell type. Adult stem cells mostly turn into cells related to their original tissue.
Stem cell therapy uses stem cells to fix or replace damaged tissues. These cells can blend with the host tissue, helping it heal.
They might replace damaged dopamine-producing neurons. This could greatly improve life for Parkinson’s patients.
Yes, they can make new insulin-producing beta cells. This could be a new way to manage or cure type1 diabetes.
Scaling up production and standardizing therapies are big challenges. Also, getting these therapies to market is tough.
Yes, trials are ongoing for various conditions. This includes Parkinson’s disease and type1 diabetes.
Ethical debates include moral and religious views. Laws aim to balance these with medical progress.
iPSCs come from adult cells and act like embryonic stem cells. They offer a different way to treat diseases.
New technologies will open more treatment options. Embryonic stem cell therapies might become common in the future.
Risks include problems in cell production and safety issues like tumors. There are also concerns about immune rejection.
Patients can get treatments through clinical trials or approved therapies. They must meet certain criteria and have insurance.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us