Understanding heterogeneous endometrium is key for women getting pelvic ultrasounds. It can mean there might be problems that need to be checked out homogeneous endometrium.
A heterogeneous endometrium means the uterine lining looks different on ultrasound. It shows uneven brightness and texture. Research shows a thicker lining can increase cancer risks, mainly in older women.
At Liv Hospital, our skilled ultrasound team uses the latest tech to check the uterine lining. We offer full support and expert advice. This helps women understand their health and what treatment options are available.
Key Takeaways
- A heterogeneous endometrium is an abnormal ultrasound finding that requires careful evaluation.
- A thicker uterine lining may increase the risk of endometrial and uterine cancers.
- Expert assessment by experienced ultrasound specialists is essential for accurate diagnosis.
- Comprehensive support is available for women undergoing diagnosis and treatment.
- Advanced imaging technology helps identify possible issues with the uterine lining.
The Anatomy and Function of the Endometrium
The endometrium is a thin layer of tissue in the uterus. It’s key for supporting pregnancy and changes a lot during the menstrual cycle. This tissue is vital for fertility and uterine health.
Structure and Layers of the Uterine Lining
The endometrium has two layers: the basal layer and the functional layer. The basal layer is deeper and more permanent. It helps the functional layer grow back. The functional layer changes a lot during the menstrual cycle, getting thicker for pregnancy and shedding if not.
This structure is key for the endometrium’s role. It allows for renewal and preparation for each cycle. A endometrial homogeneous look is usually a sign of health. But, changes can happen for many reasons.
Physiological Changes Throughout the Menstrual Cycle
The endometrium changes a lot during the menstrual cycle, mainly due to hormones. In the proliferative phase, it gets thicker with estrogen. After ovulation, the secretory phase starts, making it even thicker and ready for an embryo.
If there’s no pregnancy, the endometrium sheds during menstruation. This starts a new cycle. This cycle is key for reproductive health. Knowing these changes helps in checking endometrial health and spotting issues, like an endometrium echogenic pattern.
In short, the endometrium’s structure and function are linked to reproduction. Its ability to change and renew is essential for fertility. Knowing what’s normal, like being endometrial homogeneous, and spotting changes helps in managing reproductive health.
Heterogeneous Endometrium: Definition and Characteristics
Understanding ‘heterogeneous endometrium’ is key to reading ultrasound results right. We’ll dive into what this term means in ultrasound talk and its impact on uterine health.
What “Heterogeneous” Means in Ultrasound Terminology
In ultrasound, “heterogeneous” means a mix of different patterns in the endometrium. This shows the uterine lining is not even, with different brightness and texture. A heterogeneous endometrium has these uneven patterns.
Studies show uneven endometrial patterns are linked to health issues. So, seeing a heterogeneous endometrium on ultrasound means you need to look closer.
Visual Markers of Endometrial Heterogeneity
Ultrasound can spot signs of endometrial heterogeneity. These include:
- Irregular thickening or thinning of the endometrium
- Presence of cysts or polyps within the endometrial layer
- Variations in echogenicity, appearing as areas of different brightness
- Heterogeneous texture, which may include areas of increased or decreased echogenicity
To grasp these signs, let’s look at a table:
Visual Marker | Description | Potential Implication |
Irregular Thickening | Uneven thickness of the endometrium | Possible hyperplasia or polyp |
Cysts or Polyps | Presence of fluid-filled structures or growths | Benign growths or potentially malignant lesions |
Variations in Echogenicity | Areas of different brightness within the endometrium | May indicate hormonal influences or pathology |
Seeing a heterogeneous endometrium means more tests are needed. These might include more images or taking a sample from the endometrium.
Knowing about heterogeneous endometrium helps doctors check uterine health. They can then decide on more tests or treatments.
Understanding Homogeneous Endometrium and Normal Patterns
A homogeneous endometrium looks the same all over, which is a sign of a healthy uterine lining. This uniform look is seen during specific times in the menstrual cycle. It changes with hormone levels.
Characteristics of a Healthy Homogeneous Endometrium
A healthy homogeneous endometrium looks the same and bright on ultrasound. This shows it’s even in thickness and texture. This is important for many reproductive tasks.
The brightness of the endometrium changes with hormones. In the early part of the cycle, it gets thicker and brighter. This is when it’s ready for an embryo to implant.
Expected Endometrial Appearance by Age and Hormonal Status
The thickness and look of the endometrium change with age and hormones. In younger women, it changes with estrogen and progesterone levels.
In older women, the endometrium is thinner and more even. This is because estrogen levels drop. Any big changes might need more checking.
Age Group | Expected Endometrial Appearance |
Premenopausal | Cyclic changes, varying thickness |
Postmenopausal | Thin, homogeneous |
Reproductive Age | Thickening during proliferative phase |
Is Homogeneous Endometrium Always Good?
Even though a homogeneous endometrium usually means a healthy lining, it’s not always a sure sign. Hormonal issues or thinning can also make it look even.
So, it’s key to look at the whole picture. Symptoms and other tests help understand what a homogeneous endometrium really means.
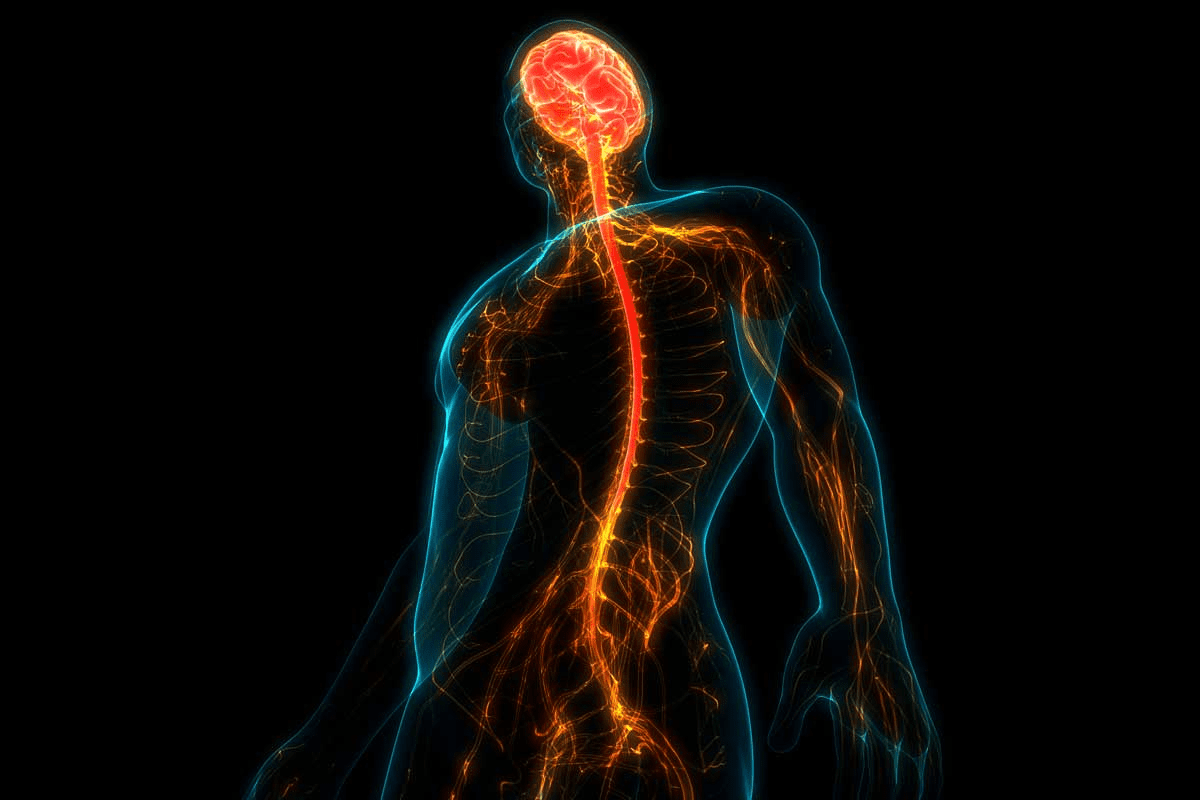
Endometrial Echogenicity: What It Reveals About Uterine Health
Ultrasound shows us the endometrium’s health. Its look changes with hormones, age, and diseases. Knowing these changes helps us spot and treat uterine problems.
Hyperechogenic vs. Hypoechogenic Patterns
Hyperechogenic and hypoechogenic describe the endometrium’s look on ultrasound. A hyperechogenic endometrium is brighter, and a hypoechogenic endometrium is darker. These looks mean different things:
- A hyperechogenic endometrium might show polyps, hyperplasia, or secretory changes.
- A hypoechogenic endometrium could mean the proliferative phase or atrophy.
Spotting these patterns helps us find endometrial problems.
Interpreting Different Echogenic Patterns in the Endometrium
Understanding the endometrium’s echogenicity needs knowing the patient’s situation. For example:
- The endometrium’s look changes with the menstrual cycle, getting more hypoechogenic in the proliferative phase and hyperechogenic in the secretory phase.
- In postmenopausal women, a thick or mixed endometrium might need more tests because of cancer risk.
These signs tell us a lot about the uterus and guide us to more tests.
The Significance of Echogenic Endometrium in Different Life Stages
The importance of endometrial echogenicity changes with age:
Life Stage | Echogenicity Significance |
Reproductive Age | Changes in echogenicity help assess menstrual cycle phase and fertility. |
Postmenopause | A thick or mixed endometrium might mean disease, needing a biopsy. |
Pregnancy | Echogenicity patterns can tell us about implantation and early pregnancy health. |
Knowing these age-related differences is key for correct diagnosis and care.
Common Causes of Heterogeneous Endometrium
Many factors can lead to a heterogeneous endometrium. This includes both harmless and serious conditions. The endometrium, a dynamic layer of the uterus, changes with hormones. Knowing what causes these changes is key for diagnosis and treatment.
Benign Conditions Leading to Endometrial Heterogeneity
Some harmless conditions can make the endometrium look different on ultrasound. These include:
- Endometrial polyps: Growths in the endometrial lining that can cause irregularities in the uterine cavity.
- Endometrial hyperplasia: A condition where endometrial cells grow too much, often due to hormonal imbalance.
- Adenomyosis: A condition where tissue like the endometrium grows into the uterine wall, leading to heterogeneity.
More Serious Underlying Conditions
In some cases, a heterogeneous endometrium may be a sign of serious conditions. These can include:
- Endometrial cancer: A cancer of the endometrium that can show up as heterogeneity on imaging studies.
- Other malignancies: Rarely, other cancers can spread to the endometrium, causing heterogeneity.
Healthcare providers must carefully check for the cause of a heterogeneous endometrium. They use clinical checks, imaging, and sometimes biopsies. This helps find the right treatment for the condition.
Diagnostic Approaches for Heterogeneous Endometrium
To diagnose heterogeneous endometrium, we use a detailed strategy. We apply different methods to accurately check and handle endometrial heterogeneity.
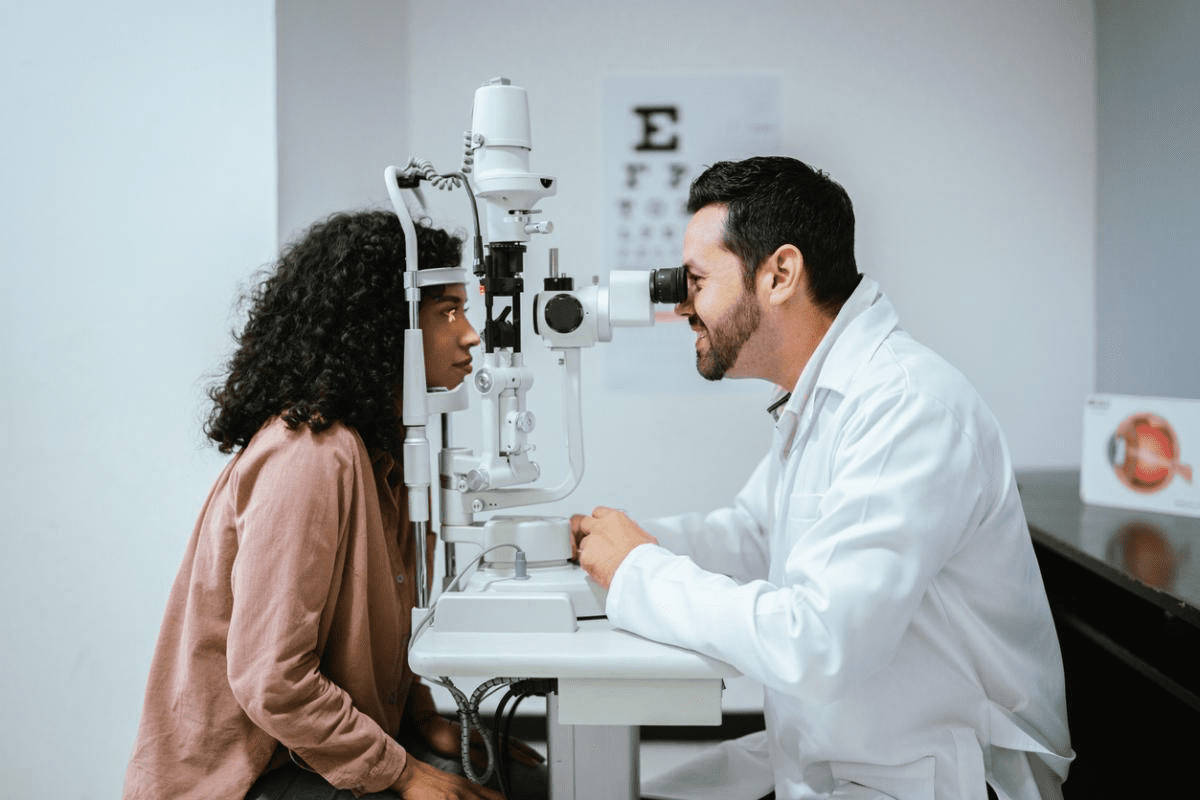
Transvaginal Ultrasound Evaluation
Transvaginal ultrasound is key for checking the endometrium. It gives clear images of the uterine lining. We can see its thickness, texture, and any issues. Key features assessed during transvaginal ultrasound include:
- Endometrial thickness and echogenicity
- Presence of focal lesions or irregularities
- Uniformity or heterogeneity of the endometrial texture
Saline Infusion Sonography (SIS)
Saline Infusion Sonography (SIS) is a special ultrasound method. It uses saline solution to see the endometrial cavity better. This helps find small problems like polyps or adhesions that cause heterogeneity.
Benefits of SIS include:
- Improved detection of intrauterine lesions
- Enhanced visualization of the endometrial surface
- More accurate diagnosis of structural abnormalities
Endometrial Sampling and Biopsy Procedures
Sometimes, we need to take tissue samples from the uterine lining. This is for a clear diagnosis. These samples are then checked under a microscope.
The decision to perform a biopsy is typically based on:
- Ultrasound findings suggestive of malignancy or other serious conditions
- Presence of abnormal uterine bleeding
- Risk factors for endometrial cancer or other pathologies
Advanced Imaging: MRI and Hysteroscopy
In complex cases, we use MRI or hysteroscopy. MRI shows detailed images of the uterus and nearby areas. Hysteroscopy lets us see the inside of the uterus directly.
These advanced methods offer:
- Detailed assessment of the extent of disease
- Preoperative planning for surgical interventions
- Confirmation of diagnosis in challenging cases
Is Heterogeneous Endometrium Normal? Age-Related Considerations
The question of whether a heterogeneous endometrium is normal changes with age. As we get older, our endometrium changes due to hormones and other health factors.
Premenopausal Women: When to Be Concerned
In younger women, a mixed endometrium might be okay, depending on the menstrual cycle. But, other signs and health history matter too.
Women with heavy or irregular periods might need more tests. This could check for endometrial polyps or fibroids.
Postmenopausal Women: Risk Assessment
Older women with mixed endometrium face a higher risk of cancer. It’s key to check for symptoms like bleeding after menopause.
Risk Factors | Low Risk | High Risk |
Age | > 60 years | |
Endometrial Thickness | > 5 mm | |
Postmenopausal Bleeding | No | Yes |
Heterogeneous Endometrium During Pregnancy
Pregnancy changes the endometrium to support the baby. A mixed endometrium is usually not a worry unless it’s with other symptoms.
In summary, whether a mixed endometrium is normal depends on age, reproductive status, and symptoms. A doctor’s check-up is needed to find out why and how to handle it.
Implications for Fertility and Reproductive Health
Women trying to get pregnant need to know about heterogeneous endometrium. It’s when the uterine lining looks uneven. This can be seen on an ultrasound. It can change how well a woman can get pregnant.
How Endometrial Heterogeneity May Affect Conception
Having a heterogeneous endometrium can make it harder to get pregnant. It changes the uterine lining, making it less ready for an embryo. Research shows this can lower fertility because of how it affects the lining’s readiness.
“The endometrium is key for implantation,” says Medical Expert, a fertility expert. “Any problem with it can make it tough to conceive.” This shows why checking the endometrium is important for women having trouble getting pregnant.
Impact on Implantation and Pregnancy Outcomes
A heterogeneous endometrium can also affect how well a pregnancy sticks. Studies show women with heterogeneous echogenicity in the uterus might face more miscarriages and pregnancy problems.
- Increased risk of implantation failure
- Higher risk of miscarriage
- Potential complications during pregnancy
Knowing these risks helps women plan and make choices about fertility treatments.
Management Options for Women Trying to Conceive
Women with heterogeneous endometrium have several options. These include hormone treatments, surgery to fix issues, and IVF. Each option aims to help with getting pregnant.
It’s best for women to talk to a fertility specialist. They can help figure out the best plan for each woman. “Tailored care is key for dealing with fertility issues from heterogeneous endometrium,” says Medical Expert, a reproductive endocrinologist.
By learning about heterogeneous endometrium and the options available, women can make better choices. This can help them have a successful pregnancy.
Treatment Options for Conditions Causing Heterogeneous Endometrium
When a heterogeneous endometrium is found, the treatment depends on the cause. We look at the patient’s age, symptoms, and goals to find the best plan.
Management Strategies
Hormonal therapies help with endometriosis or hormonal issues that cause endometrial heterogeneity. Sometimes, surgery like polypectomy or hysteroscopy is needed to remove growths or fix the uterus.
Surgical Interventions and Monitoring
For severe cases or when other treatments fail, surgeries like hysterectomy might be needed. Regular ultrasounds and check-ups help see if the treatment works and make changes if needed.
For women with a hyperechoic uterine lining, we focus on the cause and the patient’s health. We tailor treatments to meet individual needs. This helps ease symptoms, improve life quality, and support reproductive goals.
FAQ
What does heterogeneous endometrium mean?
Heterogeneous endometrium means the uterine lining looks uneven. This can happen during ultrasound checks. It might be due to hormonal changes, growths, or serious diseases.
Is heterogeneous endometrium normal?
It depends on your age, if you’re pregnant, and your health. Sometimes, it’s okay, like during certain times in your cycle or pregnancy. But for postmenopausal women, it might mean health issues.
What causes heterogeneous endometrium?
It can be due to things like polyps or fibroids. Or it could be serious, like cancer. Hormonal changes and certain health issues also play a part.
How is heterogeneous endometrium diagnosed?
Doctors use ultrasound, saline infusion sonography, and sometimes MRI or hysteroscopy. They might also take a sample to check the lining.
Can heterogeneous endometrium affect fertility?
Yes, it can. It might make it hard to get pregnant or carry a pregnancy. Finding and treating the cause can help with fertility.
What are the treatment options for conditions causing heterogeneous endometrium?
Treatment varies based on the cause. It might include hormones, surgery, or just watching it. The best plan is based on your health and condition.
Is a homogeneous endometrium always a sign of good health?
A homogeneous endometrium is usually good. But, it’s not the only sign of health. Your overall health and symptoms matter too.
How does endometrial echogenicity relate to uterine health?
The brightness of the uterine lining on ultrasound tells us about health. Different brightness levels can mean different things. It depends on your age and health.
What does hyperechogenic endometrium mean?
Hyperechogenic endometrium means the lining is too bright on ultrasound. It can mean hormonal changes or certain diseases.
Can heterogeneous endometrium be a sign of cancer?
Sometimes, it might mean a higher cancer risk, mainly in older women. But, most cases are not cancer. A proper diagnosis is needed.
References
National Center for Biotechnology Information. Heterogeneous Endometrium: Ultrasound Appearance and Clinical Significance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30916912/