Feeling sharp or aching ovarian pain after menopause can be scary. You might think that ending menstruation would mean less pain. But for many, pelvic discomfort keeps coming back. Experiencing ovary pain after menopause? Don’t ignore it. Learn 5 alarming causes and when you must see a doctor immediately.
About 15 percent of women deal with sharp pelvic pain after menopause. This pain can really upset them. AtLiv Hospital, we focus on helping women with gynecological issues. We use the latest tests and care plans to find out why you might be feeling pain.
We know that persistent discomfort might mean there’s something serious going on. In this article, we’ll look at why you might feel pain in your ovaries after menopause. We’ll also talk about how to treat it, so you can understand what’s happening.
Key Takeaways
- Ovarian pain after menopause affects approximately 15 percent of women.
- Postmenopausal ovary pain can be a sign of underlying conditions.
- Liv Hospital offers comprehensive gynecological care for postmenopausal women.
- Advanced diagnostic protocols are used to identify the root cause of ovarian discomfort.
- Patient-centered approaches ensure personalized care for each patient.
The Reality of Ovary Pain After Menopause
Understanding ovarian pain after menopause means looking at the body’s changes during this time. Menopause ends a woman’s childbearing years and can cause symptoms like pelvic pain.
Pelvic pain in menopause is discomfort in the lower belly, pelvis, or reproductive areas. It can be mild or severe and may come and go. It’s important to know that some changes are normal, but others might need medical help.
Prevalence Statistics in Postmenopausal Women
Many postmenopausal women feel ovarian pain. Research shows 2.5 to 14 percent get ovarian cysts, which can hurt. Knowing this helps us see that ovarian pain is common and should be checked out.
It’s key for doctors to find out why women have pain. This helps them treat it right.
Distinguishing Normal Changes from Concerning Symptoms
It’s important to tell normal menopause changes from serious symptoms. Normal changes might include some pelvic floor relaxation or minor discomfort. But, severe or lasting pain is not normal.
Signs that need quick doctor visits include severe pain, pain that lasts, or pain with fever, vaginal bleeding, or trouble peeing. These could mean problems like ovarian cysts, pelvic inflammatory disease, or other gynecological issues.
By understanding ovarian pain after menopause, women and doctors can find causes and treat them. This improves life for postmenopausal women.
Physiological Changes in the Reproductive System After Menopause
Menopause brings big changes to the female body. Women go through many hormonal shifts as they enter postmenopause. These changes affect their reproductive health and overall well-being.
Hormonal Shifts and Their Effects on Ovarian Tissue
One big change is the drop in estrogen levels. Estrogen keeps the vaginal walls healthy and strong. Without enough estrogen, the vaginal tissue gets thinner, drier, and less elastic. This is called vaginal atrophy.
Vaginal atrophy can cause discomfort and pain during sex. It also raises the risk of infections.
Estrogen levels also drop in the ovaries. Even though the ovaries stop making eggs, they keep making some hormones. But the drop in estrogen can cause discomfort or pain in the ovaries.
“The decline in estrogen levels during menopause has a profound impact on the female reproductive system, leading to changes that can affect a woman’s quality of life.”
Genitourinary Syndrome of Menopause and Pelvic Discomfort
Genitourinary syndrome of menopause (GSM) includes symptoms like vaginal dryness and pain during sex. It also causes urinary problems like needing to pee a lot. These symptoms lead to pelvic discomfort.
The main cause of GSM and pelvic discomfort is the drop in estrogen. Without enough estrogen, the vaginal walls are more prone to irritation and pain.
Symptoms | Causes | Effects |
Vaginal dryness, itching | Decline in estrogen levels | Discomfort, pain during intercourse |
Urinary frequency, urgency | Estrogen deficiency | Incontinence, pelvic discomfort |
Pelvic pain | Hormonal changes, GSM | Impact on quality of life |
It’s important to understand these changes to manage symptoms and improve life for postmenopausal women. Healthcare providers can offer treatments to help with discomfort and pain.
Common Gynecological Causes of Ovary Pain After Menopause
Ovarian pain after menopause can come from several gynecological causes. Menopause doesn’t mean a woman is safe from ovarian problems. Knowing these causes helps in finding the right treatment.
Ovarian Cysts in Postmenopausal Women
Ovarian cysts can happen even after menopause. Most are harmless, but they can cause pain. Simple cysts are filled with fluid and often go away on their own. Complex cysts might need more attention because they could be cancerous.
It’s wise to keep an eye on these cysts with ultrasound tests. Sometimes, removing the cyst is needed if it’s big or bothersome.
“The presence of ovarian cysts after menopause necessitates a careful evaluation to rule out malignancy and to manage symptoms effectively.”
Medical Expert, Gynecologist
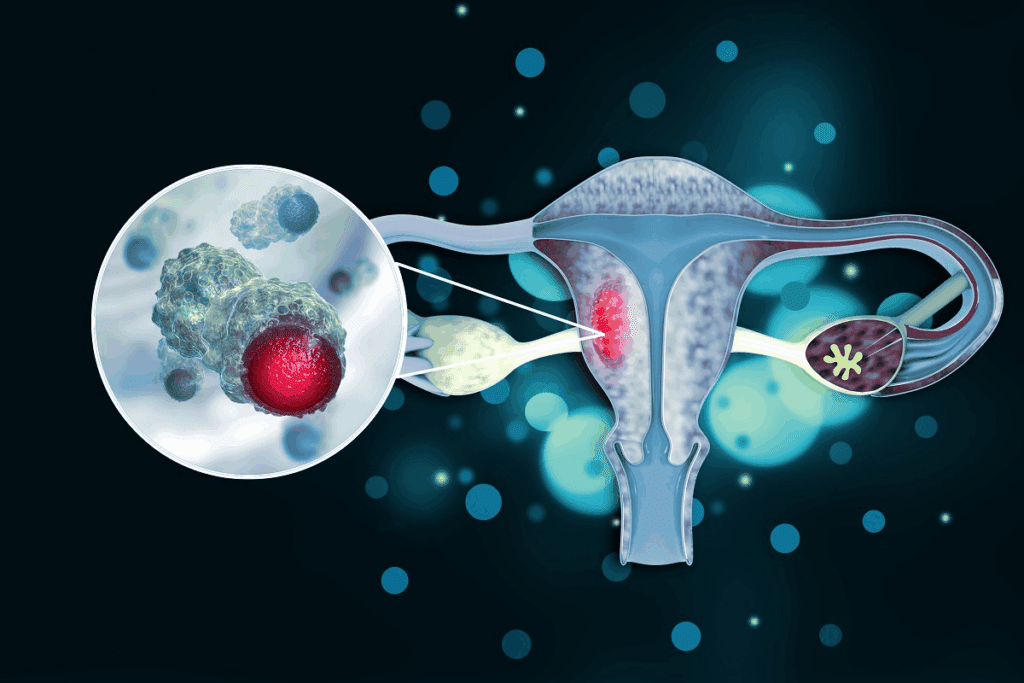
Ovarian Cancer: Risk Factors and Warning Signs
Ovarian cancer is a big worry for older women. The risk goes up with age. Family history, genetic mutations, and breast cancer history are key risk factors.
- Early satiety or difficulty eating
- Bloating or increased abdominal girth
- Pelvic or abdominal pain
- Urgency or frequency of urination
Spotting these symptoms early is key. We urge women to watch their health closely. If symptoms don’t go away, see a doctor.
Risk Factor | Description |
Family History | Having first-degree relatives (mother, sister, daughter) diagnosed with ovarian or breast cancer |
Genetic Mutations | Presence of BRCA1 or BRCA2 gene mutations |
Personal History | Previous diagnosis of breast cancer, specially at a young age |
Pelvic Inflammatory Disease in Older Women
Pelvic inflammatory disease (PID) is less common after menopause. It’s caused by bacterial infections. Symptoms include pelvic pain, unusual vaginal discharge, and fever.
Quick treatment with antibiotics is vital. It helps avoid infertility and chronic pain. Doctors use tests and exams to diagnose PID.
In summary, ovarian pain after menopause can have many causes. Each has its own risks and symptoms. A thorough medical check is essential to find the cause and the right treatment.
Less Common Gynecological Causes of Postmenopausal Ovarian Pain
There are many less common gynecological conditions that can cause ovarian pain after menopause. These conditions are important to diagnose and treat. They help manage postmenopausal ovarian pain.
Ovarian Torsion: Rare but Serious
Ovarian torsion is a rare but serious issue. It happens when the ovary twists, cutting off blood supply. It’s more common in younger women but can also affect postmenopausal women, often with cysts or masses.
Symptoms include severe pain, nausea, and vomiting. Quick medical help is needed to save the ovary and avoid serious problems.
Endometriosis Related to Hormone Replacement Therapy
Endometriosis can start or worsen after menopause, often in women on hormone therapy. Hormone therapy can make endometrial tissue grow, causing pain.
Women on hormone therapy should watch for signs like pelvic pain and heavy bleeding. Adjusting the therapy or other treatments might help manage symptoms.
Uterine Fibroids Persisting After Menopause
Uterine fibroids can keep growing after menopause and cause pain. They usually shrink but some grow, even with hormone therapy.
Symptoms include pelvic pressure and pain during sex. Treatment options vary from watching them to surgery, based on size and symptoms.
Ovarian remnant syndrome is another rare condition that can cause pain in postmenopausal women. It shows how complex diagnosing ovarian pain can be.
Condition | Symptoms | Treatment Options |
Ovarian Torsion | Severe pelvic pain, nausea, vomiting | Surgical intervention |
Endometriosis | Pelvic pain, heavy bleeding | Adjust HRT, pain management |
Uterine Fibroids | Pelvic pressure, heavy bleeding, pain during intercourse | Monitoring, surgical intervention |
Vascular and Connective Tissue Disorders
Vascular and connective tissue disorders are often overlooked causes of ovarian pain in postmenopausal women. As we age, the decline in estrogen levels can lead to various changes in the vascular and connective tissues. These changes can potentially cause discomfort or pain.
Pelvic Congestion Syndrome in Postmenopausal Women
Pelvic congestion syndrome (PCS) is a condition characterized by chronic pelvic pain associated with varicose veins in the lower pelvis. While more common in premenopausal women, PCS can persist or develop after menopause due to hormonal changes and vascular alterations.
Symptoms and Diagnosis: Women with PCS often experience a dull, aching pain in the pelvic area. This pain may worsen throughout the day, specially after standing for long periods. Diagnosis typically involves imaging studies like ultrasound or MRI to visualize the varicose veins.
Pelvic Floor Dysfunction and Chronic Pain
Pelvic floor dysfunction refers to the inability to coordinate the muscles in the pelvic floor. This leads to symptoms like chronic pain, constipation, or urinary incontinence. After menopause, the decrease in estrogen can cause the pelvic floor muscles to weaken, contributing to dysfunction.
The pelvic floor is a complex structure of muscles that support the uterus, bladder, and bowel. As estrogen levels decline, these muscles may weaken or spasm. Nerves become hypersensitive, and organs may shift slightly, causing discomfort or pressure.
Condition | Symptoms | Common Treatments |
Pelvic Congestion Syndrome | Chronic pelvic pain, varicose veins | Embolization, pain management |
Pelvic Floor Dysfunction | Chronic pain, incontinence, constipation | Physical therapy, biofeedback, medication |
Understanding these vascular and connective tissue disorders is key to managing ovarian pain after menopause. By recognizing the symptoms and seeking appropriate medical care, women can find relief from these conditions.
Non-Gynecological Conditions Mimicking Ovary Pain
Postmenopausal ovarian pain can be tricky to figure out. Many non-gynecological conditions can look like ovarian pain. It’s important for women and doctors to look at many possible causes of pelvic or abdominal pain.
Gastrointestinal Causes: IBS and Diverticulitis
Gastrointestinal problems are common in postmenopausal women. They can be mistaken for ovarian pain. Irritable Bowel Syndrome (IBS) causes stomach pain, bloating, and changes in bowel movements. Menopause can make these symptoms worse.
Diverticulitis is another issue. It’s inflammation of the colon’s diverticula. Symptoms include lower abdominal pain, fever, and changes in bowel habits. These can be mistaken for ovarian pain.
Condition | Common Symptoms | Distinguishing Features |
IBS | Abdominal pain, bloating, changes in bowel movements | Chronic condition, symptoms vary over time |
Diverticulitis | Lower abdominal pain, fever, changes in bowel habits | Acute onset, often accompanied by fever and elevated white blood cell count |
Urinary System Issues and Pelvic Hernias
Urinary system problems can also cause pain that looks like ovarian pain. Urinary Tract Infections (UTIs) and interstitial cystitis can cause pelvic pain. Pelvic hernias, like obturator or femoral hernias, can also cause pain in the groin or pelvic area.
“Accurate diagnosis requires a thorough evaluation, considering both gynecological and non-gynecological causes of pelvic pain.”
— Expert Opinion
We must think about these non-gynecological conditions when looking at postmenopausal ovarian pain. A detailed medical history, physical exam, and tests are key to finding the real cause of pain.
Understanding the many possible causes of postmenopausal ovarian pain helps women and doctors find the right treatment. This way, they can work together to solve the problem.
Diagnosing the Source of Ovarian Pain After Menopause
Ovarian pain after menopause can have many causes. To find the source, we use a detailed approach. This includes looking at medical history, doing physical exams, and using imaging and lab tests.
Comprehensive Medical History and Physical Examination
We start by asking about your past health. This helps us understand if past conditions or treatments might be linked to your pain. A thorough check-up is also key, including both outside and inside pelvic exams.
Getting a comprehensive medical history is very important. We ask about when the pain started, how long it lasts, and what it feels like. We also want to know if you have any other symptoms.
Imaging Studies: Ultrasound, CT Scan, and MRI
Imaging tests are critical in finding the cause of ovarian pain. Ultrasound is often the first choice. It helps us see the ovaries and look for cysts or masses. Sometimes, a CT scan or MRI is needed for more detailed views of the pelvic area.
Imaging Modality | Primary Use | Benefits |
Ultrasound | Initial assessment of ovarian morphology | Non-invasive, widely available |
CT Scan | Detailed evaluation of pelvic structures | High-resolution images, useful for complex cases |
MRI | Further characterization of ovarian and pelvic abnormalities | Excellent soft tissue differentiation, no radiation |
Laboratory Tests and Cancer Markers
Blood tests are a big part of diagnosing. They help us check for infections, inflammation, or other issues that might be causing pain. Sometimes, we test for cancer markers like CA-125 if we suspect ovarian cancer.
It’s important to remember that CA-125 isn’t a sure sign of ovarian cancer. But it can give us clues when we look at it with other findings and images.
By using medical history, physical exams, imaging, and lab tests together, we can find the cause of ovarian pain after menopause. Then, we can plan the right treatment.
Treatment Approaches for Postmenopausal Ovarian Pain
There are many ways to treat ovarian pain after menopause. These include medicines and changes in lifestyle. Finding the right treatment starts with knowing what’s causing the pain.
Medication Options for Different Causes
Medicine is key in treating postmenopausal ovarian pain. The choice of medicine depends on the pain’s cause. For example, hormone replacement therapy (HRT) helps with severe menopausal symptoms, including pain.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are good for pain from cysts or inflammation. For pelvic congestion syndrome, medroxyprogesterone acetate might be used to cut down on pain by reducing blood flow.
Surgical Interventions: When They’re Necessary
Surgery is needed for serious issues like ovarian torsion or big cysts at risk of bursting. Laparoscopic surgery is a less invasive way to treat these problems. It leads to faster recovery than open surgery.
If ovarian cancer is suspected or found, more surgery is needed. This might include removing the ovaries and other affected areas.
Complementary and Alternative Management Strategies
Complementary therapies can help with postmenopausal ovarian pain. Pelvic floor physical therapy is good for pain from pelvic floor issues. Acupuncture and other alternative methods can also help by reducing pain and boosting well-being.
Making lifestyle changes is also important. This includes eating right, exercising regularly, and managing stress with yoga or meditation. These actions can help manage pain and improve life quality.
When to Seek Immediate Medical Attention
Knowing when to act on ovarian pain after menopause can save lives. Menopause-related pelvic pain is usually not serious. But, there are times when you must see a doctor.
Red Flag Symptoms That Shouldn’t Be Ignored
Some symptoms with ovarian pain after menopause need quick action. These include severe or getting worse pain, bleeding after 12 months without a period, or pain with fever or stomach issues.
- Severe or Sudden Pain: Sudden, severe pain might mean a serious issue like ovarian torsion.
- Vaginal Bleeding: Bleeding after menopause, heavy or painful, needs quick check-up.
- Fever and Chills: These could mean an infection, like pelvic inflammatory disease.
- Gastrointestinal Symptoms: Nausea, vomiting, or bowel changes with pain might point to a bigger problem.
Differentiating Emergency Situations from Routine Concerns
Telling emergency situations from everyday worries can be hard. Knowing your symptoms and health history well is key.
Symptom | Possible Cause | Action |
Severe abdominal pain | Ovarian torsion, rupture | Seek immediate medical attention |
Vaginal bleeding after menopause | Endometrial cancer, hormonal changes | Schedule an urgent doctor’s visit |
Fever with pelvic pain | Pelvic inflammatory disease | Seek immediate medical care |
Knowing these warning signs and when to get help can greatly improve your health. If you’re not sure about your symptoms, always talk to your doctor.
Conclusion: Managing Your Health Beyond Menopause
Ovarian pain after menopause is a symptom that needs attention. Many women face similar issues even years after their last period. This shows how important it is to manage health beyond menopause.
We’ve looked at various causes, from common gynecological issues to less common ones. It’s clear that a detailed diagnosis is needed to find the root cause of ovarian pain.
Managing ovarian pain requires a mix of hormone therapy, physical therapy, and lifestyle changes. Knowing the causes and treatments helps women take action. Working with healthcare providers is key to creating a personalized plan for post-menopause health.
By focusing on health and seeking medical help when needed, women can face menopause and beyond with confidence. Effective health management during this time is vital for overall well-being and tackling symptoms like ovarian pain.
FAQ
What are the common causes of ovary pain after menopause?
Ovary pain after menopause can come from many sources. This includes ovarian cysts and cancer. It can also be caused by pelvic inflammatory disease, ovarian torsion, and endometriosis linked to hormone therapy. Uterine fibroids and vascular disorders like pelvic congestion syndrome can also play a role.
How common is ovarian pain after menopause?
Ovarian pain after menopause is more common than many women think. It’s not as common as during reproductive years. But, it’s a big concern for many postmenopausal women.
What are the symptoms of ovarian torsion, and is it a serious condition?
Ovarian torsion is a rare but serious issue. It causes severe, sharp pain in the ovary. Symptoms also include nausea and vomiting. It needs immediate medical care to avoid damage.
Can gastrointestinal issues cause ovarian pain after menopause?
Yes, issues like irritable bowel syndrome (IBS) and diverticulitis can cause pain. This pain might seem like it’s coming from the ovaries. It’s important to figure out the real cause for proper treatment.
How is the cause of ovarian pain after menopause diagnosed?
To find the cause of ovarian pain, doctors take a detailed medical history and do a physical exam. They use imaging like ultrasound and CT scans. They also do lab tests, including cancer markers.
What treatment options are available for postmenopausal ovarian pain?
Treatment for postmenopausal ovarian pain varies based on the cause. It might include specific medications, surgery when needed, and other management strategies.
When should I seek immediate medical attention for ovarian pain after menopause?
Seek immediate medical help for severe, sudden, or sharp pain. Also, if you have heavy vaginal bleeding, fever, or signs of shock.
Can hormone replacement therapy (HRT) cause or alleviate ovarian pain after menopause?
HRT can sometimes lead to ovarian pain, like endometriosis. But, it’s not used to treat pain directly.
Are there any lifestyle changes that can help manage ovarian pain after menopause?
Yes, healthy lifestyle changes can help. These include keeping a healthy weight, exercising regularly, and managing stress. These can reduce pain and improve overall health.
Can ovarian pain after menopause be a sign of ovarian cancer?
Ovarian pain can be a symptom of ovarian cancer. Knowing the risk factors and warning signs is key for early detection and treatment.
How can pelvic floor dysfunction contribute to ovarian pain after menopause?
Pelvic floor dysfunction can cause chronic pain, including in the ovaries. It’s due to muscle tension and other factors. Treatment often involves physical therapy and other strategies.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10796202/
































