Last Updated on November 12, 2025 by
When you get a CT scan with contrast or an MRI with contrast, you might wonder about the contrast dye after. At LIV Hospital, we get your questions and care about your safety and health.
Many patients often ask how long is later when discussing recovery timelines, but it depends on health and treatment factors.
Most contrast dye goes out through your urine. Our team is here to help you understand what happens next. We want you to know that getting rid of the dye is usually easy. We’re here to support you every step of the way.
Key Takeaways
- The body mainly gets rid of contrast dye through urine.
- Procedures like CT scans and MRI with contrast are safe when done right.
- Places like LIV Hospital focus on keeping you safe and cared for.
- Knowing what happens to contrast dye after a scan can ease your worries.
- Our medical team is ready to offer full support and advice during your care.
The Role of Contrast in Medical Imaging
Contrast agents are substances that make body structures or fluids stand out in medical images. They are key in helping doctors see inside the body more clearly.
Definition and Purpose of Contrast Agents
Contrast agents, or media, are compounds that make internal structures visible in scans like X-rays and MRI. Their main job is to show differences between tissues, helping doctors spot problems.
These agents highlight important areas like blood vessels and tumors. This helps doctors find diseases early, leading to better treatment.
How Contrast Enhances Diagnostic Accuracy
Contrast agents make it easier to see the differences between body parts. This is key for spotting issues like tumors and seeing how far a disease has spread.
Contrast agents are now a must in many medical scans. They improve image quality, helping doctors make accurate diagnoses. This is vital for creating effective treatment plans.
| Imaging Modality | Type of Contrast Agent | Purpose |
| CT Scan | Iodinated Contrast | Enhances visibility of blood vessels and organs |
| MRI | Gadolinium-Based Contrast | Highlights tumors and inflammation |
| X-ray | Barium Sulfate | Visualizes the gastrointestinal tract |
Understanding contrast agents in medical imaging shows their importance in healthcare. They not only help doctors diagnose better but also lead to better patient care.
Types of Contrast Media Used in Different Procedures

Medical imaging uses different contrast media to improve accuracy. The right contrast agent depends on the imaging method and body area.
Iodinated Contrast for CT Scans
Iodinated contrast is key for CT scans. It has iodine, which shows up well on CT images. It’s great for seeing blood vessels, organs, and tumors.
“Iodinated contrast in CT scans has changed how we diagnose,” says Dr. John Smith, a radiologist. “It gives us vital info for accurate diagnoses and treatment plans.”
Gadolinium-Based Contrast for MRI
Gadolinium-based contrast is for MRI scans. It has gadolinium, which makes MRI images clearer. It’s best for soft tissues like the brain and organs.
Barium Sulfate for GI Studies
Barium sulfate is used in GI studies like barium swallows. It coats the GI tract, making it visible on x-rays. It’s great for finding ulcers, tumors, and other issues.
Other Specialized Contrast Agents
There are more contrast agents for specific imaging. For example, microbubble agents help with ultrasound to see blood flow and tissue.
New contrast agents keep improving medical imaging. They help doctors diagnose and treat many conditions better.
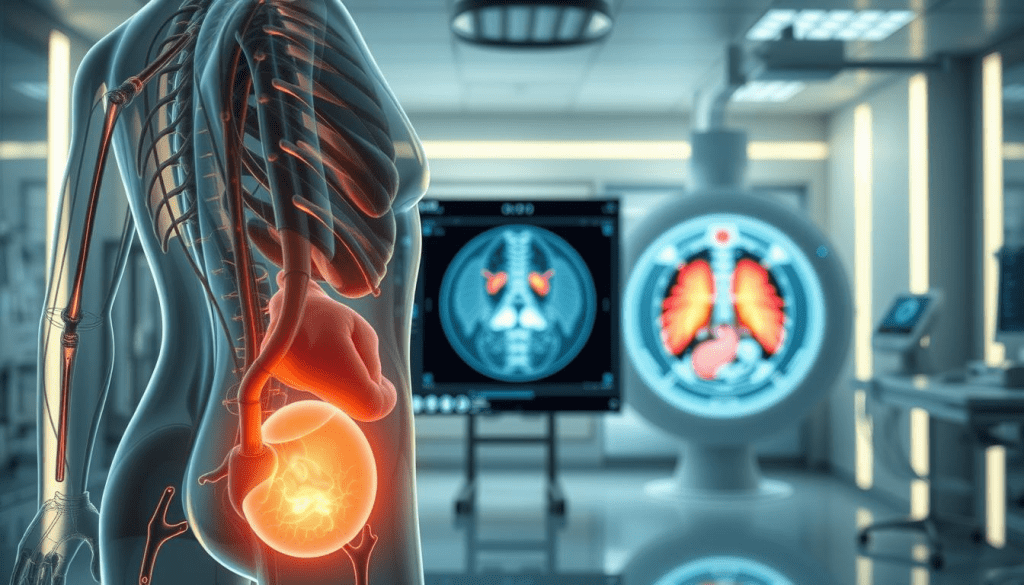
How Contrast Dye Travels Through Your Body
When injected, contrast dye moves through the bloodstream. It’s key for clear images in medical tests. This helps doctors see what’s going on inside the body.
Initial Distribution in Bloodstream
Right after it’s given, contrast dye spreads fast through the blood. This quick move is important. It helps get the dye to the right spots for clear images.
Tissue Absorption and Enhancement
The dye then gets absorbed by body tissues. This makes different parts of the body stand out more. It’s what makes images clearer and helps spot problems.
Preparation for Elimination
Soon after, the body starts getting ready to get rid of the dye. It uses special ways to filter it out. Mostly, it goes through the kidneys.
“The distribution and elimination of contrast dye are critical aspects of medical imaging, directly impacting the safety and efficacy of diagnostic procedures.”
| Process | Description |
| Initial Distribution | Contrast dye is dispersed through the bloodstream. |
| Tissue Absorption | Tissues absorb the contrast dye, making images clearer. |
| Preparation for Elimination | The body gets ready to remove the dye, mainly through the kidneys. |
Yes, You Do Pee Out Contrast Dye: The Primary Elimination Route
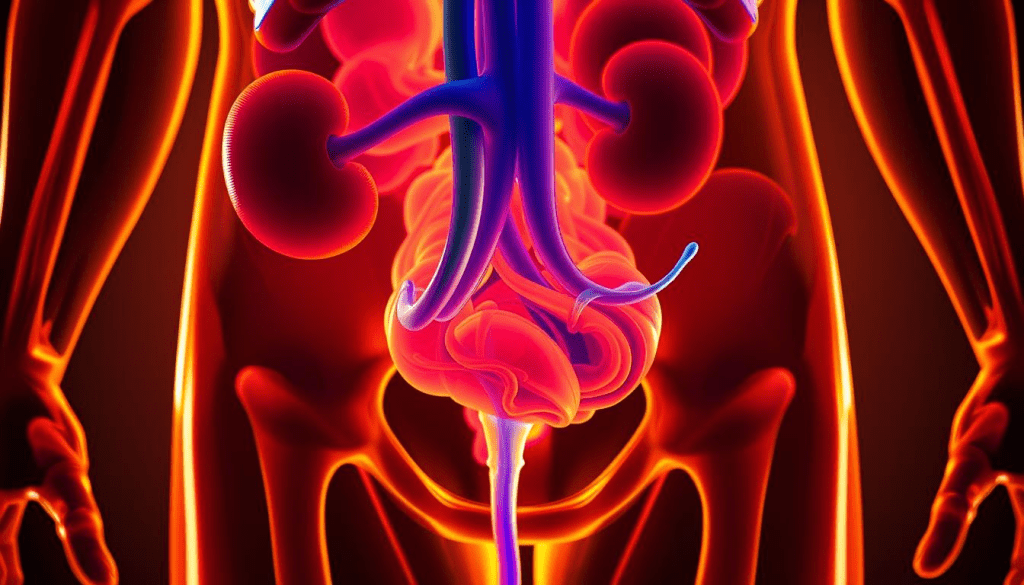
The kidneys are key in getting rid of contrast dye from the blood. This happens mainly through urination. When contrast dye is given during a medical scan, it spreads through the blood. The kidneys then filter it out and it ends up in the urine.
Kidney Filtration Process
The kidneys filter out waste and foreign substances, like contrast dye, from the blood. As the dye moves through the kidneys, it gets filtered by the glomeruli. Then, it goes into the renal tubules and is passed into the urine.
This process makes sure most of the contrast dye is removed from the body quickly. The kidneys’ role in filtering and removing contrast dye is vital. It keeps patients safe during imaging tests.
Percentage of Contrast Eliminated Through Urine
More than 90% of iodinated contrast agents leave the body through urine in 24 hours. This shows how well the kidneys work. It highlights the kidneys’ role in patients who get contrast agents.
Visual Changes in Urine After Contrast
Patients might see their urine change after getting contrast dye. It might look darker or more colored. This change usually goes away once the dye is fully out of the body.
It’s good for patients to know about these changes. But, if the color doesn’t go away or if they have pain or trouble urinating, they should talk to their doctor.
Timeline for Contrast Excretion in Healthy Individuals
Knowing how long it takes for contrast to leave the body is key for patients getting medical scans. This info helps set realistic expectations and understand how the body handles contrast agents.
First 24 Hours After Administration
Right after getting contrast, the body starts to get rid of it. The kidneys are key in this process, filtering out the contrast and sending it to the urine. Most of the contrast is gone within the first day, studies show.
Medium-Term Elimination (2-7 Days)
After the first 24 hours, the body keeps working to get rid of the contrast. How fast this happens can vary depending on things like kidney health and how much water you drink. Most of the contrast is out of the body in a few days.
Complete Return to Baseline Levels
A study at the University of Iowa found it takes about 43 days for urine iodine levels to get back to normal. This means while most of the contrast is gone quickly, it can take weeks for the body to fully recover.
It’s important to remember that everyone is different. Things like kidney health, how much water you drink, and your overall health can affect how fast contrast is removed. Doctors take these factors into account when using contrast agents and checking on patients.
University of Iowa Research on Long-Term Contrast Retention

The University of Iowa did a groundbreaking study on contrast retention. It showed us how contrast agents stay in our bodies over time. This study is key to understanding how these agents leave our bodies and how they affect our health.
Study Methodology and Patient Population
The University of Iowa used a detailed method to study contrast retention. They looked at how much iodine was in patients’ urine after they got contrast agents for scans. They picked patients carefully to make sure the study’s results were accurate and useful.
Findings on Urinary Iodine Levels
The study found interesting things about iodine in urine. By watching iodine levels over time, they saw how fast contrast agents leave our bodies. This info helps us understand the long-term effects of contrast agents and how to reduce risks.
The 43-Day Median Return to Baseline
A major discovery was that it takes about 43 days for iodine levels to go back to normal. This means, on average, it takes 43 days for our bodies to clear out the contrast agent. Knowing this helps doctors and patients plan better.
Implications for Patient Care
This research has big implications for taking care of patients. Knowing how long contrast agents stay in our bodies helps doctors manage risks. It also helps decide when to use contrast agents in scans, making sure the benefits outweigh the risks.
Secondary Routes of Contrast Elimination
While the kidneys are the main way to get rid of contrast agents, there are other paths too. These paths are key for people with health issues that affect how the kidneys work.
Hepatobiliary Excretion Pathways
The liver and bile ducts are important for getting rid of contrast agents. Hepatobiliary excretion is key for liver and bile duct imaging studies.
Some contrast agents, like those for X-ray and CT scans, go through the liver and bile. They get into the bile, then into the intestines. From there, they leave the body in feces.
| Characteristics | Renal Excretion | Hepatobiliary Excretion |
| Primary Organs Involved | Kidneys | Liver, Bile Ducts |
| Contrast Agents | Iodinated, Gadolinium-based | Specific Iodinated Agents |
| Elimination Route | Urine | Feces |
Minor Elimination Through Sweat and Feces
Contrast agents can also leave the body through sweat and feces. This is a smaller amount compared to the kidneys or liver.
Even though it’s less, it’s important for patients with kidney problems. It helps when the kidneys can’t do their job well.
Knowing how contrast agents leave the body is vital for doctors. It helps them take care of patients better, during imaging tests. By understanding these paths, doctors can make sure tests are safe and work well.
Factors That Affect How Quickly Contrast Leaves Your System
Many things can change how fast contrast dye leaves your body. Knowing these can help both patients and doctors manage imaging better.
Kidney Function and eGFR Measurements
Kidneys play a big role in getting rid of contrast dye. The estimated Glomerular Filtration Rate (eGFR) shows how well kidneys work. People with higher eGFR values get rid of contrast faster than those with lower values. Good kidney function is key for quick contrast removal.
Those with normal kidney function (eGFR above 90 ml/min/1.73m ²) usually get rid of contrast in a few hours to a couple of days. But, those with kidney problems might take longer.
Hydration Status Before and After Imaging
How well you’re hydrated before and after imaging also matters. Drinking enough water helps get rid of contrast dye. Doctors often tell patients to drink lots of fluids for this reason.
Staying hydrated keeps kidneys working well, which helps get rid of contrast dye faster. Doctors might give specific hydration advice based on each patient’s needs.
Age and Overall Health Considerations
Age and health can also affect how fast contrast dye leaves your body. Older people or those with health issues might have slower kidney function or other problems that slow down contrast removal.
For example, people with diabetes or high blood pressure might have kidney problems. This can slow down how fast contrast dye is removed. Doctors think about these factors when deciding if imaging with contrast is safe.
Dosage and Specific Type of Contrast Used
The amount and type of contrast used also matter. Different contrast agents are processed and removed at different rates by the body.
Some contrast agents are made to be removed quickly, while others stay longer. The specific contrast agent used can affect how long it takes to get rid of it.
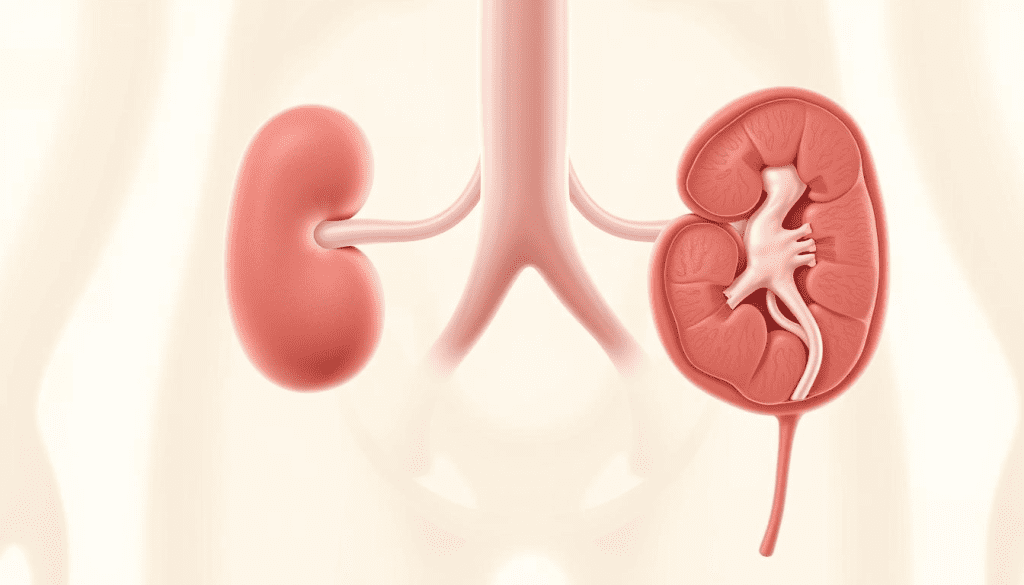
Contrast Excretion in People with Kidney Problems
People with kidney issues often have different ways of getting rid of contrast. This can affect their health and treatment plans.
Delayed Clearance in Renal Impairment
When kidneys don’t work well, contrast agents take longer to leave the body. This is because the kidneys can’t filter out the dye as they should. So, the dye stays longer, which can cause problems.
Delayed clearance is a big worry for those with very bad kidney problems. We keep a close eye on them to avoid any bad effects.
Risk Assessment Based on eGFR Values Below 30 ml/min/1.73m ²
Patients with an eGFR under 30 ml/min/1.73m ² face a higher risk from contrast. We check eGFR to see how well the kidneys are working. This helps us decide if they can safely have imaging with contrast.
- eGFR above 60: Generally considered safe for contrast administration
- eGFR between 30-60: Requires caution and potentially adjusted contrast dosage
- eGFR below 30: High-risk category; alternative imaging methods are often recommended
Alternative Imaging Options for High-Risk Patients
For those with very bad kidney function, we look into alternative imaging options without contrast. Options like ultrasound or non-contrast MRI are safer. They might not show as much detail, but they’re safer.
We know every patient is different. We try to find the best way to help each one, making sure they get the best care.
Gadolinium Contrast: Special Considerations for Excretion
Gadolinium contrast agents are used in MRI scans. They have unique ways of being removed from the body. Knowing how they are processed is key to their safe use.
Elimination Patterns of MRI Contrast Agents
Gadolinium-based contrast agents mainly leave the body through the kidneys. The process starts right after they are given, with most being gone in 24 hours. But, how fast they leave can change based on kidney health and the type of agent.
Key factors influencing elimination:
- Kidney function: Patients with kidney problems may take longer to clear them.
- Type of gadolinium agent: Each agent clears differently.
- Hydration status: Drinking enough water helps kidneys work better.
Concerns About Long-Term Retention
Research has found that gadolinium stays in the body for a long time. It can be found in the brain, bones, and skin, even after it’s first removed.
Potential risks associated with long-term retention:
- Nephrogenic systemic fibrosis (NSF) in patients with severe kidney impairment.
- Potential for gadolinium deposition in brain tissues.
Research on Gadolinium Deposition in Tissues
Studies have looked into where gadolinium goes in the body. While its long-term effects are not fully understood, it’s important to watch patients who have had these agents for any signs of problems.
We keep learning about how gadolinium contrast agents are removed from the body. By keeping up with new research and guidelines, we can make MRI scans safer for our patients.
Potential Risks of Delayed Contrast Excretion
When contrast dye stays in the body too long, it can harm health. This includes kidney damage and systemic fibrosis. Patients worry about this when they have medical imaging.
The risks of delayed contrast excretion are many. Contrast-induced nephropathy is a big worry, mainly for those with kidney problems.
Contrast-Induced Nephropathy
Contrast-induced nephropathy (CIN) is kidney damage from imaging contrast agents. It makes kidney function drop suddenly after contrast use. This is a big risk for those with kidney issues.
The reasons for CIN are complex. It includes the harm of contrast on kidney cells and less blood flow to the kidneys. Diabetes, heart failure, or kidney disease increase the risk of CIN.
Nephrogenic Systemic Fibrosis
Nephrogenic systemic fibrosis (NSF) is a serious issue with certain contrast agents in severe kidney cases. It makes skin and connective tissue harden, causing disability.
We stress the need for careful patient checks before using certain contrast agents. This helps avoid NSF.
Other Complications from Prolonged Retention
Long-term contrast agent retention can cause more problems. This includes long-term gadolinium deposition in tissues. This has raised concerns about long-term health effects.
We keep up with new research on contrast agent retention. We aim to use best practices to reduce these risks.
What to Expect After Receiving Contrast: The Patient Experience
Getting contrast dye is a key part of many medical tests. But what happens next? We’ll walk you through what you might feel, changes in how you pee, and when to worry.
Immediate Sensations During Administration
When you get contrast dye, you might feel a cold sensation or taste something metallic. This is usually short-lived and safe. Try taking slow, deep breaths to ease any discomfort.
Some people might feel a bit nauseous or dizzy. If this happens, tell the medical team right away. They can help you feel better.
Changes in Urination Patterns
Contrast dye leaves your body through pee. You might notice your pee looks different or you pee more often. This is usually okay and will pass.
| Change in Urination | Normal or Concerning? |
| Darker urine color | Normal |
| Increased frequency of urination | Normal |
| Painful urination | Concerning – consult a doctor |
| Blood in urine | Concerning – seek medical attention |
Normal vs. Concerning Symptoms
Some symptoms after getting contrast dye are normal, but others need medical help. Watch how your body reacts and get help if symptoms are bad or last a long time.
Normal symptoms include mild nausea, feeling warm or cold where you got the dye, and changes in pee. These usually go away quickly.
Concerning symptoms that mean you should see a doctor include a bad rash, trouble breathing, chest pain, or a lot of pain where you got the dye. If you have these, get help right away.
Knowing what to expect after getting contrast dye can make you feel less worried. It helps you get through the recovery better. If you’re unsure or have questions, talk to your doctor.
Preparing for Contrast-Enhanced Imaging Procedures
Contrast-enhanced imaging needs special preparation for accurate results and safety. Knowing what to do before your imaging can make it easier and less scary.
Pre-procedure Hydration Recommendations
Drinking lots of water is key before contrast-enhanced imaging. It helps your body use the contrast agent better. Staying hydrated can lower the chance of problems from the contrast.
Drink at least 8-10 glasses of water in the 24 hours before. But, your hydration needs might change based on your health and the imaging type.
Medication Considerations and Temporary Adjustments
Some medicines might need to be changed or stopped before your imaging. Tell your doctor about all your medicines, including supplements and over-the-counter ones.
Medicines like metformin for diabetes might need special care with contrast agents. Your healthcare team will tell you what to do with your medicines.
Fasting Requirements for Different Types of Scans
Fasting rules differ based on the imaging type. For some CT scans, fasting for a few hours is needed.
- For CT scans with contrast, fasting for 2-4 hours is often recommended.
- MRI procedures with contrast usually don’t need fasting, but it depends on the protocol.
- Always follow the specific instructions from your healthcare provider or the imaging facility.
By following these guidelines, you can help make your contrast-enhanced imaging safe and effective.
Post-Procedure Care to Help Eliminate Contrast Safely
To safely get rid of contrast dye, it’s key to follow a detailed care plan after your procedure. Your body needs support to clear out the dye. We have some strategies to help your body do this.
Optimal Hydration Strategies
Drinking lots of water is a top way to help your body get rid of contrast dye. Aim for 8-10 glasses of water in the first 24 hours after your test. Also, eat foods that help you stay hydrated, like watermelon or cucumbers.
Monitoring Your Urination After Contrast
Watching your urine after getting contrast dye is important. You might see changes in color or how often you pee. But, if you notice anything odd, like trouble peeing or pain, call your doctor right away. This helps you see how well your body is getting rid of the dye.
- Note the color and clarity of your urine.
- Monitor the frequency of your urination.
- Report any unusual symptoms to your healthcare provider.
When Follow-up Testing Might Be Necessary
In some cases, you might need follow-up testing to make sure the dye is gone. This is more likely if you have kidney problems or got a big dose of dye. Your doctor will decide if you need more tests based on your health and the test you had.
Following these care tips can help your body safely get rid of the dye. Always talk to your doctor for advice that fits your needs.
Advanced Contrast Safety Protocols in Modern Healthcare
Modern healthcare relies on advanced contrast safety protocols to keep patients safe during imaging. We focus on reducing risks from contrast agents. Our approach covers many areas.
Patient Screening and Risk Assessment
Checking patients before giving contrast agents is key. We look at kidney function, hydration, and past reactions. Thorough risk assessment helps us spot and prevent problems.
- Evaluate kidney function and eGFR levels
- Assess patient’s hydration status
- Review medical history for previous contrast reactions
Dose Optimization Techniques
Optimizing contrast doses is vital. We use the least amount needed to avoid bad reactions. This includes choosing lower osmolarity agents and adjusting how fast they’re given.
- Use the minimum effective dose of contrast agent
- Select contrast media with lower osmolarity
- Adjust the injection rate according to patient needs
International Best Practices Like Those at LIV Hospital
LIV Hospital leads in contrast safety with international best practices. They screen patients well, optimize doses, and watch patient results closely. This ensures top care for our patients.
By using advanced contrast safety protocols, we boost patient safety and care quality. It’s our dedication to excellence, helping both our patients and the healthcare world.
Conclusion
Contrast dye is key in medical imaging, making diagnoses more accurate. It is mainly removed by the kidneys and comes out in urine. Several things affect how fast it’s removed, like kidney health and how much water you drink.
Studies, like those from the University of Iowa, show most dye is gone in 24 to 48 hours in healthy people. But, those with kidney problems or other health issues might take longer. This shows why it’s important to check patients carefully before using dye.
Doctors use special safety steps to make sure imaging with dye is safe. This includes checking patients, using the right amount of dye, and caring for them after the test. For more details, look at studies in medical journals, like PubMed Central.
Knowing how dye is removed and using safety steps helps reduce risks. This way, patients get the best results from their imaging tests.
FAQ
What is contrast dye and how is it used in medical imaging?
Contrast dye, also known as contrast agent, is used to make medical images clearer. It’s used in X-rays, CT scans, and MRI scans. It helps doctors see specific parts of the body better, making diagnosis and treatment easier.
How is contrast dye eliminated from the body?
The body gets rid of contrast dye mainly through urine. The kidneys filter it out. How fast it’s eliminated depends on kidney function, how much water you drink, and your overall health.
How long does it take for contrast dye to be eliminated from the body?
In healthy people, most contrast dye is gone within 24 hours. It can take several days for all of it to return to normal levels.
Are there any risks associated with delayed contrast excretion?
Yes, delayed excretion can lead to risks. These include contrast-induced nephropathy and nephrogenic systemic fibrosis. People with kidney problems are at higher risk.
How can I prepare for a contrast-enhanced imaging procedure?
To prepare, stay hydrated and follow fasting instructions. Tell your doctor about any medications or health conditions. They may give more specific advice on what to do before the procedure.
What can I do to help eliminate contrast dye safely after a procedure?
Drink plenty of water to help eliminate the dye. Monitor your urine and follow any post-procedure instructions from your doctor.
Are there any special considerations for gadolinium contrast excretion?
Yes, gadolinium has its own elimination patterns and concerns. It can deposit in tissues. Talk to your doctor about any worries you have.
What are the advanced contrast safety protocols in modern healthcare?
Modern healthcare, like LIV Hospital, follows international safety standards. This includes screening patients, optimizing doses, and monitoring them closely during and after procedures.
References
- Nimmons, G. L., et al. (2013). Urinary iodine excretion after contrast computed tomography scan. JAMA Otolaryngology“Head & Neck Surgery. https://pubmed.ncbi.nlm.nih.gov/23599025/
- van der Molen, A. J., Reimer, P., Dekkers, I. A., et al. (2018). Post-contrast acute kidney injury ” Part 1: Epidemiology, definitions and mechanisms. European Radiology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5986826/
- Cheong, B. Y. C., et al. (2022). Gadolinium-based contrast agents: updates and answers. Frontiers / Review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9242635/
- Frydrychowicz, A., et al. (2018). Review of hepatobiliary-specific magnetic resonance contrast agents. European Journal of Radiology Open. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6385936/
- Modi, K., et al. (2023). Contrast-induced nephropathy. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448066/