Knowing when a patient needs a blood transfusion because of anemia is key for doctors. New guidelines have set clear levels for giving red blood cells to anemic patients.
The 2023 AABB guidelines say a transfusion is usually needed when a patient’s hemoglobin is less than 7 g/dL. This is for stable, non-bleeding adults in the hospital. This rule helps balance the good of transfusion with its risks.
Every patient is different, based on their health, heart disease, and how bad their anemia symptoms are. So, doctors must look at each case carefully.
Key Takeaways
- Hemoglobin levels below 7 g/dL usually mean a transfusion is needed for stable, non-bleeding adults.
- Each patient’s situation affects whether they get a transfusion.
- New guidelines try to reduce the dangers of transfusions.
- LIV Hospital leads in safe, focused transfusion care for patients.
- It’s vital to know the latest guidelines for the best care.
What Defines Anemia and When It Becomes Critical
Understanding anemia and its severity is key in patient care. Anemia happens when there are not enough red blood cells, hemoglobin, or hematocrit. The World Health Organization says anemia is when hemoglobin is below 13 g/dL in males and 12 g/dL in non-pregnant females. Knowing these levels is vital for diagnosing and treating anemia well.

Normal vs. Abnormal Hemoglobin Ranges
Hemoglobin levels tell us if someone has anemia. For men, normal levels are 13.8 to 17.2 g/dL. For women, it’s 12.1 to 15.1 g/dL. If levels drop below these, anemia is present. Anemia’s severity depends on how much the hemoglobin level drops.
How Anemia Severity is Classified
Anemia’s severity is based on the hemoglobin level. Mild anemia occurs when levels are just below normal. Severe anemia means levels are much lower. This classification helps decide the right treatment, such as whether a blood transfusion is needed. Knowing the severity is key for good patient care.
When thinking about a blood transfusion, doctors look at more than just hemoglobin levels. They also consider symptoms and the anemia’s cause. This detailed approach makes sure treatment fits the patient’s specific needs.
Standard Hemoglobin Thresholds for Blood Transfusion
There are set hemoglobin levels for when a blood transfusion is needed. These levels help doctors decide if a patient needs a transfusion to treat anemia.
The 7 g/dL Threshold for Stable Hospitalized Adults
The 2023 AABB guidelines say a hemoglobin level of 7 g/dL is okay for stable adults in the hospital. This rule helps avoid unnecessary transfusions and saves blood. Restrictive transfusion strategies are safe and work well for these patients.
Higher Thresholds for Specific Patient Groups
Some patients need higher hemoglobin levels for transfusions. For example, those with heart disease or having orthopedic surgery might need 7.5-8 g/dL. These higher levels help protect these patients from the risks.
- Patients with heart disease need more oxygen to the heart.
- Surgical patients, like those having big surgeries, also need higher levels.
Evidence from Clinical Trials Supporting Current Thresholds
Many studies have looked into the best hemoglobin level for transfusions. These studies back up the current guidelines. They show that giving blood only when really needed improves health and saves money. For example, a big study in the New England Journal of Medicine found that giving blood less often was better.
Knowing and using these hemoglobin levels helps doctors make better choices. This leads to better care and results for patients.
5 Patient Categories That Require Different Transfusion Approaches
Blood transfusions are not the same for everyone. Different patients need different approaches. Knowing these differences is key to better care.
Patients with Cardiovascular Disease
Those with heart disease need special care with blood transfusions. They can’t handle anemia as well as others. Restrictive transfusion strategies are often used, but adjusted based on heart function and symptoms.
For example, someone with severe heart disease might need more blood to keep the heart working. Doctors should decide together, considering the patient’s health.
Surgical Patients (Orthopedic and Cardiac)
Surgical patients, like those having orthopedic or cardiac surgery, have special needs. They might lose a lot of blood, so blood products must be carefully planned. Patient blood management programs help avoid unnecessary transfusions.
The right time and amount of blood transfusions can greatly affect how well a patient does. For cardiac surgery, the decision depends on the patient’s blood level, surgery complexity, and any bleeding issues.
Critically Ill Patients
Critically ill patients in the ICU often need blood transfusions. The goal is to improve oxygen delivery without risking complications like TRALI. A restrictive transfusion strategy is usually best, with a hemoglobin threshold of 7 g/dL.
This threshold can change based on the patient’s health, including heart issues or severe lack of oxygen.
Elderly Patients with Comorbidities
Elderly patients with health issues, like kidney disease or diabetes, need careful transfusion decisions. They are more at risk of anemia due to weaker body strength.
Transfusion decisions for elderly patients should consider their health, symptoms, and wishes. For example, those with dementia might need more proactive anemia management.
In conclusion, different patients need different blood transfusion approaches. Understanding these needs helps healthcare providers improve patient care and reduce risks.
7 Symptoms That May Warrant a Blood Transfusion Regardless of Hemoglobin Level
Certain symptoms may mean you need a blood transfusion, even if your hemoglobin level is okay. These signs show your body needs more red blood cells. This is to make sure tissues and organs get enough oxygen.
Chest Pain or Cardiac Symptoms
Chest pain or heart symptoms can mean your heart isn’t getting enough oxygen. Patients with chest pain or heart symptoms might need a blood transfusion. This helps ease the heart’s workload.
Severe Shortness of Breath
Severe shortness of breath, or dyspnea, is another warning sign. It can happen when your blood or tissues don’t get enough oxygen. We check how bad the shortness of breath is and how it affects you.
Hemodynamic Instability
Hemodynamic instability means big changes in blood pressure. This is a big sign you might need a blood transfusion. Patients with unstable blood pressure might get a transfusion to keep their vital signs stable.
Acute Blood Loss
Acute blood loss is a serious emergency that often needs a blood transfusion right away. How much blood is lost and how you react to treatment help decide if you need a transfusion.
Here are some symptoms that might mean you need a blood transfusion:
- Chest pain or angina
- Severe shortness of breath
- Hemodynamic instability
- Acute blood loss
- Dizziness or fainting spells
- Confusion or altered mental status
- Severe fatigue
Knowing these symptoms is key for doctors to decide on blood transfusions. By looking at these signs, we can make sure patients get the right care fast.
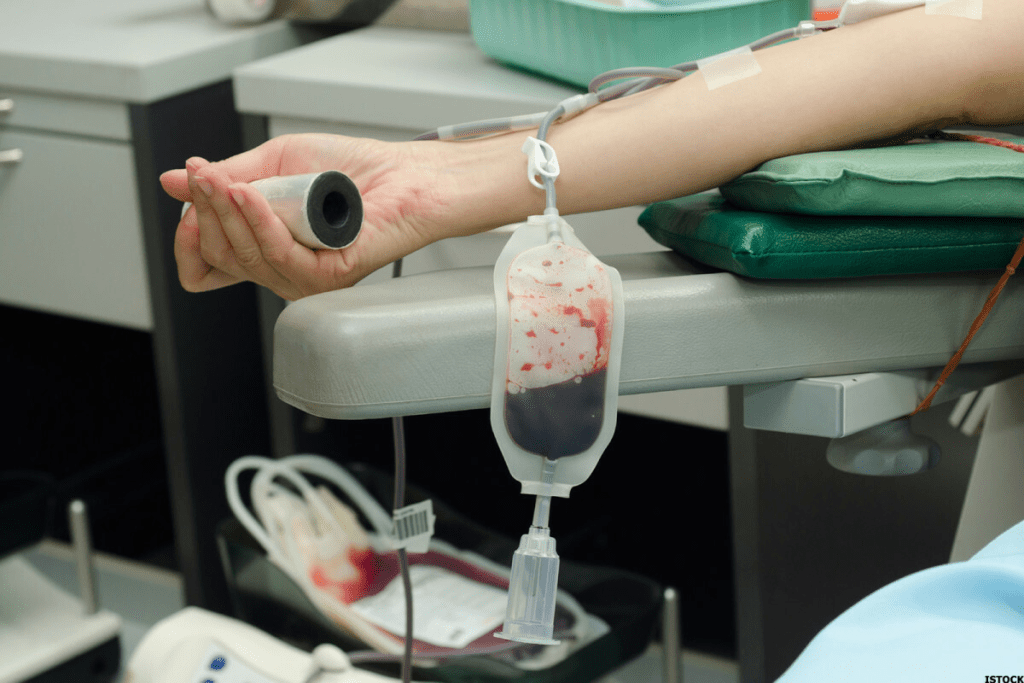
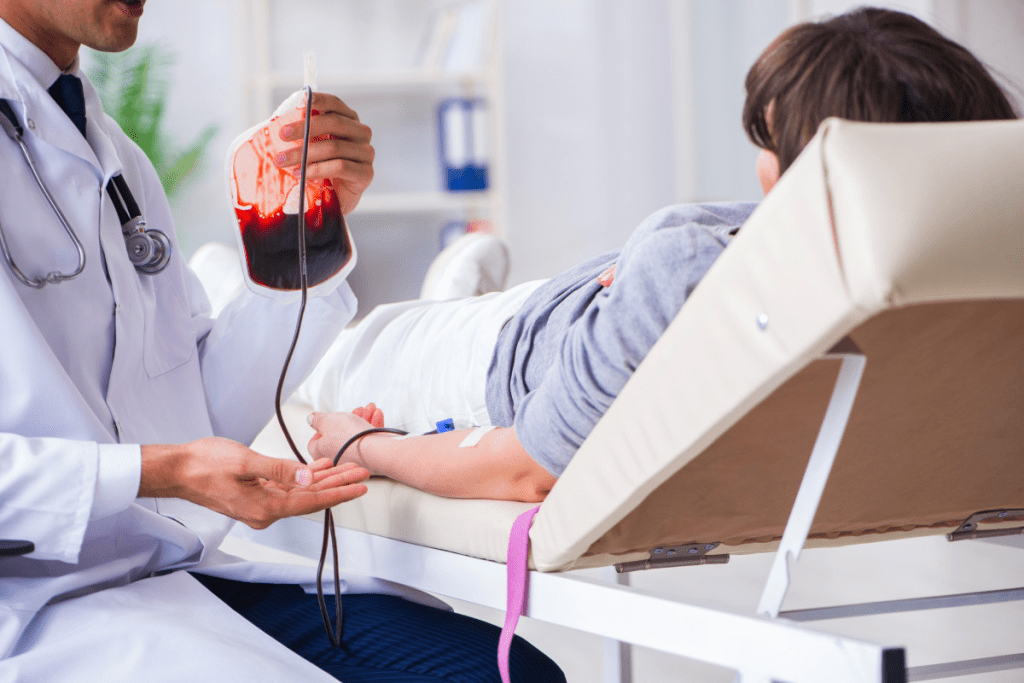
The Complete Blood Transfusion Process Explained
The blood transfusion process has many important steps to keep patients safe. We’ll cover the key stages, from getting ready to aftercare.
Pre-transfusion Testing Requirements
Before a blood transfusion, several tests are done to check if the donor’s blood matches the patient’s. These tests include:
- Blood typing to find the patient’s ABO blood group
- Rh factor testing to see if the patient is Rh positive or negative
- Cross-matching to make sure the donor’s blood is safe for the patient
- Screening for antibodies against blood components
These tests help avoid bad reactions during or after the transfusion.
How Long Does a Blood Transfusion Take
The time it takes for a blood transfusion varies. It depends on the patient’s health, how much blood is given, and how fast it’s given. Usually, it takes one to four hours to finish.
Monitoring During and After the Procedure
Healthcare professionals watch the patient’s vital signs closely during the transfusion. They check temperature, blood pressure, and heart rate. They also look for any signs of a bad reaction, such as:
- Rash or itching
- Shortness of breath
- Chest pain
- Fever or chills
After the transfusion, patients are watched for a bit to make sure there are no late reactions.
Post-transfusion Hemoglobin Assessment
After the transfusion, a hemoglobin test is done. This test checks if the transfusion worked. It measures the hemoglobin in the blood to see if it’s safe. The test results help decide if more transfusions are needed.
Knowing about the blood transfusion process helps patients prepare for this treatment. Our medical team is dedicated to caring for patients at every step of the transfusion.
Restrictive vs. Liberal Transfusion Strategies: What Research Shows
Clinical trials have given us insights into the outcomes of two blood transfusion strategies. These strategies differ in when a blood transfusion is given. We will look at the benefits and risks of each approach.
Benefits of Restrictive Approaches
Restrictive transfusion strategies are becoming more popular. They lead to fewer transfusions and lower risks of complications. By being more careful with blood transfusions, doctors can avoid bad reactions and reduce the need for blood products.
Studies show that these strategies don’t harm patients. They are a good choice for managing anemia in many patients.
Arecent study found that restrictive transfusions work well. They cut down on transfusions without harming patient safety. This is good for patients at risk of complications.
Potential Risks of Unnecessary Transfusions
Liberal transfusion strategies might lead to too many transfusions. This can expose patients to risks like TRALI, TACO, and allergic reactions. Restrictive strategies avoid these risks by only giving transfusions when needed.
Patient Outcomes Comparison from Major Studies
Studies have compared patient outcomes between restrictive and liberal transfusion strategies. They show that restrictive strategies are just as good or better. For example, a study on critically ill patients found similar outcomes with restrictive strategies.
This evidence supports using restrictive transfusion strategies as the standard for managing anemia.
In conclusion, research backs the use of restrictive transfusion strategies over liberal ones. By avoiding unnecessary transfusions, doctors can lower risks and improve patient outcomes.
Conclusion: Making Informed Decisions About Anemia Treatment
Knowing when a blood transfusion is needed for anemia is key to good care. We’ve looked at what makes a transfusion necessary. This includes how severe the anemia is, the patient’s symptoms, and their overall health.
New guidelines and studies back up the use of careful transfusion strategies. This means giving blood only when it’s really needed. It helps avoid risks like complications and infections.
Healthcare providers can make better choices about blood transfusions for anemia. They understand the role of transfusions in treating anemia. This knowledge helps them tailor care to each patient, improving their health.
The choice to give a blood transfusion for anemia should be thoughtful. It should consider the patient’s hemoglobin levels and symptoms. This way, patients get the best treatment for their anemia.
FAQ
What is a blood transfusion?
A blood transfusion is when donated blood is given to a patient through an IV line. It’s used to treat anemia, blood loss, or other blood-related conditions.
At what hemoglobin level is a blood transfusion typically required?
For adults in the hospital, a transfusion is usually needed when hemoglobin drops below 7 g/dL. But, for some patients, like those with heart disease or going through surgery, it might be at 7.5-8 g/dL.
What are the symptoms that may warrant a blood transfusion regardless of hemoglobin level?
Chest pain, severe shortness of breath, unstable blood pressure, or sudden blood loss might need a transfusion. This is true even if the hemoglobin isn’t very low.
How long does a blood transfusion take?
A blood transfusion can take 1-4 hours. It depends on how much blood is being given and the patient’s needs.
What is the difference between restrictive and liberal transfusion strategies?
Restrictive strategies mean blood is only given when hemoglobin is below 7 g/dL. Liberal strategies give blood at higher levels. Studies show restrictive is safer and saves blood.
What are the benefits of restrictive transfusion approaches?
Restrictive transfusions lower the risk of complications like lung injury and circulatory overload. They also help save blood for others.
How is anemia severity classified?
Anemia is classified by hemoglobin levels. Mild is 10-12 g/dL, moderate is 8-10 g/dL, and severe is below 8 g/dL.
What patient categories require different transfusion approaches?
Patients with heart disease, those going through surgery, those who are critically ill, or the elderly with health issues need special care. Their needs and health status guide the transfusion approach.
What is the purpose of pre-transfusion testing?
Pre-transfusion testing checks if the donated blood matches the patient’s blood. This reduces the risk of bad reactions.
How is the patient monitored during and after a blood transfusion?
Patients are watched closely during and after transfusions for signs of bad reactions. They’re checked for fever, chills, or changes in vital signs. The transfusion’s success in treating anemia is also monitored.
References
U.S. National Library of Medicine. (2022). Restrictive Red Blood Cell Transfusion Strategy for Patients in Intensive Care: A Systematic Review and Meta-Analysis. Transfusion Medicine Reviews, 36(4), 211-220.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9143543/


































