Last Updated on November 27, 2025 by Bilal Hasdemir

We know how vital heart health is. At Liv Hospital, we’re dedicated to top-notch care for vascular disease patients. Atherosclerosis of the thoracic aorta is a serious issue where plaque accumulates in the aorta, posing severe risks.
This disease gets worse over time and can lead to strokes and aneurysms. Catching it early and treating it quickly is key to avoiding these dangers. We focus on patient care at Liv Hospital, aiming for the best results for our patients.
Key Takeaways
- Understanding atherosclerosis of the thoracic aorta is vital for maintaining cardiovascular health.
- The condition is a progressive disease that can lead to severe complications if left untreated.
- Early detection and treatment are critical to preventing embolic stroke and aneurysm formation.
- Liv Hospital is committed to providing advanced diagnostics and patient-centered care.
- Timely intervention is essential for ensuring the best possible outcomes for patients.
Understanding Atherosclerosis of the Thoracic Aorta

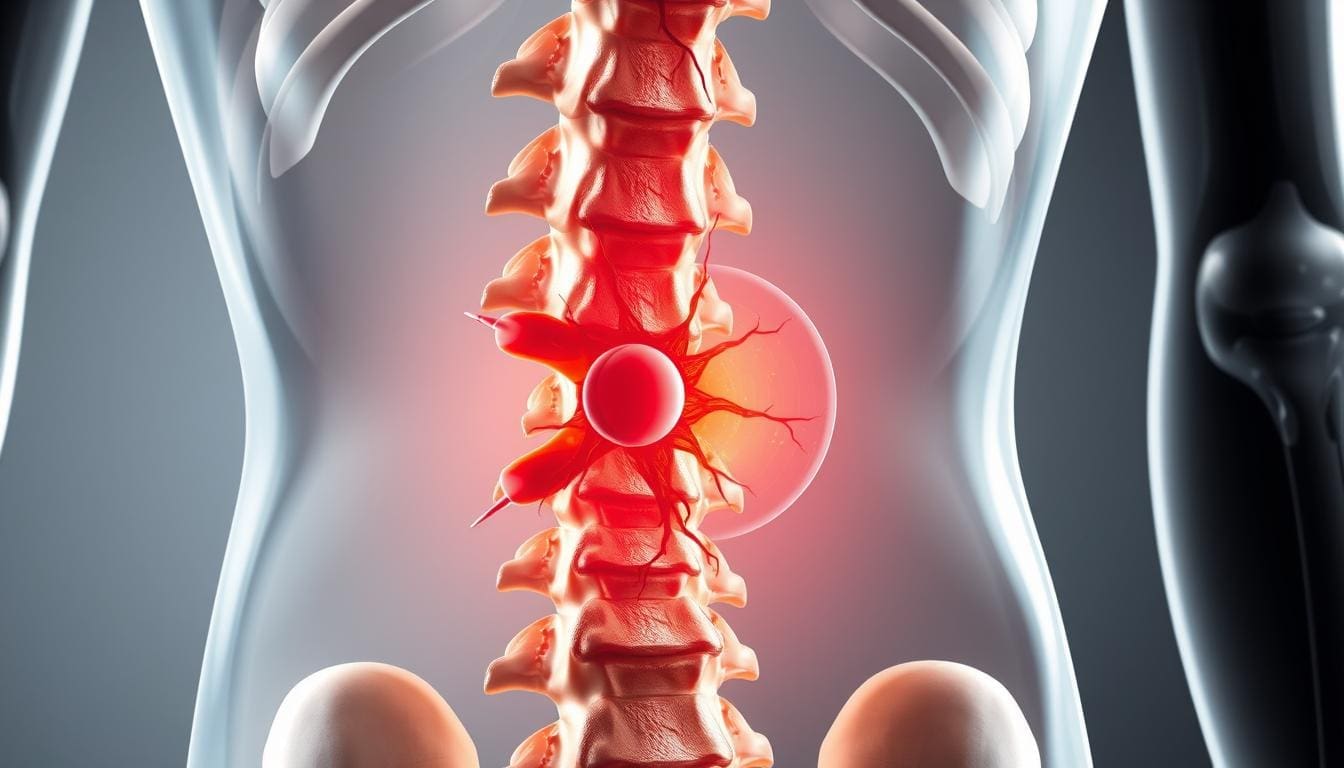
To understand atherosclerosis of the thoracic aorta, we need to know how it works and what causes it. This condition happens when plaque builds up in the arteries. This buildup can lead to heart disease.
Definition and Pathophysiology
Atherosclerosis in the thoracic aorta means plaque builds up in the aorta’s wall. This makes the aorta less strong and less able to work right. It starts with damage to the inner lining of the artery, then lipids and inflammatory cells get in.
Over time, this leads to atherosclerotic lesions. These can get worse with calcification, ulceration, or blood clots.
The reasons for thoracic aortic atherosclerosis are complex. They include problems with lipid metabolism, inflammation, and changes in the blood vessels. Many factors can make this disease worse, like high blood pressure, high cholesterol, diabetes, and smoking.
Prevalence and Age-Related Incidence
Atherosclerosis in the thoracic aorta gets more common with age. It’s a big worry for older people. Research shows that more people get this condition after 40, and even more after 60.
| Age Group | Prevalence of Thoracic Aortic Atherosclerosis |
| 40-49 years | 15% |
| 50-59 years | 30% |
| 60-69 years | 50% |
| 70+ years | 65% |
This table shows how atherosclerosis in the thoracic aorta gets more common with age. It points out that age is a big risk factor we can’t change.
Pathophysiology of Aortic Plaque Formation

Understanding how aortic plaque forms is key to knowing how atherosclerosis grows. Aortic plaque formation is a complex process. It involves many cellular, molecular, and hemodynamic factors.
Initiation of Plaque Development
The start of plaque development in the thoracic aorta is linked to endothelial dysfunction. This makes the artery wall more open and attracts lipids and inflammatory cells. Low-density lipoprotein (LDL) cholesterol is important here. It builds up in the artery wall and gets oxidized, causing inflammation.
Progression of Atherosclerotic Lesions
As atherosclerotic lesions grow, they become more complex. They start to hold smooth muscle cells, macrophages, and lymphocytes. The lesions can change in many ways, like calcifying, ulcerating, or hemorrhaging. This makes them unstable. Inflammation is a big factor in this growth, with pro-inflammatory cytokines helping plaques grow and destabilize.
Classification of Atherosclerotic Severity
Atherosclerotic lesions are sorted by their makeup and shape. The American Heart Association has a system for this. It goes from early fatty streaks to advanced complicated lesions. Knowing the severity and type of lesions is key for assessing risk and planning treatment.
The formation of aortic plaque is a complex process. It’s influenced by many factors, like lipid metabolism, inflammation, and blood flow. By understanding these, we can see how complex atherosclerosis is. This shows why we need a full approach to managing it.
Risk Factors for Thoracic Aortic Atherosclerosis
Thoracic aortic atherosclerosis is caused by several risk factors. These can be changed or not. Knowing them helps prevent and manage the disease.
Non-Modifiable Risk Factors
Non-modifiable risk factors are things we can’t change. These include:
- Age: The risk of thoracic aortic atherosclerosis grows with age.
- Genetics: Family history greatly affects the risk of atherosclerosis.
- Gender: Some studies show gender differences in atherosclerosis incidence.
Modifiable Risk Factors
Changing these risk factors can slow down thoracic aortic atherosclerosis:
- Smoking: Smoking is a big risk factor for atherosclerosis.
- Hypertension: High blood pressure helps atherosclerotic plaques grow.
- Dyslipidemia: Blood lipid imbalances speed up plaque formation.
- Diabetes Mellitus: Diabetes raises the risk of atherosclerosis.
Comorbid Conditions
Some conditions can also affect thoracic aortic atherosclerosis:
- Chronic Kidney Disease: Poor kidney function increases atherosclerosis risk.
- Inflammatory Diseases: Diseases like rheumatoid arthritis can lead to atherosclerosis.
Healthcare providers can create better prevention and treatment plans by understanding these risk factors and conditions.
Clinical Presentation and Symptoms
It’s important to know how thoracic aortic atherosclerosis shows up early. This disease can be silent in its early days or cause severe symptoms later on.
Asymptomatic Presentation in Mild Disease
In its early stages, thoracic aortic atherosclerosis often doesn’t show symptoms. This makes it hard to catch without special tests. We usually find it by accident when doing tests for heart issues.
Symptomatic Manifestations in Moderate Disease
When the disease gets a bit worse, symptoms start to appear. People might feel chest pain or discomfort because of less blood flow. They could also have transient ischemic attacks (TIAs) or small strokes if debris from the aorta goes to the brain.
Advanced Disease Presentations
At its worst, thoracic aortic atherosclerosis can cause serious problems. These include big embolic events, aortic aneurysms, or aortic dissections. Symptoms can be very bad, like severe pain, unstable blood pressure, or failing organs.
| Disease Stage | Common Symptoms | Potential Complications |
| Mild | Asymptomatic | Incidental discovery during imaging |
| Moderate | Chest pain, TIAs, minor strokes | Embolization to peripheral or cerebral arteries |
| Advanced | Severe pain, hemodynamic instability | Aortic aneurysm, dissection, significant embolic events |
It’s key to know the signs and risks of thoracic aortic atherosclerosis for quick action. We should think of this disease when patients show heart symptoms, and they have risk factors for atherosclerosis.
Diagnostic Approaches for Thoracic Aortic Atherosclerosis
Healthcare providers use many tools to diagnose thoracic aortic atherosclerosis. They use advanced imaging techniques. This condition is complex and needs a detailed approach to understand the atherosclerotic plaque in the thoracic aorta.
Imaging Techniques
Imaging is key in diagnosing thoracic aortic atherosclerosis. Some common imaging methods include:
- Transesophageal Echocardiography (TEE): Gives clear images of the aorta. It helps see how thick the plaque is and its shape.
- Computed Tomography (CT) Angiography: Shows detailed pictures of the aorta and its branches. It helps find and measure atherosclerotic plaque.
- Magnetic Resonance Imaging (MRI): Allows seeing the aortic wall and plaque without using harmful radiation.
Laboratory Assessment
Laboratory tests are important for checking cardiovascular risk. They help find factors that might lead to atherosclerosis. Key tests include:
- Lipid Profile: Shows if there’s dyslipidemia, a big risk for atherosclerosis.
- C-Reactive Protein (CRP): High CRP levels mean there’s inflammation. This is linked to atherosclerotic disease.
- Blood Glucose: Helps find diabetes, a major risk for atherosclerosis.
Atheromatous Aorta Image Analysis
Looking at images from different imaging methods is vital. It helps see how bad the atherosclerosis is. They check the plaque’s thickness, type, and if it’s ulcerated. This helps predict the risk of complications.
By using imaging, lab tests, and detailed image analysis, doctors can accurately diagnose thoracic aortic atherosclerosis. They can then plan the best treatment.
Thoracic Aortic Atherosclerosis and Stroke Risk
The link between thoracic aortic atherosclerosis and stroke risk is a big concern in heart health. Atherosclerosis in the thoracic aorta is not just a local issue. It affects heart health overall, raising the risk of stroke.
Aortic Arch Atheroma as an Embolic Source
Aortic arch atheroma is a known risk factor for stroke. Atheromatous lesions in the aortic arch can cause thrombi. These thrombi can travel to the brain, leading to ischemic stroke. The severity of aortic arch atheroma is directly linked to stroke risk. Accurate diagnosis and risk assessment are key.
Research shows that atheroma thickness and complexity predict stroke risk. Patients with thicker, more complex plaques face a higher risk of embolic events. So, identifying and characterizing aortic arch atheroma is vital for preventing strokes.
Risk Stratification and Prevention Strategies
Effective risk stratification combines imaging and clinical assessment. We use imaging like transesophageal echocardiography (TEE) to check aortic arch atheroma. TEE is great for detailed images of the aortic arch and spotting complex lesions.
| Risk Factor | Description | Impact on Stroke Risk |
| Aortic Arch Atheroma Thickness | Thickness of the atheromatous plaque | Increased thickness correlates with higher stroke risk |
| Complexity of Atheroma | Presence of ulceration, mobile components | Complex lesions are associated with higher embolic risk |
| Patient Age and Comorbidities | Presence of hypertension, diabetes, etc. | Comorbid conditions increase overall cardiovascular risk |
Prevention strategies aim to lower embolic event risk. We use anticoagulation therapy, manage risk factors like hypertension, and promote lifestyle changes. Statins and antiplatelet agents help reduce stroke risk in patients with significant aortic arch atheroma. Patient education and treatment adherence are also key for stroke prevention.
Complications of Untreated Aortic Atherosclerotic Disease
Untreated aortic atherosclerosis can cause severe and life-threatening problems. It’s important to treat this condition early to avoid serious issues.
Embolic Events
One big risk is embolic events. Emboli can break off and travel to other parts of the body. This can damage organs or cause dysfunction.
For example, a stroke can happen if an embolus goes to the brain. Limb ischemia can occur if it goes to the arteries in the limbs.
Several factors can increase the risk of embolic events. These include the size and type of plaque, and other heart disease risk factors.
| Risk Factor | Description | Impact on Embolic Risk |
| Plaque Size | Large plaques are more likely to be a source of emboli. | High |
| Plaque Composition | Plaques with a high lipid content are more prone to rupture. | High |
| Cardiovascular Risk Factors | Presence of hypertension, diabetes, and smoking increases overall cardiovascular risk. | Moderate to High |
Aneurysm Formation and Progression
Aneurysms can also form and grow if atherosclerosis is not treated. The weakened aortic wall can lead to aneurysmal dilatation. This is a risk of rupture if not treated.
Monitoring and managing aneurysm growth is key to prevent rupture. Regular imaging studies and tracking the size and growth rate are important.
Other Vascular Complications
Untreated aortic atherosclerosis can also cause other vascular problems. These include renal artery stenosis, peripheral artery disease, and mesenteric ischemia.
It’s important to manage atherosclerotic disease comprehensively. This can help reduce these risks and improve patient outcomes.
Treatment Strategies for Atherosclerosis of the Thoracic Aorta
Managing thoracic aortic atherosclerosis requires a mix of medical, surgical, and new treatments. Each patient is different, so we tailor our treatment plans to fit their needs.
Medical Management
Medical treatment is often the first step for thoracic aortic atherosclerosis. It aims to lower risk factors and slow the disease’s growth. Statins help lower cholesterol, and antiplatelet therapy prevents blood clots. It’s also key to manage high blood pressure and diabetes.
We stress the importance of lifestyle changes too. Quitting smoking, eating right, and exercising help keep your heart healthy.
Surgical Interventions
When medical treatment isn’t enough, surgery might be needed. Endovascular repair is a less invasive option for some aortic issues. Open surgical repair is used for more serious cases, where the aorta needs to be replaced or fixed.
Choosing between these surgeries depends on the patient’s health, the disease’s extent, and other health issues.
Emerging Therapeutic Approaches
New treatments for thoracic aortic atherosclerosis are being researched. Novel pharmacotherapies might offer better disease management. Also, new endovascular techniques could lead to better surgical results.
We’re always learning more about thoracic aortic atherosclerosis. Our goal is to provide the latest and most effective treatments.
Monitoring and Long-Term Management
Managing thoracic aortic atherosclerosis requires a detailed plan. This plan includes monitoring, making lifestyle changes, and using medical treatments. It’s key to stop complications and help patients get better.
Follow-up Protocols Based on Disease Severity
Follow-up plans for thoracic aortic atherosclerosis depend on how severe the disease is. For those with mild atherosclerosis, yearly imaging and check-ups are often enough.
But, if the disease is more serious, doctors might need to see patients more often. This could be every 6 to 12 months to keep track of how the disease is growing and change treatment plans as needed.
| Disease Severity | Follow-up Frequency | Key Components of Follow-up |
| Mild | Annually | Imaging studies, clinical assessment |
| Moderate | Every 6-12 months | Imaging studies, risk factor assessment, medication review |
| Severe | Every 3-6 months | Imaging studies, clinical assessment, adjustment of treatment plans |
Patient Education and Lifestyle Modifications
Teaching patients about their condition is vital. It helps them understand the importance of following their treatment plans and making lifestyle changes. These changes can slow down the disease’s growth.
Important lifestyle changes include eating better, being more active, quitting smoking, and managing stress. By making these changes, patients can lower their risk of the disease getting worse and its complications.
Quality of Life Considerations
When managing thoracic aortic atherosclerosis, it’s important to think about the patient’s quality of life. This means treating the disease but also looking at the psychological and social effects it has.
Doctors should work with patients to create care plans that fit their needs. These plans should balance treating the disease with improving the patient’s quality of life. This ensures patients get care that helps them feel better overall.
Conclusion
We’ve looked into atherosclerosis of the thoracic aorta, a disease where plaque builds up in the aorta. It’s important to know the risk factors and how to diagnose it. This knowledge helps in managing the disease effectively.
We talked about how lifestyle changes and medical treatments can help slow down the disease. By tackling risk factors and using the right tests, we can lower the chance of serious problems like stroke and peripheral artery disease.
Managing thoracic aortic atherosclerosis requires a full approach. We need to teach patients about living healthy and regular check-ups. This helps stop the disease from getting worse.
This summary shows we need a wide strategy to tackle this complex disease. It’s all about improving patient care and outcomes.
FAQ
What is atherosclerosis of the thoracic aorta?
Atherosclerosis of the thoracic aorta is a disease where plaque builds up in the aorta. This can cause serious problems, like embolic events and aneurysms.
What are the risk factors for developing thoracic aortic atherosclerosis?
Risk factors include age, family history, and conditions like hypertension and hyperlipidemia. Smoking, diabetes, and obesity also increase the risk.
How is thoracic aortic atherosclerosis diagnosed?
Doctors use imaging like transesophageal echocardiography (TEE) and CT scans. They also check blood work to assess heart risk.
What are the symptoms of thoracic aortic atherosclerosis?
Symptoms vary. Mild cases might not show symptoms. But severe cases can cause chest pain, back pain, and other serious issues.
How does thoracic aortic atherosclerosis increase the risk of stroke?
Aortic arch atheroma can send emboli to the brain, leading to stroke. It’s important to manage this risk through prevention and treatment.
What are the treatment options for atherosclerosis of the thoracic aorta?
Treatments include medications to control risk factors and surgery for complications. New treatments aim to reduce plaque.
How is thoracic aortic atherosclerosis monitored and managed long-term?
Long-term care involves regular check-ups and patient education. It also includes lifestyle changes to maintain quality of life.
Can thoracic aortic atherosclerosis be prevented?
While some risks can’t be changed, managing others through lifestyle and medicine can prevent or slow the disease.
What are the potentially complications of untreated thoracic aortic atherosclerosis?
Untreated disease can lead to serious issues like embolic events and aneurysms. Early detection and treatment are key.
References
National Heart, Lung, and Blood Institute (NHLBI): Atherosclerosis Diagnosis