The menstrual cycle is a complex process that happens every month in women of childbearing age. It involves different phases that work together. These phases prepare the body for pregnancy, affect energy and mood, and impact overall health.
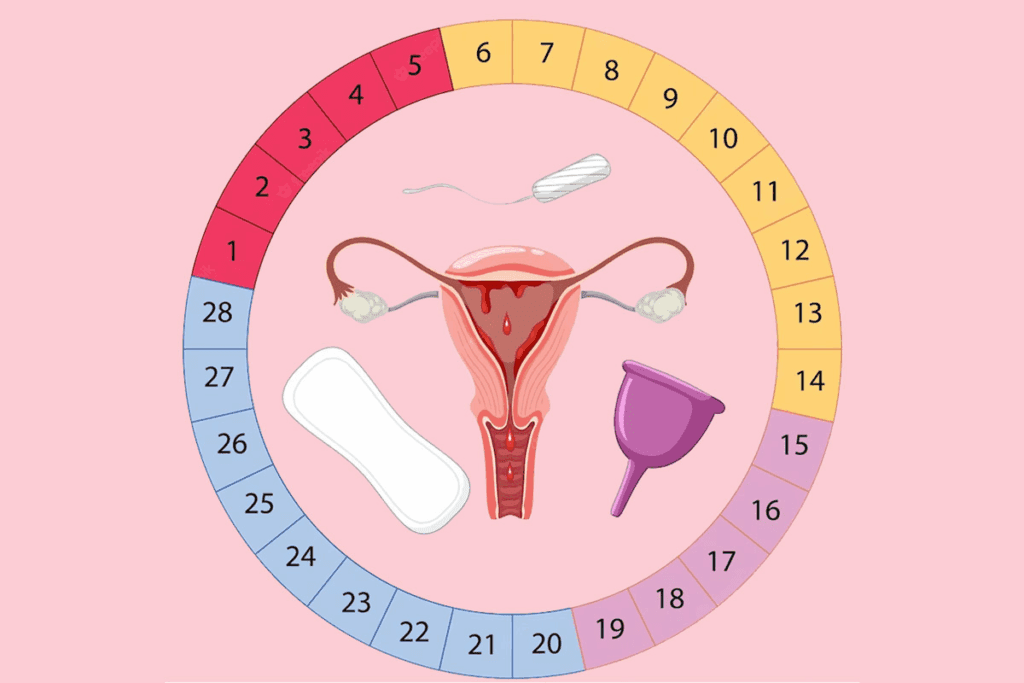
Regulated by various hormones, the menstrual cycle has four main phases. These are the menstrual phase, the follicular phase, the ovulatory phase, and the luteal phase. Knowing about these phases helps women track their health and understand body changes.
Understanding the different phases helps women manage their health better. It lets them make informed choices about their well-being. Dive into the 4 stages of menstrual cycle—know your body’s monthly rhythm for better health management and planning.
Key Takeaways
- The menstrual cycle is a complex process regulated by hormones.
- There are four distinct phases in the menstrual cycle.
- Understanding these phases can help women track their reproductive health.
- Recognizing the phases can empower women to make informed decisions about their health.
- The menstrual cycle influences energy levels, mood, and overall health.
The Biological Importance of Menstrual Cycles
Menstrual cycles are very important for women’s health. They are a complex process that helps keep women fertile. Each phase of the cycle is vital for reproductive health.
“A normal menstrual cycle is a sign of a woman’s overall health and fertility,” says Medical Expert. He stresses the need to know about your cycle.
Reproductive Function and Fertility
The menstrual cycle is key for reproductive health and fertility. It prepares the body for pregnancy. The reproductive system releases an egg during ovulation, ready for fertilization.
Tracking your cycle can give you insights into your health. Medical Expert’s normal for you. This can help spot any problems early.
Cycle Length Variations (21-35 Days)
Menstrual cycle length varies from 21 to 35 days. Age, lifestyle, and health can affect it. Knowing these variations is important for recognizing what’s normal.
While cycle length can change, big changes may mean health issues. So, knowing your cycle and its patterns is key for reproductive health.
In conclusion, menstrual cycles are essential for women’s health. They affect fertility and overall well-being. Understanding menstrual cycles helps women manage their reproductive health better.
The 4 Stages of Menstrual Cycle

The menstrual cycle has four stages, each important for reproductive health. Knowing these stages helps women take care of their health.
Sequential Process Overview
The cycle includes menstruation, the follicular phase, ovulation, and the luteal phase. Each stage is connected and prepares the body for pregnancy.
Menstruation is the first stage, lasting 3 to 7 days. It’s when the uterine lining is shed if there’s no pregnancy. Then comes the follicular phase, which starts with menstruation and ends with ovulation. This phase prepares the body to release an egg.
Ovulation is when the egg is released into the fallopian tube. It happens around the cycle’s midpoint, making a woman most fertile.
The luteal phase follows ovulation and lasts until menstruation starts. The empty follicle forms the corpus luteum, which makes progesterone. This hormone prepares the uterine lining for pregnancy.
Hormonal Orchestration
Hormones like estrogen and progesterone control the cycle. Estrogen grows the uterine lining during the follicular phase. Progesterone keeps the lining ready for pregnancy in the luteal phase.
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary gland are key. The LH surge makes the egg release from the ovary.
Cycle Timeline Visualization
Seeing the menstrual cycle helps understand its stages and timing. The cycle is usually 21 to 35 days long, with ovulation in the middle.
Knowing the cycle’s stages and hormonal changes helps women manage their health. It also helps spot any irregularities.
Hormonal Regulation Throughout the Cycle
The menstrual cycle is a complex dance of hormones. It prepares the body for pregnancy. Many hormones work together in each stage of the cycle.
Follicle-Stimulating Hormone (FSH)
Follicle-Stimulating Hormone (FSH) is key in the menstrual cycle, mainly in the follicular phase. It helps ovarian follicles grow, which hold eggs. FSH levels go up, helping 5 to 20 follicles grow, but only one will release an egg.
Role of FSH: FSH is vital for follicle growth and estrogen production. As follicles grow, they make estrogen. This estrogen then stops FSH production, creating a feedback loop.
Luteinizing Hormone (LH)
Luteinizing Hormone (LH) spikes mid-cycle, causing ovulation. This surge lets the dominant follicle release an egg. LH also helps form the corpus luteum after ovulation.
Role of LH: LH is key for ovulation and corpus luteum formation. The corpus luteum makes progesterone, preparing the uterine lining for pregnancy.
Estrogen and Progesterone Interplay
Estrogen and progesterone work together in the menstrual cycle. Estrogen levels rise in the follicular phase, thickening the uterine lining. After ovulation, progesterone levels increase, further preparing the uterine lining for a fertilized egg.
Interplay: The balance between estrogen and progesterone is critical. Estrogen grows the uterine lining, while progesterone maintains it. If pregnancy doesn’t happen, the drop in progesterone leads to menstruation.
Hormone | Primary Function | Phase |
FSH | Follicular development | Follicular |
LH | Ovulation, Corpus Luteum formation | Ovulation |
Estrogen | Uterine lining thickening | Follicular |
Progesterone | Uterine lining maintenance | Luteal |
As shown in the table, each hormone has a unique role and phase in the menstrual cycle. Knowing these hormonal changes can help understand reproductive health and fertility.
Medical Expert, “Hormonal changes in the menstrual cycle greatly affect women’s health. They influence fertility and overall well-being.”
“The menstrual cycle is a complex interplay of hormones, and understanding this can help women better manage their reproductive health.” – Medical Expert
Understanding the hormonal regulation of the menstrual cycle helps women understand their bodies better. This knowledge can guide them in making informed decisions about their reproductive health.
Phase 1: Menstruation Explained
Let’s start with menstruation, a key part of female health. It’s the first step in the menstrual cycle, starting a new cycle.
Uterine Lining Shedding Process
Menstruation is when the uterine lining sheds. This happens because progesterone levels drop if there’s no pregnancy. It’s a natural way to get ready for a new cycle.
Duration and Blood Loss (3-7 Days)
The menstrual phase lasts 3 to 7 days. The most blood is lost in the first two days. On average, women lose 2-3 tablespoons of blood.
Using the right sanitary products and staying clean is key to managing blood loss.
Common Symptoms and Management
During menstruation, women often feel cramps, bloating, tiredness, and mood swings. Medical Expert-rich foods and doing light exercise to help. Over-the-counter pain relievers can also ease cramps.
Understanding what happens during menstruation and making healthy choices can help manage symptoms. This improves overall well-being during this time.
Phase 2: The Follicular Phase
After menstruation, the follicular phase starts. It’s filled with big hormonal and body changes. This phase is key for ovulation and getting pregnant.
Timing and Duration
The follicular phase lasts about 13 to 14 days. It starts right after your period and ends with ovulation.
Follicle Development
The pituitary gland releases Follicle-Stimulating Hormone (FSH) during this time. It makes follicles in the ovaries grow. Usually, 5 to 20 follicles start, but only one will be ready to release an egg.
Estrogen Rise and Endometrial Thickening
As follicles grow, they make estrogen. This hormone makes the uterine lining get thicker. The thicker lining is ready to support a fertilized egg. Estrogen also changes cervical mucus, helping sperm get in.
Knowing about the follicular phase is important for women wanting to get pregnant. It shows when they can get fertilized. By tracking this phase and its signs, women can improve their chances of getting pregnant.
Phase 3: Ovulation – The Fertility Window
Ovulation is a key part of the menstrual cycle, important for fertility. It’s when the body releases an egg from the ovary, ready for fertilization. This is vital for making babies and involves many hormones working together.
LH Surge and Egg Release
The luteinizing hormone (LH) surge is a big event that starts ovulation. When LH levels go up, it makes the egg come out. This usually happens 24-36 hours before ovulation, marking the fertility window.
Medical Expert, hormone levels go up. This can make you feel better, more energetic, and more interested in sex. These changes can improve your mood and energy.
Physical Signs of Ovulation
There are signs that ovulation is happening. These include:
- Changes in cervical mucus, making it easier for sperm to move
- A slight rise in basal body temperature
- Mild pelvic pain or cramping, called mittelschmerz
- Feeling more interested in sex because of hormone changes
Fertility Tracking Methods
Knowing when you ovulate is key for getting pregnant or avoiding it. There are ways to track ovulation:
- Monitoring basal body temperature
- Watching cervical mucus
- Using ovulation predictor kits to find the LH surge
- Fertility apps that guess when you’ll ovulate based on your cycle
By paying attention to ovulation signs, you can manage your fertility. This is helpful whether you’re trying to get pregnant or not.
Phase 4: The Luteal Phase
The luteal phase is a key part of the menstrual cycle. It happens after ovulation and gets the uterus ready for pregnancy. This phase sees big changes in hormones that can affect how we feel and our bodies.
Corpus Luteum Formation
After ovulation, the empty follicle turns into the corpus luteum. This structure makes progesterone. Progesterone helps make the uterine lining thick, ready for a fertilized egg. If a woman gets pregnant, the corpus luteum keeps making progesterone until the placenta takes over.
Progesterone Dominance
In the luteal phase, progesterone levels go up. This hormone can slow down the intestines, causing bloating. It also raises body temperature a bit. These changes can affect daily life, so it’s important to understand and manage them.
Premenstrual Syndrome (PMS) Explained
Many women get premenstrual syndrome (PMS) during the luteal phase. Symptoms include mood swings, tender breasts, and feeling tired. PMS is linked to hormonal changes, like the drop in estrogen and progesterone if there’s no pregnancy. To deal with PMS, women can try changing their diet and exercising more. Sometimes, medical help is needed too.
Knowing about the luteal phase and its effects can help women manage their symptoms better. By understanding PMS and the role of progesterone, women can take steps to lessen its impact.
Physical Changes Throughout the Menstrual Cycle
As we go through the menstrual cycle, we notice many physical changes. These changes happen because of hormone shifts. They help us know what phase of the cycle we’re in.
Cervical Mucus Variations
Cervical mucus changes a lot during the cycle. It’s important for fertility. When it’s more fluid, it helps sperm move, making it easier to get pregnant.
Watching cervical mucus can help track when you’re most fertile. Women can see changes in its texture, color, and amount. This gives clues about their reproductive health.
Basal Body Temperature Patterns
Basal body temperature also changes with the cycle. It usually goes down before ovulation and up after. This helps women find their fertile time and understand their cycle.
The temperature change is small, about 1 degree Fahrenheit. But tracking it can show when ovulation happens.
Breast Tenderness and Other Physical Indicators
Many women feel breast tenderness during their cycle. This is often because of hormone changes. Symptoms like bloating and cramps can also change from cycle to cycle.
Other signs include changes in energy, skin sensitivity, and digestion. Knowing these changes helps women manage their symptoms and stay healthy.
Emotional and Mental Changes During Cycle Phases
Hormonal changes in the menstrual cycle can cause emotional and mental symptoms. Women go through different phases, leading to significant changes in their lives.
Effects on Mood
Estrogen and progesterone levels affect mood. Medical Expert, “hormone levels can change serotonin levels, causing mental or emotional symptoms.” Rising estrogen in the follicular phase boosts well-being and energy.
In the luteal phase, progesterone increases, leading to calmness but also anxiety or irritability in some.
Here’s a look at emotional changes in the cycle phases:
Cycle Phase | Hormonal Changes | Common Emotional Symptoms |
Menstruation | Low estrogen and progesterone | Irritability, sadness |
Follicular Phase | Rising estrogen | Increased energy, improved mood |
Ovulation | Peak estrogen, LH surge | Confidence, sociability |
Luteal Phase | Rising progesterone | Anxiety, irritability, calmness |
Energy Level Fluctuations
Energy levels change in the menstrual cycle. In the follicular phase, women often feel more energetic as estrogen rises. In the luteal phase, some may feel tired due to progesterone.
Cognitive Function Throughout the Cycle
Hormonal changes can affect concentration and memory. Estrogen may improve cognitive functions, making women feel sharper in the follicular phase.
“Understanding these changes can empower women to manage their emotional and mental health more effectively throughout their menstrual cycle.”
Knowing about emotional and mental changes in the menstrual cycle helps women prepare and manage symptoms. This improves their overall well-being.
Menstrual Cycle Health and Lifestyle Considerations
Women can manage their menstrual health by making smart choices about diet, exercise, and sleep. By adapting their lifestyle, they can ease symptoms and feel better overall.
Nutrition Recommendations for Each Phase
Nutrition is key for menstrual health. In the follicular phase, eat foods full of antioxidants and omega-3 fatty acids to help with hormone balance. For the luteal phase, choose complex carbs and magnesium-rich foods to ease PMS symptoms.
Medical Expert. For example, more iron during menstruation helps replace lost iron. Also, calcium-rich foods are good for bones all cycle long.
Exercise Adaptations Throughout the Cycle
Exercise is vital for menstrual health. During menstruation, try yoga or light cardio to ease cramps and boost mood. The follicular phase is best for more energetic workouts.
At ovulation, balance workouts with rest. In the luteal phase, you might feel less energetic, so stick to easier activities.
Sleep Quality and Hormonal Fluctuations
Sleep quality greatly affects menstrual health. Hormones change throughout the cycle, affecting sleep. In the luteal phase, progesterone levels can make you sleepier, while some might have trouble sleeping.
Keep a regular sleep schedule and a calming bedtime routine. Avoid caffeine and electronic screens before bed for better sleep.
Menstrual Cycle Irregularities and Causes
It’s important for women to know about menstrual cycle irregularities. These issues can affect health and reproductive well-being. We’ll look at common patterns, medical conditions, and how age changes menstrual cycles.
Identifying Common Irregularity Patterns
Irregularities can show up in many ways, like changes in cycle length or bleeding. Hormonal imbalances, stress, and other factors can cause these issues. Spotting these patterns is key to getting the right medical help.
Medical Conditions Affecting Menstrual Cycles
Some health issues, like PCOS, thyroid problems, and uterine fibroids, can mess with menstrual cycles. Medical Expert, see a doctor to check for underlying problems.
Age-Related Changes in Menstrual Cycles
Menstrual cycles change a lot from puberty to menopause. Knowing these changes is important for managing menstrual health. As women get closer to menopause, hormonal shifts can cause irregular periods and other symptoms.
Understanding menstrual irregularities helps women take care of their health. If irregularities last or are severe, getting medical advice is a good step.
FAQ
What are the 4 stages of the menstrual cycle?
The menstrual cycle has four stages: menstruation, the follicular phase, ovulation, and the luteal phase. These stages are controlled by hormones. They are key for reproductive health.
What is the follicular phase, and how long does it last?
The follicular phase comes after menstruation. It’s when follicles in the ovaries grow. It usually lasts 13-14 days, but can vary.
What is ovulation, and how is it triggered?
Ovulation is when a mature egg is released from the ovary. It’s triggered by a surge in luteinizing hormone (LH). It happens around the cycle’s midpoint, making it the most fertile time.
What are the symptoms of premenstrual syndrome (PMS), and how can they be managed?
PMS symptoms include mood swings, breast tenderness, and bloating. To manage them, try lifestyle changes like exercise, better nutrition, and stress management.
How do hormonal fluctuations affect mood and energy levels throughout the menstrual cycle?
Hormonal changes can affect mood, energy, and brain function. Changes in estrogen and progesterone levels influence neurotransmitters. This leads to emotional and physical symptoms.
What lifestyle changes can improve menstrual cycle health?
Improving menstrual health involves nutrition, exercise, and sleep. Eating well, staying active, and getting enough rest can help manage symptoms and regulate the cycle.
What are common irregularity patterns in the menstrual cycle, and what causes them?
Irregularities include changes in cycle length, heavy or light bleeding, and anovulatory cycles. Causes include hormonal imbalances and medical conditions like PCOS.
How do medical conditions affect the menstrual cycle?
Medical conditions like thyroid disorders, PCOS, and endometriosis can affect menstrual regularity and symptoms. They can also impact reproductive health.
How does age affect the menstrual cycle, from puberty to perimenopause?
The menstrual cycle changes with age. Puberty starts menstruation, while perimenopause marks the transition to menopause. Hormonal changes and cycle irregularities are common during these times.
What are the physical changes that occur during the menstrual cycle?
Physical changes include cervical mucus variations, basal body temperature shifts, and breast tenderness. These changes signal different cycle phases.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK500020/








