Polycystic ovary syndrome (PCOS) is a common hormonal disorder affecting millions of women worldwide. Women with PCOS often face irregular menstrual cycles, heavy or prolonged periods, and painful menstruation. At Liv Hospital, we understand how these symptoms affect daily life. We are committed to providing compassionate care. Does PCOS cause heavy bleeding? This ultimate guide reveals the alarming, critical truth and the best, powerful strategies for relief.
Understanding the link between PCOS and menstrual irregularities is key to effective management. We will dive into the hormonal mechanisms behind PCOS and its effects on menstrual cycles. This will give insights into the experiences of women with this condition.
Key Takeaways
- PCOS is a hormonal disorder that affects menstrual cycles.
- Heavy or prolonged periods are common symptoms of PCOS.
- Painful menstruation is a significant issue for many women with PCOS.
- Understanding PCOS symptoms is vital for effective management.
- Liv Hospital provides patient-centered care for women with PCOS.
Understanding PCOS: A Common Hormonal Disorder

PCOS, or Polycystic Ovary Syndrome, is a hormonal disorder that affects women of childbearing age. It causes a range of symptoms due to hormonal imbalances.
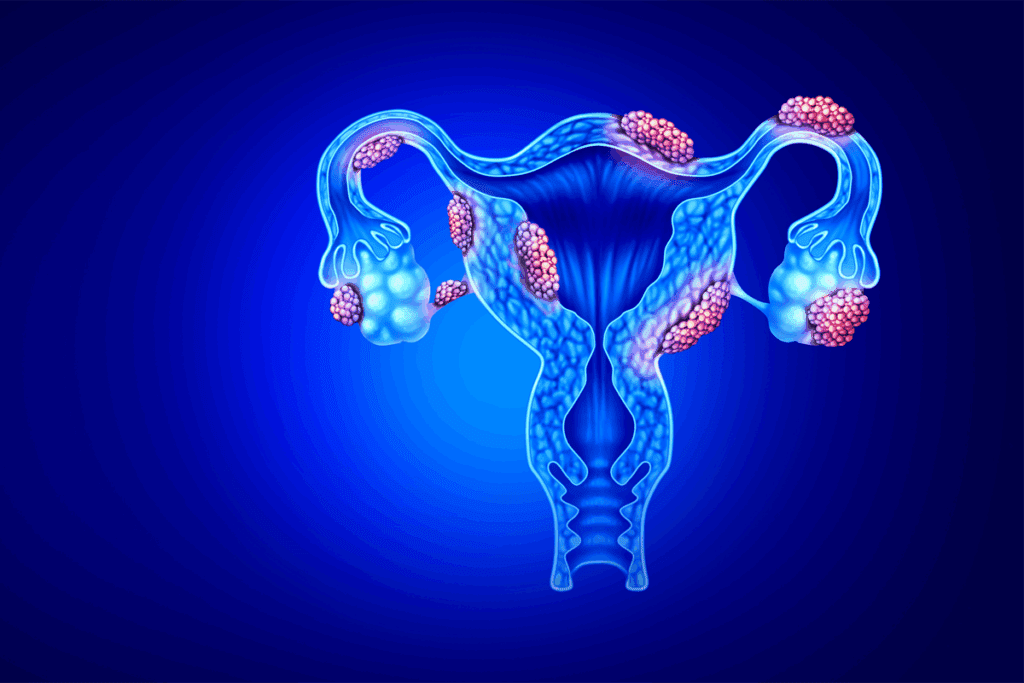
What Is Polycystic Ovary Syndrome?
PCOS is a complex endocrine disorder that affects the ovaries. It leads to irregular menstrual cycles, cysts on the ovaries, and other metabolic issues. It is marked by hyperandrogenism, ovulatory dysfunction, and polycystic ovaries seen on ultrasound.
Prevalence and Risk Factors
PCOS is influenced by genetics and environment. It affects 6% to 12% of women of reproductive age in the U.S. Insulin resistance is a key factor in its development and severity.
Risk Factors | Description |
Genetic Predisposition | Family history of PCOS or related conditions |
Insulin Resistance | Body’s cells do not respond effectively to insulin |
Hormonal Imbalance | Disturbances in levels of estrogen, progesterone, and testosterone |
The Hormonal Imbalance Behind PCOS
The hormonal imbalance in PCOS affects estrogen, progesterone, and testosterone levels. Heavy menstrual bleeding affects 10-30 percent of women with PCOS. Understanding these imbalances is key to managing symptoms and improving quality of life.
PCOS is a complex condition needing a holistic approach. By grasping its prevalence, risk factors, and hormonal imbalances, we can improve diagnosis and treatment.
The Relationship Between PCOS and Menstrual Irregularities
Women with Polycystic Ovary Syndrome (PCOS) often face menstrual problems. These issues can affect their daily life a lot. They might have periods that are too far apart, too long, or too heavy. These problems are linked to the hormonal imbalances found in PCOS.
Common Menstrual Patterns in PCOS
Menstrual issues are common in PCOS, affecting up to 80% of women. The most common issue is oligomenorrhea, where cycles last more than 35 days. Other problems include not getting periods at all and having very heavy or long periods.
The hormonal imbalance in PCOS, with low progesterone and high estrogen, causes these issues. This imbalance messes up the normal cycle. It can affect fertility and overall health a lot.
Oligomenorrhea: When Cycles Extend Beyond 35 Days
Oligomenorrhea is a big problem in PCOS, where periods come less often. Women might have cycles that last up to 45 days or more. This often means they don’t ovulate, or release an egg.
About 80% of women with PCOS have oligomenorrhea. It’s caused by hormonal imbalances and insulin resistance, common in PCOS.
Why Menstrual Cycles Become Disrupted in PCOS
Menstrual cycle problems in PCOS come from hormonal imbalances. Low progesterone and high estrogen mess up the cycle’s feedback loop. Insulin resistance and high male hormones also play a part.
It’s important to know why menstrual issues happen in PCOS. This helps doctors find the right treatments. By fixing hormonal imbalances and other issues, doctors can help women with PCOS feel better and live better lives.
Does PCOS Cause Heavy Bleeding? The Scientific Evidence
PCOS and heavy bleeding are linked through hormonal and physical factors. Women with PCOS often face irregular periods, including heavy bleeding. This is a big concern for many.
Prevalence of Heavy Bleeding in PCOS Patients
Research shows women with PCOS are more likely to have heavy periods. This is due to hormonal imbalances and how they affect the uterus.
Key findings include:
- Women with PCOS are at a higher risk of experiencing heavy menstrual bleeding.
- Hormonal imbalances, like low progesterone and high estrogen, lead to heavy bleeding.
- The uterine lining gets thicker because of these hormonal changes, causing heavier periods.
How Hormonal Imbalances Lead to Excessive Bleeding
Hormonal imbalance in PCOS is key to heavy bleeding. The balance between estrogen and progesterone affects the uterus.
Estrogen makes the uterine lining grow, while progesterone keeps it stable. In PCOS, low progesterone and high estrogen make the lining thicker. This leads to heavier bleeding.
Measuring Normal vs. Heavy Menstrual Flow
Knowing the difference between normal and heavy flow is key. Normal flow lasts 3 to 7 days and loses about 30-40 mL of blood.
Characteristics | Normal Menstrual Flow | Heavy Menstrual Flow |
Duration | 3-7 days | More than 7 days |
Blood Loss | 30-40 mL | More than 80 mL |
Heavy flow is over 80 mL or lasts more than 7 days. Women with PCOS may need to change products often. They might pass large clots.
The Mechanism Behind PCOS and Heavy Periods
Women with Polycystic Ovary Syndrome (PCOS) often face heavy and long menstrual bleeding. This is due to complex hormonal interactions. It’s vital to grasp the underlying mechanisms to improve their quality of life.
Endometrial Thickening Due to Hormonal Fluctuations
In PCOS, hormonal balance is disrupted, causing endometrial thickening. The endometrium, the uterus lining, thickens each month in preparation for pregnancy. In PCOS, this thickening becomes excessive due to lack of ovulation and hormonal imbalance.
This excessive thickening leads to heavier and longer menstrual bleeding. Studies reveal women with PCOS may lose almost double the normal amount of blood. They often experience clotting during their periods.
The Role of Low Progesterone and High Estrogen
The hormonal imbalance in PCOS, with low progesterone and high estrogen levels, is key to endometrial thickening. Progesterone stabilizes the endometrium and prepares it for pregnancy. With low progesterone, the endometrium grows under estrogen’s influence, causing excessive thickening.
Why PCOS Periods May Last Longer Than 10 Days
Women with PCOS often experience prolonged menstrual bleeding. The irregular shedding of the endometrium, along with its excessive thickening, can make periods last longer than usual. They often extend beyond 10 days.
- Irregular hormonal feedback mechanisms
- Failure to ovulate regularly
- Continuous estrogen exposure without sufficient progesterone
These factors lead to irregular and prolonged menstrual bleeding in PCOS.
Understanding Clotting in PCOS-Related Heavy Bleeding
Clotting during heavy menstrual bleeding is a major concern for women with PCOS. The heavy flow can cause large clots and severe cramping. It’s important to understand the cause of clotting to manage heavy bleeding effectively.
In PCOS, hormonal imbalances and endometrial thickening cause both heavy flow and clots. Managing these underlying hormonal issues is key to effective management.
PCOS and Painful Periods: Understanding the Connection
The link between PCOS and painful periods is complex. It involves hormonal imbalances and uterine contractions that make menstrual pain worse. Women with PCOS often face irregular periods and dysmenorrhea, which means painful cramps during menstruation.
How PCOS Contributes to Menstrual Pain
PCOS leads to menstrual pain through several ways. A big factor is the hormonal imbalance, with too much estrogen and not enough progesterone. This imbalance makes the endometrium thicker, causing more painful cramps.
Heavy bleeding in PCOS forces the uterus to contract harder to get rid of excess lining. This increases pelvic pain, making menstrual pain worse for women with PCOS.
Uterine Contractions and Heavy Bleeding
Uterine contractions are key in menstrual pain, more so in women with PCOS. The uterus contracts to shed its lining during menstruation. In PCOS, these contractions are stronger because of hormonal imbalances and a thicker endometrial lining.
To grasp how uterine contractions affect menstrual pain in PCOS, let’s look at a table. It outlines the factors that make painful periods worse in PCOS:
Factor | Description | Impact on Pain |
Hormonal Imbalance | Elevated estrogen and low progesterone | Increases endometrial thickness, leading to more painful cramps |
Uterine Contractions | Forceful contractions to expel excess lining | More intense pain due to stronger contractions |
Endometrial Thickness | Thicker lining due to hormonal imbalance | More painful shedding of the lining |
Differentiating PCOS Pain from Other Gynecological Conditions
It’s important to tell PCOS-related menstrual pain from other gynecological conditions. Conditions like endometriosis, adenomyosis, and fibroids can also cause painful periods. A detailed evaluation is needed to find the real cause.
Knowing the specific signs of PCOS-related pain helps doctors make the right diagnosis. They can then create a treatment plan that works.
Additional Symptoms That May Accompany Heavy and Painful Periods
PCOS affects women in many ways. Heavy and painful periods are big concerns. But, women with PCOS face other challenges too.
Mood Swings and Emotional Symptoms
Mood swings and emotional symptoms are common in women with PCOS. Hormonal imbalances can cause anxiety, depression, and irritability. These feelings can be as tough as the physical symptoms, affecting daily life and relationships.
Managing these emotional symptoms is key. Counseling and stress management techniques help cope with PCOS’s emotional side.
- Mood swings can be triggered by hormonal changes.
- Emotional symptoms can impact daily life and relationships.
- Support systems, such as counseling, are vital for managing emotional symptoms.
PCOS and Anemia Risk
Women with PCOS are at higher risk of anemia due to heavy menstrual bleeding. Anemia causes fatigue, weakness, and shortness of breath. It adds to the health challenges women with PCOS face.
Women with PCOS should have regular check-ups. They should talk to their healthcare provider about their menstrual bleeding to lower anemia risk.
- Heavy menstrual bleeding can lead to anemia.
- Regular health check-ups are key for early detection.
- Dietary adjustments can help manage anemia risk.
Other Physical Discomforts
Women with PCOS may also face other physical discomforts. These include acne and hirsutism. These symptoms can hurt self-esteem and body image.
We know how important it is to tackle these symptoms fully. Treatments are available for acne, hirsutism, and other physical discomforts linked to PCOS.
Diagnosing PCOS When You Have Heavy or Painful Periods
Heavy or painful periods might mean you have PCOS. But, you need a full medical check to be sure. It’s important to see a doctor to find out why you’re feeling this way.
When to See a Doctor
If you have heavy or long periods, or a lot of pain, see a doctor. These signs could mean PCOS, but they might also point to other health issues. It’s key to get checked out.
A doctor will first ask about your health history. They’ll want to know about your periods, symptoms, and family health.
Tests and Examinations
To figure out if you have PCOS, you’ll need some tests. These might include:
- Hormonal Assessments: Blood tests to check hormone levels, including androgens and other hormones related to PCOS.
- Ultrasound: An ultrasound scan to examine the ovaries and check for cysts or other abnormalities.
- Physical Examination: A physical exam to look for signs of excess androgen, such as acne or excess hair growth.
These tests help doctors understand what’s causing your symptoms. They help make a correct diagnosis.
Diagnostic Test | Purpose |
Hormonal Assessments | To check for hormonal imbalances associated with PCOS |
Ultrasound | To examine the ovaries for cysts or other abnormalities |
Physical Examination | To look for signs of excess androgen |
Ruling Out Other Conditions
It’s important to check for other conditions that might cause similar symptoms. This includes thyroid problems, hyperprolactinemia, and other causes of irregular periods or heavy bleeding.
“Accurate diagnosis is key to managing PCOS effectively. A thorough evaluation helps in finding the best treatment plan.”
— Medical Expert, Endocrinologist
Knowing what’s causing your symptoms helps us create a treatment plan just for you. This way, we can help you feel better and improve your life.
Treatment Options for PCOS-Related Heavy Bleeding and Pain
Managing PCOS-related heavy bleeding and painful periods is key to improving life quality. Treatment involves hormonal and non-hormonal options.
Hormonal Treatments
Hormonal treatments are often the first choice for PCOS symptoms. They aim to balance hormones that cause menstrual issues.
Hormonal contraceptives are often used to control heavy bleeding and pain. They help regulate the menstrual cycle and reduce uterine lining thickness, cutting down on bleeding.
Anti-androgen medications treat symptoms like acne and excess hair, common in PCOS.
Non-Hormonal Medications for Pain and Bleeding
Some prefer or need non-hormonal meds alongside hormonal treatments. Nonsteroidal anti-inflammatory drugs (NSAIDs) help with pain and bleeding.
Iron supplements are suggested for those with anemia from heavy bleeding.
Surgical Interventions When Necessary
Surgery might be needed for some PCOS complications. Endometrial ablation destroys the uterine lining to stop heavy bleeding.
Lifestyle Modifications That Can Help
Lifestyle changes are vital for managing PCOS symptoms. Dietary modifications and regular exercise help regulate cycles and improve health.
Keeping a healthy weight is also important. Stress management techniques like yoga or meditation help manage symptoms.
Conclusion: Living Well with PCOS Despite Menstrual Challenges
Living with PCOS can be tough, mainly because of heavy and painful periods. But, with the right management, women can greatly improve their life quality. Understanding PCOS and its symptoms is key. This knowledge helps in creating a treatment plan that includes lifestyle changes and medical treatments.
PCOS can lead to irregular periods, heavy bleeding, and pain. It’s caused by hormonal imbalances. Managing these symptoms is vital for well-being. With the right diagnosis and treatment, women with PCOS can live active, healthy lives, reducing the effects of menstrual issues.
Managing PCOS requires a variety of approaches. This includes hormonal treatments, non-hormonal medications, and lifestyle adjustments. Working with healthcare providers helps in creating a plan tailored to individual needs. This proactive method lets women manage their condition, improving their health and life quality while dealing with PCOS.
FAQ
Does PCOS cause heavy bleeding?
Yes, PCOS can lead to heavy bleeding. This is due to hormonal imbalances, mainly between estrogen and progesterone. These imbalances cause the endometrium to thicken and shed irregularly.
Is PCOS associated with painful periods?
Yes, many women with PCOS experience painful periods. This pain is often caused by uterine contractions and hormonal changes.
Can PCOS cause anemia?
Yes, heavy menstrual bleeding from PCOS can increase anemia risk. This is because of significant blood loss over time.
How does PCOS affect menstrual cycles?
PCOS often disrupts menstrual cycles. This can lead to irregularities like oligomenorrhea, where cycles last over 35 days. This is due to hormonal imbalances.
Can ovarian cysts cause mood swings?
While cysts themselves might not directly cause mood swings, hormonal imbalances from PCOS can. These imbalances can lead to emotional symptoms, including mood swings.
What are the common symptoms of PCOS beside heavy and painful periods?
Women with PCOS may also experience acne, hirsutism, and emotional symptoms like mood swings. These symptoms, along with menstrual irregularities, are common.
How is PCOS diagnosed in women with heavy or painful periods?
Diagnosing PCOS requires a detailed medical evaluation. This includes a thorough history, physical exam, and diagnostic tests. These steps help rule out other conditions and confirm PCOS.
What treatment options are available for managing PCOS-related heavy bleeding and pain?
Treatment plans for PCOS may include hormonal treatments and non-hormonal medications for pain and bleeding. Lifestyle changes and, in some cases, surgery are also options to manage symptoms effectively.
Can lifestyle changes help manage PCOS symptoms?
Yes, a healthy lifestyle can help manage PCOS symptoms. This includes a balanced diet and regular exercise. These changes can reduce symptoms like heavy and painful periods.
Does PCOS make periods worse over time?
If not managed, PCOS symptoms, including heavy and painful periods, can worsen over time. This highlights the need for a proactive treatment plan.
References
National Center for Biotechnology Information. PCOS: Impact on Menstrual Bleeding and Period Pain. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6737062/


































