Last Updated on November 27, 2025 by Bilal Hasdemir

Understanding and managing aortic ectasia is key to avoiding serious health issues. At Liv Hospital, we offer top-notch care for international patients. Our team includes cardiologists and specialists to ensure the best results.
We know that aortic ectasia needs careful watching and management. This is to stop it from getting worse and to avoid complications. We focus on controlling blood pressure and keeping an eye on the aorta’s size. This way, we tailor the aortic ectasia treatment to each patient’s specific needs.
Key Takeaways
- Effective management of aortic ectasia is key to avoiding serious health issues.
- Liv Hospital offers top-notch care for international patients with aortic ectasia.
- Our team of specialists works together to provide the best possible outcomes.
- Managing blood pressure is a key part of aortic ectasia treatment.
- Monitoring the aorta’s diameter is essential for preventing further dilation.
What is Aortic Ectasia: Definition and Clinical Significance

Aortic ectasia is when the aorta gets a bit wider but not as much as an aneurysm. Knowing this difference is key to understanding the risks and how to treat it.
This condition is common, mainly in older adults. For example, up to 9 percent of them might have aorta ascendens ectasia. It’s important to know the difference between mild widening and an aneurysm for proper care.
Mild Dilation vs. Aneurysm
Aortic ectasia means the aorta widens a bit but not enough to be called an aneurysm. An aneurysm is when it widens by 1.5 times or more. Ectasia is less severe but needs attention because it could get worse.
Why is aortic ectasia important? It can turn into a bigger problem like an aneurysm. So, doctors keep an eye on it and manage any heart issues.
Aorta Ascendens Ectasia Explained
Aorta ascendens ectasia is when the top part of the aorta widens a bit. It might lead to bigger problems and is often found during tests for other reasons.
This condition can cause aortic regurgitation, dissection, or aneurysm. So, it’s important to watch for and manage risk factors.
| Condition | Definition | Clinical Significance |
| Aortic Ectasia | Mild dilation of the aorta not meeting aneurysm criteria | Potential for progression to aneurysm or dissection |
| Aneurysm | Dilation 1.5 times normal aortic diameter or greater | High risk of rupture or dissection; requires immediate attention |
| Aorta Ascendens Ectasia | Mild dilation of the ascending aorta | Risk of aortic regurgitation, dissection, or aneurysm formation |
Understanding aortic ectasia helps doctors take better care of patients. It can help prevent serious problems related to the aorta.
Prevalence and Risk Factors

It’s important to know about aortic ectasia’s prevalence and risk factors. This condition, where the aorta gets wider, can cause serious heart problems if not treated. Knowing about it helps us manage it better.
We’ll look at how common aortic ectasia is, mainly in older people. We’ll also talk about what increases the chance of getting it. This info helps us find who’s at risk and how to prevent it.
Incidence Rates in Older Adults
Aortic ectasia is more common in older adults because of aging. As we get older, our aorta can get wider. Studies show that older people are more likely to have this condition.
Table: Incidence Rates of Aortic Ectasia by Age Group
| Age Group | Incidence Rate (%) |
| 50-59 | 2.5 |
| 60-69 | 5.1 |
| 70-79 | 8.3 |
| 80+ | 12.1 |
Common Risk Factors for Development
Several things can make aortic ectasia more likely. These include high blood pressure, high cholesterol, and smoking. It’s key to manage these to stop aortic ectasia from getting worse.
Hypertension is a big risk because it strains the aorta, making it wider. Hyperlipidemia also plays a part by making the aorta weaker.
Common Risk Factors:
- Hypertension
- Hyperlipidemia
- Smoking
- Family history of aortic diseases
Knowing these risk factors helps doctors create better plans to manage aortic ectasia. This way, we can treat it more effectively.
Symptoms and Diagnostic Approaches
It’s key to spot the symptoms of aortic ectasia early. This helps avoid serious problems later. Aortic ectasia might not show symptoms at first. But as it gets worse, different signs can appear.
Common Presenting Symptoms
People with aortic ectasia might feel chest pain, shortness of breath, or palpitations. Sometimes, doctors find it during a check-up or imaging for something else.
The symptoms depend on where and how much the aorta is dilated. For example, if it’s in the ascending aorta, it might cause aortic regurgitation. This can lead to feeling tired and short of breath.
Imaging Techniques for Diagnosis
Diagnosing aortic ectasia mainly uses imaging techniques. The top methods are:
- Echocardiography, which helps see the aortic root and ascending aorta.
- Computed Tomography (CT) scans, which give detailed aorta and surrounding images.
- Magnetic Resonance Imaging (MRI), which is great for checking the aorta and finding issues.
At Liv Hospital, we use the latest imaging to get a precise diagnosis. Regular checks are important, even for mild cases. This is because the condition can stay the same for years but needs watching to avoid problems.
We mix clinical checks with top-notch imaging to get a correct diagnosis. Then, we create a plan that fits the patient’s needs.
Natural History and Progression
Aortic ectasia grows slowly over time. This growth can be affected by many things. These include the patient’s age, other health issues, and their genes.
Knowing how aortic ectasia grows is key. It helps predict problems and plan how to manage them.
Typical Expansion Rates
Research shows that how fast aortic ectasia grows varies a lot. On average, it grows by 0.1 to 0.5 cm each year. This depends on the aorta’s size and if the person has high blood pressure.
Several things can affect how fast it grows:
- How big the aorta is at first
- If the person has high blood pressure
- If they smoke
- If their family has a history of aortic aneurysms
Potential Complications Without Treatment
If not treated, aortic ectasia can cause serious problems. The biggest risks are aortic rupture, dissection, and pressing on nearby structures.
Aortic rupture is very dangerous and can be deadly. This shows why finding and treating it early is so important.
Knowing about these risks makes it clear why regular checks and proper care are vital. They help avoid these serious issues.
Aortic Ectasia Treatment: Overview of Management Strategies
Treating aortic ectasia involves a detailed plan to manage the condition and prevent serious issues. We understand that every patient is different. So, we create treatment plans that meet their specific needs.
Treatment Goals and Objectives
The main goals of treating aortic ectasia are to manage blood pressure and keep an eye on the aorta’s size. By doing this, we can lower the risk of serious problems and improve how patients feel.
Specifically, treatment aims to:
- Control hypertension to reduce stress on the aortic wall
- Regularly monitor the aorta’s diameter to detect any changes
- Prevent aortic dissection or rupture
Factors Influencing Treatment Selection
Several factors affect the choice of treatment for aortic ectasia. These include the patient’s overall health, symptoms, and the size and location of the ectasia.
To illustrate the factors influencing treatment selection, consider the following table:
| Factor | Description | Impact on Treatment |
| Patient’s Overall Health | Presence of comorbidities such as hypertension or diabetes | Influences the choice of medication and intensity of monitoring |
| Presence of Symptoms | Symptoms such as chest pain or shortness of breath | May necessitate more aggressive treatment or surgical intervention |
| Size and Location of Ectasia | Diameter of the aorta and its location | Determines the need for regular monitoring or surgical repair |
Treatment Option 1: Blood Pressure Management
Blood pressure management is key in treating aortic ectasia. It’s important to control high blood pressure to avoid heart problems.
Studies show that keeping blood pressure in check can slow down aortic ectasia. Antihypertensive medications are essential for this. There are many types, each with its own benefits.
Antihypertensive Medication Classes
We use different types of antihypertensive drugs for aortic ectasia. These include:
- Angiotensin-Converting Enzyme (ACE) inhibitors, which relax blood vessels.
- Calcium Channel Blockers, which lower the heart’s workload.
- Beta-blockers, which slow the heart rate and lower pressure.
- Angiotensin II Receptor Blockers (ARBs), an alternative to ACE inhibitors.
A leading cardiology journal says, “Choosing the right antihypertensive depends on the patient’s health and other conditions.”
“Optimal blood pressure control is key to slowing the progression of aortic ectasia.”
Target Blood Pressure Levels
It’s important to reach the right blood pressure levels. We aim for below 130/80 mmHg, but it can vary.
Effective blood pressure management can lower the risk of aortic ectasia complications. This, along with other treatments, makes a complete plan for each patient.
Treatment Option 2: Lifestyle Modifications
Lifestyle changes are key in managing aortic ectasia. They help patients take control of their health. By choosing the right diet and staying active, people can slow down the disease’s growth.
Dietary Recommendations
Eating well is vital for aortic ectasia management. Focus on fruits, veggies, whole grains, and lean meats. Lowering sodium intake is also important. High sodium can worsen high blood pressure, a big risk for aortic ectasia.
The American Heart Association says a diet full of veggies, fruits, and whole grains is good for the heart. It should also limit sodium and added sugars.
“A healthy diet is foundational to maintaining cardiovascular health and managing conditions like aortic ectasia.”
Physical Activity Guidelines
Staying active is also key for managing aortic ectasia. Try for 150 minutes of moderate exercise weekly. Or, do 75 minutes of vigorous exercise, or mix both. Good activities include brisk walking, cycling, or swimming.
Before starting any new exercise, talk to your doctor. Make sure the exercise fits your health and abilities for safety and success.
Treatment Option 3: Risk Factor Control
Managing aortic ectasia starts with controlling risk factors. By tackling these factors, we can lower the risk of serious problems. This approach helps improve patient health.
Controlling risk factors means tackling smoking, cholesterol, and diabetes. These steps are key to reducing heart disease risk. They also slow down aortic ectasia’s growth.
Smoking Cessation Programs
Smoking is a big risk for aortic ectasia getting worse. Programs to help people quit smoking are vital. They use counseling and medicine to support quitting.
A study in the Journal of the American Heart Association showed quitting smoking can cut aortic aneurysm growth risk by 50%. This shows how quitting is key in managing aortic ectasia.
“Smoking cessation is a critical component of risk factor control for patients with aortic ectasia. By quitting smoking, patients can significantly reduce their risk of cardiovascular complications.”
Managing Cholesterol and Diabetes
It’s also important to manage cholesterol and diabetes for aortic ectasia. High LDL cholesterol and diabetes can lead to heart problems.
| Condition | Management Strategy | Benefits |
| High Cholesterol | Statin therapy, lifestyle modifications | Reduced LDL cholesterol, slowed disease progression |
| Diabetes | Glycemic control, lifestyle modifications | Reduced risk of cardiovascular complications, improved outcomes |
By managing cholesterol and diabetes well, we can lower the risk of heart problems. This is a key part of treating aortic ectasia.
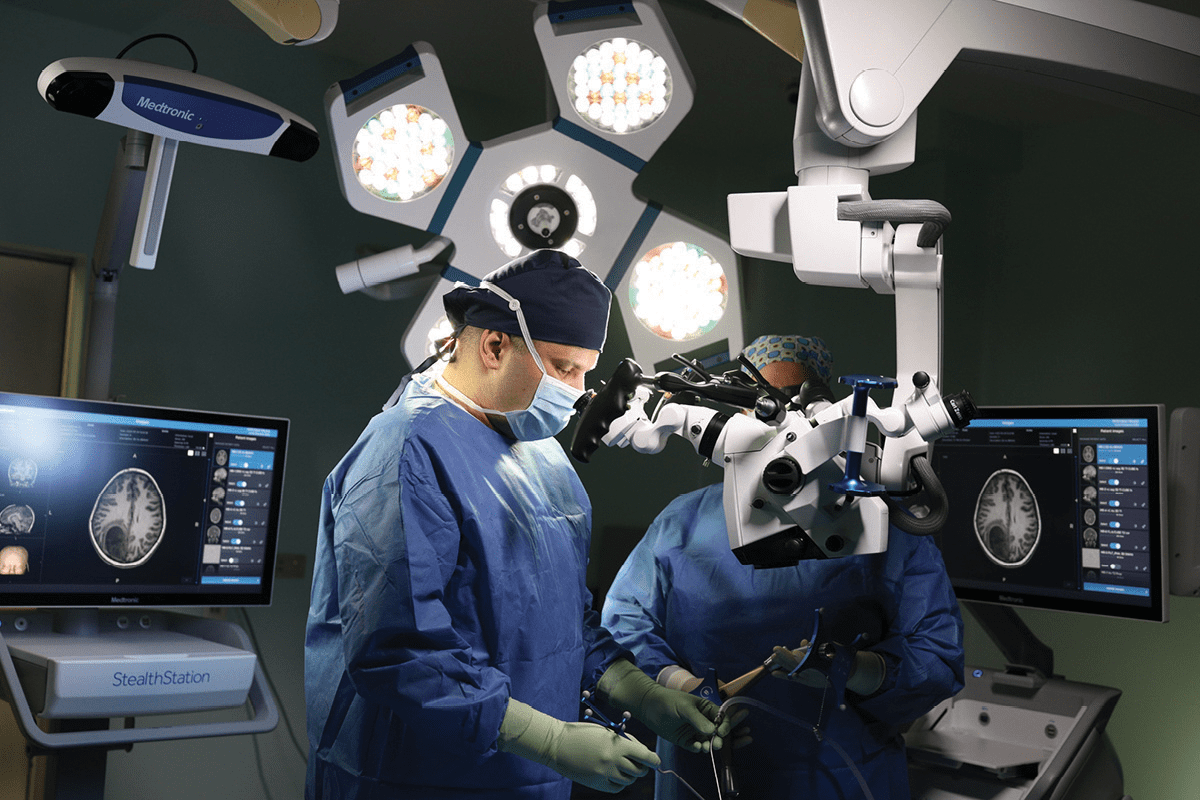
Treatment Option 4: Regular Imaging Surveillance
For those with mild aortic ectasia, regular imaging checks are key. This helps prevent serious issues like aortic dissection.
Recommended Monitoring Frequency
The timing of these checks varies based on the aorta’s size and the patient’s health. Here’s what we suggest:
- Annual or bi-annual scans for small ectasias
- More often for larger ectasias or those growing fast
Types of Imaging Studies
Several imaging methods are used to keep an eye on aortic ectasia. These include:
| Imaging Modality | Advantages | Limitations |
| Echocardiography | Non-invasive, easy to get | Depends on the doctor’s skill and patient factors |
| CT Angiography | Shows detailed images | Uses radiation and contrast |
| MRI Angiography | No radiation, great for soft tissues | Costlier, might cause claustrophobia |
At Liv Hospital, we use top-notch imaging to track aortic ectasia. Our radiologists team up with cardiologists for the best care.
Regular imaging checks are vital for managing aortic ectasia. They help catch problems early and lower the risk of serious issues. We adjust our monitoring plans for each patient to ensure they get the best care.
Treatment Option 5: Pharmacological Interventions
Pharmacological interventions are key for treating aortic ectasia. They help lower the risk of complications and slow the condition’s progression. We’ll look at the role of beta-blockers and other aortic-protective medications.
Beta-Blockers and Their Mechanism
Beta-blockers are vital in managing aortic ectasia. They reduce the heart’s contraction force and lower blood pressure. This reduces stress on the aortic wall, slowing its dilation.
Common beta-blockers include metoprolol and atenolol. Research shows they can slow aortic expansion in patients with aortic ectasia.
For more information on cardiovascular diseases, visit Patient.info. They offer detailed resources on thoracic aortic aneurysms and related conditions.
Other Aortic-Protective Medications
Other medications also protect the aorta and manage related conditions. These include:
- Angiotensin II receptor blockers (ARBs): These help lower blood pressure and reduce aortic wall stress.
- Statins: Primarily for cholesterol management, statins may also protect the aorta.
The right medication depends on the patient’s condition and other cardiovascular risks. A healthcare provider will choose the best treatment based on a thorough assessment.
In conclusion, pharmacological interventions are essential in managing aortic ectasia. Understanding these treatments helps healthcare providers create effective plans to improve patient outcomes.
Treatment Options 6 and 7: Surgical Approaches
Surgery is key in treating aortic ectasia, mainly for fast growth or symptoms. We’ll look at when surgery is needed, the open repair methods, and endovascular treatments.
Indications for Surgical Intervention
Surgery is for those with aortic ectasia who grow it fast or have symptoms. The choice to operate depends on the patient’s health and their condition’s details.
A study in the Journal of Thoracic and Cardiovascular Surgery found symptoms and fast growth are key for surgery.
“The presence of symptoms and rapid aortic dilation are strong predictors of the need for surgical repair in patients with aortic ectasia.”Journal of Thoracic and Cardiovascular Surgery
Open Surgical Repair Techniques
Open surgery replaces the aorta with a synthetic graft. It’s done under general anesthesia, with a cut in the chest to reach the aorta. The graft is sewn in place for a strong fix.
Open surgery’s benefits are:
- Long-lasting results
- Can handle complex aorta issues
- Well-established method
But, it also has risks:
- Severe post-op pain
- Chances of complications like bleeding or infection
- Longer healing time
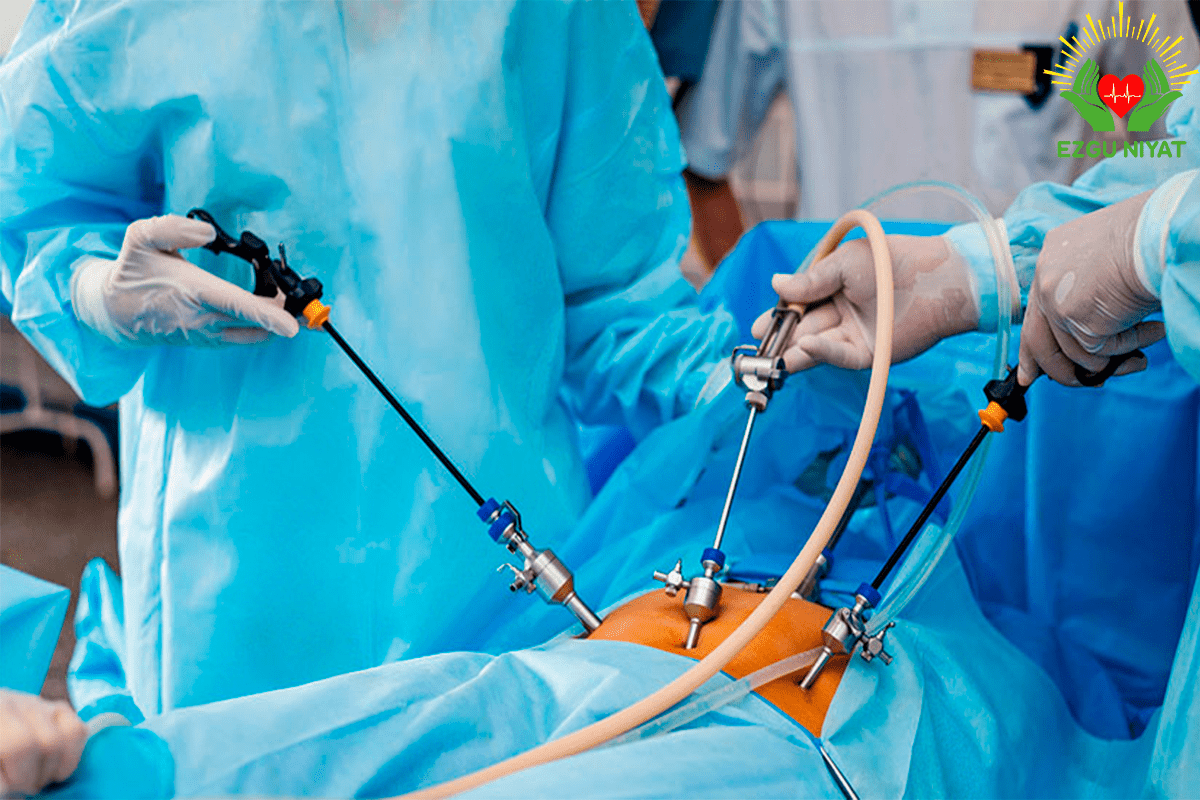
Endovascular Treatment Options
Endovascular treatment uses a stent-graft to block the aorta’s affected part. It’s less invasive, done under local or general anesthesia, guided by images.
| Treatment Option | Benefits | Risks |
| Open Surgical Repair | Durable long-term results, ability to address complex pathology | Significant postoperative pain, risk of complications |
| Endovascular Treatment | Minimally invasive, shorter recovery times, less postoperative pain | Risk of endoleak, stent-graft migration |
The table shows both methods have pros and cons. The right choice depends on the patient’s condition and health.
In summary, surgery is essential for aortic ectasia, providing effective treatments for those with fast growth or symptoms. We carefully decide on surgery and the best method for each patient.
Conclusion: Prognosis and Long-term Management
Managing aortic ectasia well needs a mix of treatments. We talked about seven ways to help, from controlling blood pressure to surgery. These methods aim to improve how patients feel and live.
The outlook for aortic ectasia depends on how bad it is and the patient’s health. With the right care, people can live better and avoid serious problems.
At Liv Hospital, we offer top-notch care for international patients. Our team creates custom plans for each patient. This ensures they get the best care possible.
Knowing how to manage aortic ectasia helps patients take charge of their health. We aim to support them every step of the way. Our goal is to help them reach their best health.
FAQ
What is aortic ectasia, and how is it different from an aortic aneurysm?
Aortic ectasia is when the aorta slightly expands but doesn’t qualify as an aneurysm. Both involve aorta enlargement, but ectasia is less severe.
What are the common risk factors for developing aortic ectasia?
Older age, high blood pressure, smoking, and genetics are common risks. Managing these can help prevent the condition from getting worse.
How is aortic ectasia diagnosed, and what imaging techniques are used?
Doctors use CT scans, MRI, or echocardiography to diagnose aortic ectasia. These tests check the aorta’s size and shape.
What are the treatment goals for managing aortic ectasia?
The main goals are to control blood pressure, manage risk factors, and monitor the condition. This aims to prevent complications and slow aorta expansion.
How is blood pressure managed in patients with aortic ectasia?
Managing blood pressure is key. Doctors often prescribe beta-blockers to keep blood pressure in check and reduce aorta strain.
What lifestyle modifications are recommended for patients with aortic ectasia?
Patients should eat healthy, exercise regularly, and quit smoking. These changes help manage risk factors and improve heart health.
How often should patients with aortic ectasia undergo imaging surveillance?
Imaging frequency varies based on individual risk factors. Regular CT or MRI scans are usually recommended to track aorta dilation.
What pharmacological interventions are used to treat aortic ectasia?
Beta-blockers and other medications are used to manage aortic ectasia. They help lower blood pressure and protect the aortic wall.
When is surgical intervention considered for aortic ectasia?
Surgery is considered for significant dilation or symptoms. The decision depends on health and aorta size.
What are the benefits and risks associated with surgical approaches to treating aortic ectasia?
Surgery can prevent further dilation and reduce rupture risk. But, it also carries surgery risks and complications.
What is the prognosis for patients with aortic ectasia, and how can long-term management be optimized?
Prognosis varies based on condition severity and management. Long-term, regular monitoring, lifestyle changes, and treatment adherence are key to better outcomes.
References
Journal of the American College of Cardiology (JACC): Aortic Dilatation and Aneurysm Management (Specific DOI
PubMed Central (NCBI): Genetics of Aortic Aneurysm (Specific PMC ID)