Immunotherapy failed? We discuss the alternative treatments and clarify can immunotherapy cure stage 4 cancer when initial treatments aren’t successful.
Immunotherapy is a new way to fight cancer by using the body’s immune system. It has shown great promise in treating many cancers, including melanoma that has spread.

When immunotherapy works, it can add months or even years to a patient’s life. But sometimes, it doesn’t work as well as hoped. This leaves patients and doctors looking for other options.
Looking ahead, doctors might try other treatments or mix different ones. These new approaches are being studied to help those who don’t respond to immunotherapy.
Key Takeaways
- Immunotherapy uses the body’s immune system to fight cancer.
- It can be effective in treating various types of cancer.
- Alternative treatments are being explored when immunotherapy fails.
- Combination treatments offer new hope for patients.
- Research is ongoing to develop more effective treatments.
Understanding the Basics of Immunotherapy
Immunotherapy has changed cancer treatment by using the body’s immune system to fight cancer. This new method has shown great promise in treating different cancers. It offers hope to patients who don’t respond well to traditional treatments.
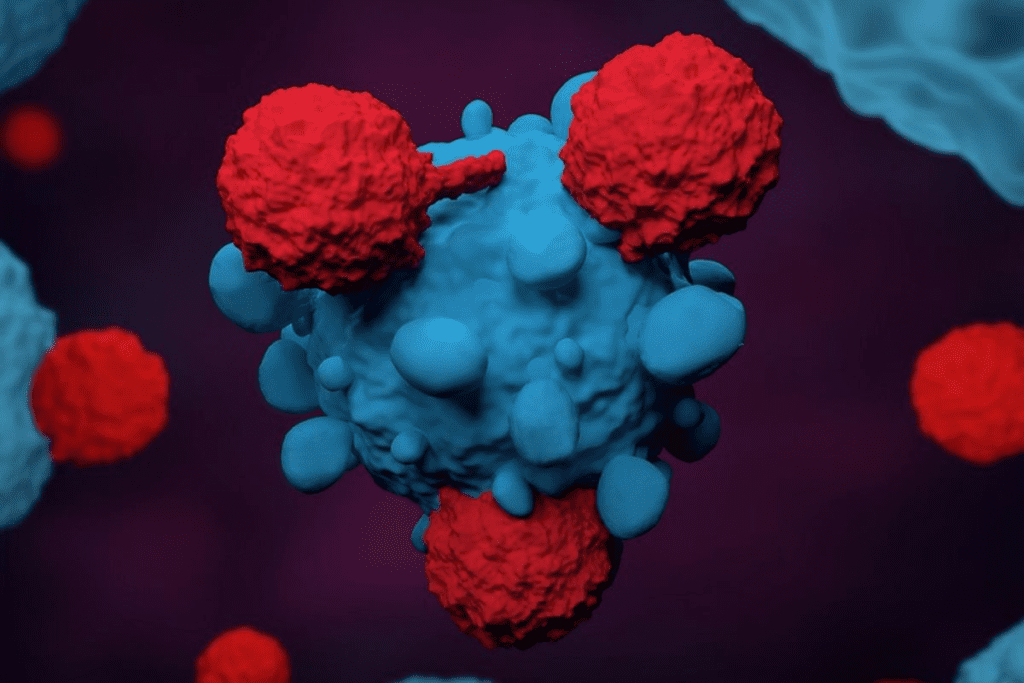
How Immunotherapy Fights Cancer
Immunotherapy boosts the immune system to better fight cancer cells. It helps the immune system see cancer cells more clearly. This makes it easier for the immune system to destroy these harmful cells.
The immune system uses various ways to fight cancer. It activates immune cells like T-cells and dendritic cells. These cells are key in recognizing and killing cancer cells. Immunotherapy en
hances these natural processes, leading to better cancer treatment.
Types of Immunotherapy Treatments
There are many types of immunotherapy treatments. Each works differently to fight cancer. These include:
- Checkpoint inhibitors, which let the immune system attack cancer cells more freely.
- Cancer vaccines, which help the immune system recognize and fight cancer cells.
- Adoptive T-cell therapy, where T-cells are taken, changed, and put back to better target cancer cells.
- Cytokines, proteins that boost the immune response to fight cancer.
How Long Immunotherapy Stays in Your System
The time immunotherapy stays in your system varies. It depends on the type of treatment, the dose, and the patient. Generally, immunotherapy’s effects can last weeks to months after treatment ends. Knowing how long it stays active is key for planning future treatments.
Even after treatment stops, the immune system can remember cancer cells. This means it can keep fighting cancer even after treatment is over.
Can Immunotherapy Cure Stage4 Cancer?
The question of whether immunotherapy can cure stage 4 cancer is complex. It depends on many factors. Immunotherapy has changed how we treat advanced cancers. It offers hope to those who have tried other treatments.
Success Rates in Advanced Cancer
Success rates for immunotherapy in stage 4 cancer vary a lot. This depends on the cancer type, patient health, and the treatment used. Some patients see durable responses, with their cancer staying in remission for a long time.
Recent studies show that some cancers, like melanoma and non-small cell lung cancer, respond well to immunotherapy. For example, pembrolizumab has shown great results in treating advanced melanoma.
Factors Affecting Treatment Response
Many factors affect how well a patient responds to immunotherapy. These include:
- The type and stage of cancer
- The patient’s overall health and immune function
- Genetic mutations present in the tumor
- Previous treatments the patient has undergone
A leading oncologist notes, “The presence of certain biomarkers can greatly affect immunotherapy’s success. This makes personalized treatment plans very important.”
“Immunotherapy has changed the landscape of cancer treatment, giving hope to patients with advanced disease.”
Realistic Expectations for Stage 4 Patients
While immunotherapy is promising, stage 4 cancer patients need to have realistic expectations. It may not work for everyone, and its success can vary a lot.
Patients should talk to their healthcare provider about their prognosis and treatment options. They should understand both the benefits and limitations of immunotherapy for their case.
Recognizing Signs Immunotherapy Is Not Working
For patients on immunotherapy, knowing when it’s not working is key. Immunotherapy has changed cancer treatment, but it works differently for everyone. Spotting when it’s not effective is important for finding new ways to help.
Clinical Indicators of Treatment Failure
Clinical signs are important in checking if immunotherapy is working. Symptoms like more pain, tiredness, or worsening cancer symptoms can mean it’s not working. Doctors watch these signs closely to see if the treatment is helping.
A patient’s overall health is also a big clue. If they get better or stay the same, it’s a good sign. But if they get worse, it might mean the treatment isn’t working.
Imaging and Laboratory Evidence
Imaging tests like CT scans and PET scans help see how tumors are doing. If tumors grow or new ones show up, it means the treatment isn’t working. Blood tests that check for tumor markers also give important clues.
Lab tests can show problems before symptoms do. So, regular tests are key to catching treatment failure early.
Distinguishing Between Side Effects and Disease Progression
It can be hard to tell if side effects or disease progression are happening. Side effects can look like disease getting worse, so careful checks are needed.
Doctors use their knowledge, imaging, and lab tests to tell the difference. Knowing this helps them decide if to keep or change the treatment.
Why Immunotherapy Treatment May Be Discontinued
Several factors can lead to stopping immunotherapy. These include disease progression and severe side effects. It’s important for patients and doctors to understand why treatment might end.
Disease Progression Despite Treatment
When cancer grows despite treatment, doctors might stop immunotherapy. They look for other treatments to try.
Doctors use tests like imaging and lab work to check if cancer is getting worse. If it is, the current treatment isn’t working.
Severe Side Effects and Toxicities
Severe side effects are another reason to stop immunotherapy. While it can be effective, it can also cause serious problems for some patients.
These side effects can really affect a patient’s life. Sometimes, doctors can manage them. But often, they need to stop the treatment.
Why Immunotherapy Is Often Stopped After 2 Years
Immunotherapy is often stopped after 2 years for several reasons. One reason is that it might not work as well over time. Or, the patient might have gotten the benefits they needed.
Stopping treatment after 2 years can also help avoid long-term side effects. It can also save money on care. But, this decision depends on each patient’s situation and how they respond to treatment.
Alternative Treatment Options After Immunotherapy
The journey doesn’t end when immunotherapy stops working. There are many other treatments to consider. When immunotherapy is no longer effective, patients and their healthcare providers must explore alternative treatment options to manage their cancer.
Returning to Traditional Chemotherapy
One of the primary alternative treatments is returning to traditional chemotherapy. Chemotherapy uses drugs to kill cancer cells. It’s often used when the cancer has spread or is in an advanced stage. While it can have significant side effects, chemotherapy remains a viable option for many patients.
Benefits of Chemotherapy:
- Effective in treating various types of cancer
- Can be used in combination with other treatments
- Helps in reducing tumor size and slowing disease progression
Targeted Therapy Approaches
Targeted therapy is another alternative treatment. It focuses on specific molecules involved in cancer growth and progression. By targeting these molecules, the therapy can help stop the cancer from growing and spreading.
Key aspects of targeted therapy include:
- Precision in targeting cancer cells, reducing harm to healthy cells
- Potential for fewer side effects compared to traditional chemotherapy
- Can be used alone or in combination with other treatments
Radiation Therapy Considerations
Radiation therapy is a treatment that uses high-energy rays to kill cancer cells or slow their growth. It’s often used when the cancer is localized or to alleviate symptoms such as pain.
Considerations for Radiation Therapy:
- Effective for localized tumors or to relieve symptoms
- Can be used in combination with other treatments like chemotherapy
- Helps in improving quality of life by reducing cancer-related symptoms
In conclusion, there are several alternative treatment options available after immunotherapy. Each has its benefits and considerations. Patients should discuss these options with their healthcare providers to determine the best course of action for their specific situation.
Combination Treatment Strategies
When just one treatment isn’t enough, combining therapies can help. Cancer is complex, so a mix of treatments might work better. This approach can lead to better results for patients.
Chemoimmunotherapy Combinations
Chemoimmunotherapy combines chemotherapy with immunotherapy. It’s a promising way to fight cancer. This method uses chemotherapy to kill cancer cells and boosts the immune system with immunotherapy.
Benefits of Chemoimmunotherapy:
- Enhanced cancer cell killing
- Improved immune system activation
- Potential for better treatment outcomes
Dual Immunotherapy Approaches
Dual immunotherapy pairs different immunotherapies to fight cancer better. It combines checkpoint inhibitors with other treatments. This way, it targets cancer from different angles.
This method aims to boost the immune system’s fight against cancer. It does this by attacking cancer through multiple paths.
Adding Targeted Agents to Immunotherapy
Targeted therapy uses drugs that only harm cancer cells. When added to immunotherapy, it makes the treatment more effective. This is because it focuses on cancer without harming healthy cells.
Examples of targeted agents include:
- Monoclonal antibodies that target specific proteins on cancer cells
- Tyrosine kinase inhibitors that block signals promoting cancer growth
Success Rates of Combination Approaches
Studies show that combining treatments can greatly improve outcomes for cancer patients. The success depends on the cancer type, the treatments used, and the patient’s health.
Key Takeaways:
- Combination treatments offer new hope for patients who don’t respond to single-modality therapies.
- Chemoimmunotherapy and dual immunotherapy approaches are showing promising results in clinical trials.
- The addition of targeted agents to immunotherapy can further enhance treatment efficacy.
Clinical Trials as a Critical Next Step
Clinical trials are a key next step for those who haven’t seen results from immunotherapy. They offer new treatments that could help patients, including those with NSCLC.
Finding Appropriate Clinical Trials
Finding the right clinical trial can be tough. Start by talking to your oncologist. They can find trials that match your condition and medical history. Online resources like the ClinicalTrials.gov website also have lots of information.
It’s important to check if you qualify for each trial. Look at the trial’s location, benefits, risks, and support offered.
The CAN-2409 Trial for NSCLC Patients
The CAN-2409 trial is for NSCLC patients. It’s testing a new gene therapy with standard treatments. The goal is to boost the immune system against cancer, improving survival and quality of life.
“The CAN-2409 trial represents a significant advancement in the treatment of NSCLC, giving new hope to patients who have tried other options,” said, a leading researcher in the field.
Other Promising Clinical Trial Results
There are many clinical trials showing promising results. For example, trials combining immunotherapy with other treatments are showing good results. These studies are changing how we treat cancer.
- Trials investigating dual immunotherapy approaches
- Studies examining the addition of targeted agents to immunotherapy regimens
- Research on novel antibody-based treatments
Questions to Ask Before Enrolling in a Trial
Before joining a clinical trial, ask important questions:
- What are the trial’s main goals, and how might it help my condition?
- What are the possible risks and side effects?
- How will my progress be tracked, and what support is available?
- Are there any extra costs for participating?
Thinking about these questions and talking to healthcare professionals can help you make a good choice about joining a trial.
Cancer-Specific Approaches After Immunotherapy Failure
When immunotherapy doesn’t work, doctors look at other treatments. Each cancer type reacts differently to treatments. So, it’s important to choose the right treatment for each cancer.
Non-Small Cell Lung Cancer (NSCLC) Options
For NSCLC patients, there are several options after immunotherapy fails. These include:
- Targeted therapy against specific genetic mutations
- Chemotherapy regimens tailored to the patient’s condition
- Participation in clinical trials for new NSCLC treatments
Targeted therapy is promising for NSCLC with certain genetic markers. For example, EGFR mutations can be treated with specific inhibitors.
Small Cell Lung Cancer Treatment Pathways
Small cell lung cancer (SCLC) is aggressive. After immunotherapy fails, treatments may include:
- Topotecan or irinotecan-based chemotherapy
- Re-challenge with the initial chemotherapy regimen if there’s a long treatment-free interval
- Clinical trials investigating new agents for SCLC
SCLC treatment often combines chemotherapy and radiation. Clinical trials are key to finding new treatments.
Melanoma Alternative Strategies
For melanoma patients who progress after immunotherapy, several options are available:
- Targeted therapy against BRAF mutations
- Combination regimens of different immunotherapies
- Local treatments such as surgery or radiation for isolated metastases
Targeted therapy against BRAF mutations is effective in melanoma with this mutation.
Approaches for Other Common Cancer Types
Other cancers like breast, colon, and prostate also have specific treatments after immunotherapy fails. These may include:
- Hormonal therapies for hormone receptor-positive cancers
- Targeted therapies against specific molecular targets
- Chemotherapy and radiation therapy tailored to the cancer type and stage
The right treatment depends on the cancer’s genetic profile, previous treatments, and the patient’s health.
Emerging Treatments Beyond Standard Immunotherapy
The world of cancer treatment is changing fast. New therapies are being developed that go beyond traditional treatments. These new options give hope to patients when usual treatments don’t work.
Engineered Cell Therapies
Engineered cell therapies, like CAR-T cell therapy, are big steps forward. They change a patient’s T cells to better fight cancer.
Key benefits of engineered cell therapies include:
- Targeted action against cancer cells
- Potential for long-term remission
- Ongoing research to improve efficacy and reduce side effects
New Cytokine Agonists
Cytokine agonists boost the body’s immune fight against cancer. They help the immune system find and kill cancer cells better. Experts say cytokine therapy could work well with other treatments, attacking cancer from different angles.
“The development of new cytokine agonists represents a promising frontier in cancer immunotherapy, giving new hope to patients with advanced disease.”
Novel Antibody Approaches
New antibody methods are being made to target cancer more precisely. Bispecific antibodies, for example, can hit two targets at once. This makes them very promising. Many are being tested in clinical trials.
Biomarker-Guided Treatment Selection
Biomarkers are key in choosing the right treatment for cancer. They help doctors pick treatments based on a patient’s cancer type. This makes treatments more personal and could lead to better results.
Life Expectancy and Quality of Life Considerations
When immunotherapy stops working, it’s important to know about life expectancy and quality of life. This helps patients and their families make informed decisions about treatment.
Understanding Survival Statistics When Treatments Stop Working
Survival statistics are key for patients whose cancer doesn’t respond to immunotherapy.
The survival rate shows the percentage of patients alive after a certain time. For example, a 5-year survival rate means the percentage of patients alive 5 years after diagnosis.
Balancing Treatment Efficacy and Side Effects
It’s important to weigh treatment benefits against side effects. More effective treatments can have severe side effects, affecting quality of life.
- Evaluating the benefits and risks of continuing treatment.
- Assessing the impact of treatment on daily life and well-being.
- Considering alternative treatments with better side effect balance.
Supportive and Palliative Care Options
Supportive and palliative care are vital when treatments fail. They focus on relieving symptoms and stress of serious illnesses.
Palliative care teams help manage pain and symptoms. They improve quality of life. Healthcare professionals say, “Palliative care is not just for end-of-life care; it’s for anyone living with a serious illness.”
“Palliative care is specialized medical care for people living with a serious illness, such as cancer. This type of care is focused on providing relief from the symptoms and stress of a serious illness.”
Making Informed Decisions About Continuing Treatment
Deciding to continue treatment involves many factors. These include benefits, risks, and quality of life impact. Patients should talk to their healthcare team about their options.
- Understanding the goals of continuing treatment.
- Evaluating the outcomes and risks.
- Considering personal preferences and values.
By carefully considering these factors, patients can make decisions that meet their needs and priorities.
Conclusion
When immunotherapy doesn’t work, knowing what to do next is key. This article covered the basics of immunotherapy and its role in stage 4 cancer. It also looked at signs that treatment might not be working and other treatment options.
It’s important to know when immunotherapy isn’t effective. There are many other ways to treat cancer, like traditional chemotherapy and targeted therapy. Radiation therapy is also an option.
Cancer treatment is complex, but there’s hope. Using a mix of treatments, like combining chemotherapy with immunotherapy, can help. Clinical trials are also important for finding new ways to fight cancer.
In short, while immunotherapy might not work for everyone, there are many other ways to treat cancer. By learning about these options and staying up-to-date on cancer research, patients can make better choices. This helps them keep fighting cancer.
FAQ
What is immunotherapy, and how does it work?
Immunotherapy is a cancer treatment that uses the immune system to fight cancer. It makes the immune system attack cancer cells. It also introduces immune cells that target cancer cells.
How long does immunotherapy stay in your system?
Immunotherapy’s stay in the system varies by treatment and individual factors. Some treatments can last months or even years after stopping.
What are the signs that immunotherapy is not working?
Signs it’s not working include disease growth, worsening symptoms, and lab and imaging results showing no response.
Why is immunotherapy stopped after 2 years?
It may stop after 2 years due to severe side effects, disease progression, or the end of the planned treatment.
What happens when immunotherapy stops working?
If it stops working, other treatments like chemotherapy or targeted therapy might be considered. Clinical trials could also be an option.
Can immunotherapy cure stage 4 cancer?
Immunotherapy shows promise for stage 4 cancer. But success rates depend on the cancer type, individual factors, and more.
What are the alternative treatment options after immunotherapy?
After immunotherapy, options include chemotherapy, targeted therapy, radiation therapy, or combination treatments.
What is the role of clinical trials in cancer treatment?
Clinical trials are key in cancer treatment. They offer new treatments, including emerging therapies and combination strategies.
How do I find appropriate clinical trials for my cancer treatment?
To find clinical trials, search online databases, talk to your healthcare provider, or contact cancer organizations for help.
What are the emerging treatments beyond standard immunotherapy?
New treatments include engineered cell therapies, cytokine agonists, antibody approaches, and biomarker-guided treatments.
How do I make informed decisions about continuing treatment?
Discuss your options with your healthcare provider. Consider treatment effectiveness, side effects, and quality of life.
What is the life expectancy when treatments stop working?
Life expectancy varies by cancer type, overall health, and other factors when treatments stop working.
What is meant by immunotherapy?
Immunotherapy is a cancer treatment that uses the immune system to fight cancer.
What happens after immunotherapy ends?
After immunotherapy ends, patients may be monitored for response. Or, alternative treatments might be considered.
What if Lonsurf doesn’t work?
If Lonsurf doesn’t work, other chemotherapy regimens or clinical trials might be considered.
What happens when abiraterone stops working?
If abiraterone stops working, other hormone therapies or chemotherapy might be considered.
What are the signs Nivolumab is working?
Signs Nivolumab is working include tumor shrinkage, improved symptoms, or lab evidence of response.
When chemo stops working?
When chemotherapy stops working, options include targeted therapy, radiation therapy, or clinical trials.
References
- National Cancer Institute. (n.d.). Immunotherapy to treat cancer.https://www.cancer.gov/about-cancer/treatment/types/immunotherapy
- Sharma, P., & Allison, J. P. (2015). The future of immune checkpoint therapy. Science, 348(6230), 56“61.https://doi.org/10.1126/science.aaa8155
- Stenger, M. M., & Hinchcliff, M. D. (2020). Management of immune-related adverse events with immune checkpoint inhibitors. Journal of Clinical Oncology, 38(18), 2056“2067.https://doi.org/10.1200/JCO.19.02047



































