Last Updated on December 2, 2025 by Bilal Hasdemir
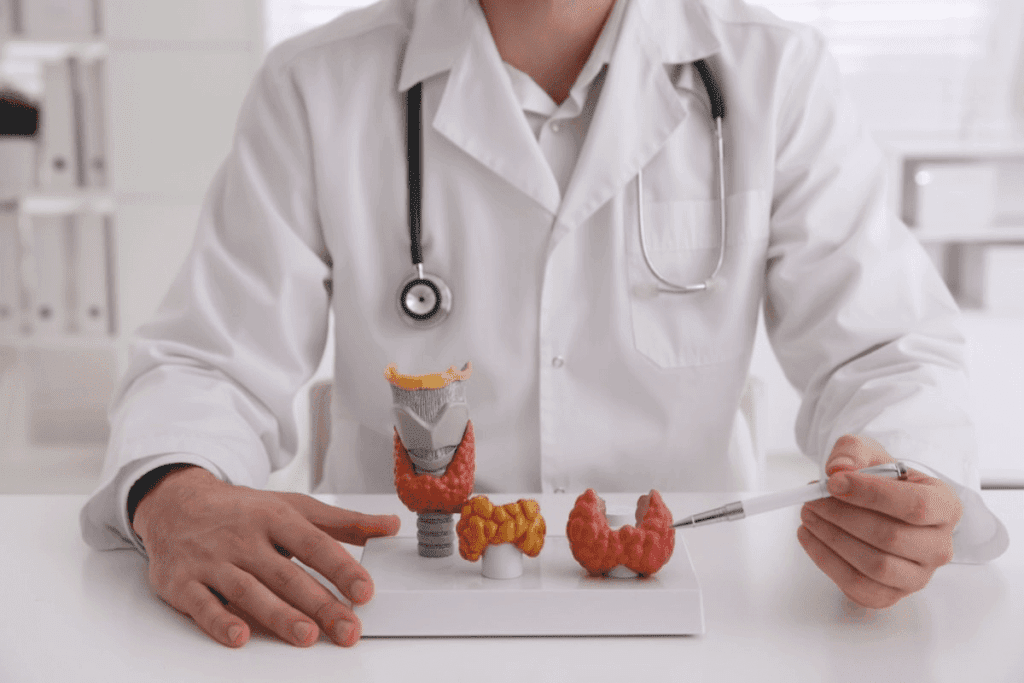
Nearly 1 in 10 adults in the United States has a thyroid disorder. Many need surgery to treat it. Identifying the specific conditions for which endocrine surgery is the primary or most effective treatment option. Learn about endocrine surgery cases.
Endocrine disorders like thyroid, parathyroid, adrenal, and pituitary disorders can really affect your life. If not treated right, they can cause big problems.
Surgery is a good option for many of these conditions. It can help patients feel better and live better lives.
Key Takeaways
- Thyroid disorders are common and often require surgical treatment.
- Parathyroid, adrenal, and pituitary disorders can also be treated surgically.
- Surgical intervention can significantly improve patient outcomes.
- Understanding the role of surgery in treating endocrine disorders is important.
- There are different surgical options for each disorder.
Understanding Endocrine Disorders and Their Treatment Options
It’s key to grasp the endocrine system’s complexity for the right treatment. This system has glands that make hormones. These hormones control growth, metabolism, and more.
The Endocrine System: Glands and Hormones
The system includes glands like the pituitary, thyroid, adrenal glands, pancreas, and gonads (ovaries and testes). Each gland makes hormones for health. For example, the thyroid controls metabolism, and the pancreas manages blood sugar.
Problems in the endocrine system can cause issues like hypothyroidism and diabetes. These problems come from gland issues or hormone imbalances.
Medical vs. Surgical Management of Endocrine Disorders
There are two main ways to treat endocrine disorders: medicine or surgery. Medicine might include hormone therapy or drugs to balance hormones. Surgery is needed for gland removal or when medicine doesn’t work.
“Surgical intervention is considered when there’s a need to remove a gland or tumor that’s causing the hormonal imbalance or when medical management is ineffective or not feasible.”
Surgery for endocrine issues might include removing the thyroid or pancreas. Doctors choose surgery based on tests and the patient’s health.
Disorder | Medical Management | Surgical Management |
Hypothyroidism | Hormone replacement therapy | Not typically required |
Thyroid Cancer | Radioactive iodine therapy | Thyroidectomy |
Primary Hyperparathyroidism | Monitoring, medication for symptoms | Parathyroidectomy |
Knowing the treatment options for endocrine disorders helps both doctors and patients. It leads to better decisions and a better life.
Overview of Endocrine Surgery: When Is It Necessary?
When other treatments don’t work, endocrine surgery is often needed. It involves procedures to fix problems with the endocrine glands. These glands make hormones that control our body’s functions.
Endocrine surgery is needed when a gland isn’t working right. This can include the thyroid, parathyroid, adrenal, or pancreas glands.
Indications for Surgical Intervention
Surgery is considered when gland problems can’t be fixed with medicine or other treatments. For example, thyroidectomy is done for thyroid nodules or cancer. Parathyroid surgery is for parathyroid adenomas or hyperplasia causing primary hyperparathyroidism.
Doctors decide on surgery after checking hormone levels and doing imaging studies. They look at how bad the gland problem is and if surgery will help.
Benefits and Risks of Surgical Treatment
Endocrine surgery can cure or greatly improve symptoms for some patients. For example, removing a diseased gland can balance hormones again. This can greatly improve a patient’s life.
But, surgery also has risks like infection, bleeding, or damage to nearby tissues. The risks depend on the surgery type. For example, thyroid surgery might harm the vocal cords or cause hypothyroidism.
It’s important for patients and doctors to know the benefits and risks of endocrine surgery. Talking to a skilled endocrine surgeon can help decide if surgery is the right choice.
Thyroid Disorders Requiring Surgical Treatment
Thyroid problems can range from benign nodules to cancerous tumors, often requiring surgical treatment. The thyroid gland, a vital part of the endocrine system, is located in the neck. It plays a key role in regulating metabolism through the production of thyroid hormones.
Cancer: Types and Surgical Approaches
Thyroid cancer is a significant concern among thyroid disorders. There are several types of thyroid cancer, including papillary, follicular, medullary, and anaplastic thyroid cancer. The surgical approach for thyroid cancer typically involves thyroidectomy, which is the removal of part or all of the thyroid gland.
The extent of surgery depends on the type and stage of cancer. For early-stage cancers, a lobectomy (removal of one lobe of the thyroid) might be sufficient. More advanced cases may require a total thyroidectomy. Surgical treatment for thyroid cancer has a high success rate, when detected early.
Hyperthyroidism and Graves’ Disease
Hyperthyroidism is a condition where the thyroid gland produces excess thyroid hormones. Symptoms include weight loss, palpitations, and anxiety. Graves’ disease is the most common cause of hyperthyroidism, an autoimmune disorder that stimulates the thyroid to overproduce hormones.
Surgical treatment for hyperthyroidism, in cases of Graves’ disease, involves removing part or all of the thyroid gland. This approach is considered when antithyroid medications are ineffective or not tolerated. It’s also used when there’s a large goiter causing compressive symptoms.
Large Goiters and Compressive Symptoms
A goiter refers to the enlargement of the thyroid gland. It can cause compressive symptoms such as difficulty swallowing, shortness of breath, or neck discomfort. Large goiters, whether benign or malignant, may require surgical intervention to alleviate these symptoms and improve quality of life.
The decision to surgically treat a goiter depends on its size, the presence of compressive symptoms, and the risk of malignancy. Surgical removal of the goiter can provide significant relief. It is often performed using minimally invasive techniques to reduce recovery time and scarring.
Surgical Management of Parathyroid Disorders
Treatment approaches for parathyroid disorders have evolved, offering better outcomes for patients.These conditions, like hyperparathyroidism, often need surgery to manage well.
Primary Hyperparathyroidism and Parathyroid Adenomas
Primary hyperparathyroidism happens when the parathyroid hormone (PTH) is made too much. This is usually because of a tumor or gland growth. Parathyroidectomy, or removing the gland, is a common treatment.
Parathyroid adenomas are small, non-cancerous tumors that make the gland work too hard.
To treat primary hyperparathyroidism, doctors find and remove the bad gland. Before surgery, tests like ultrasound and sestamibi scans help locate the gland.
Secondary and Tertiary Hyperparathyroidism
Secondary hyperparathyroidism happens when the glands are too active because of low calcium. This is common in people with kidney disease. Tertiary hyperparathyroidism is when the glands keep making too much PTH even after the cause is fixed.
Surgical parathyroidectomy is an option for those who don’t get better with medicine. The surgery aims to cut down PTH by removing the overactive glands. The surgery can be partial or total, depending on the case.
In summary, treating parathyroid disorders needs a plan based on the condition and its severity. Understanding these disorders helps doctors provide better care and improve patient results.
Adrenal Disorders Amenable to Surgical Intervention
The adrenal glands are key in making hormones. Problems with them might need surgery. These issues can be tumors, hormonal imbalances, or other conditions.
Functional and Non-functional Adrenal Tumors
Adrenal tumors can make too much hormone or not at all. The ones that do make hormones can cause Cushing’s syndrome or hyperaldosteronism. Surgical removal is often needed for these tumors, if they’re causing big hormonal problems or might be cancer.
Non-functional tumors don’t make hormones but can be big or grow fast. Whether to remove them depends on their size, how fast they grow, and the patient’s health.
Pheochromocytoma Management
Pheochromocytomas are rare tumors in the adrenal medulla. They can make too much catecholamine, causing high blood pressure and heart problems. Preoperative management is key to control blood pressure and get the patient ready for surgery.
- Preoperative alpha-blockade to control blood pressure
- Beta-blockade to manage tachycardia, if necessary
- Careful monitoring during surgery to manage possible hypertensive crises
Cushing’s Syndrome and Adrenal Surgery
Cushing’s syndrome is when you have too much cortisol. This can be because of tumors in the adrenal glands. Taking out the affected adrenal gland is a treatment for Cushing’s syndrome caused by tumors.
The benefits of adrenal surgery for Cushing’s syndrome are:
- Quick relief from symptoms of too much cortisol
- Potential cure for patients with adrenal tumors
- Improved life quality by reducing cortisol-related problems
In conclusion, surgery is a key treatment for many adrenal disorders, like tumors, pheochromocytoma, and Cushing’s syndrome. The choice to have surgery depends on a full check-up, the type of adrenal disorder, and the surgery’s benefits and risks.
Pituitary Disorders Treated with Surgery
The pituitary gland is called the ‘master gland.’ It can get sick and need surgery. These problems can mess up hormone levels, causing health issues.
Pituitary Adenomas and Their Classification
Pituitary adenomas are tumors in the pituitary gland. They can be small or big, and some make too much hormone. Microadenomas are under 10 mm, and macroadenomas are bigger. Some adenomas are functional, making too much hormone, while others are non-functional.
- Functional adenomas can cause hormonal imbalances, leading to conditions such as Cushing’s disease or acromegaly.
- Non-functional adenomas may not produce hormones but can cause problems due to their size, compressing surrounding structures.
Transsphenoidal Surgery for Pituitary Tumors
Transsphenoidal surgery is a small cut procedure to remove pituitary tumors. It goes through the sphenoid sinus, not needing to open the skull.
This surgery has many benefits:
- It’s safer than old-school surgery.
- It hurts less after.
- You get to go home sooner and feel better faster.
If you have a pituitary problem, seeing an endocrine surgery specialist is key. They can help decide if surgery is right for you. Surgery can really help people with pituitary tumors.
Pancreatic Endocrine Disorders and Surgical Options
Endocrine disorders of the pancreas, like insulinomas and other neuroendocrine tumors, often need surgery. These conditions can really affect a patient’s health. So, a detailed treatment plan is needed.
Insulinomas and Other Pancreatic Neuroendocrine Tumors
Insulinomas are a type of pancreatic neuroendocrine tumor (PNET) that mainly make too much insulin. This leads to low blood sugar. Other PNETs can make different hormones, causing various symptoms. Getting the right diagnosis is key to managing these conditions well.
Characteristics of Pancreatic Neuroendocrine Tumors:
- Variable hormone production
- Diverse clinical presentations
- Potential for malignancy
Surgical Approaches to Pancreatic Endocrine Tumors
Surgery is often the first line of treatment for many pancreatic endocrine tumors. The type of surgery depends on the tumor’s size, location, and the patient’s health.
Surgical options include:
- Enucleation for small, benign tumors
- Pancreatic resection (e.g., Whipple procedure) for larger or malignant tumors
- Minimally invasive techniques when feasible
Tumor Type | Surgical Approach | Considerations |
Insulinoma | Enucleation or resection | Tumor size and location |
Other PNETs | Resection or debulking | Tumor biology and extent |
New surgical methods and better pre-surgery checks have helped improve results for patients with pancreatic endocrine tumors. A team effort is vital for the best care.
Modern Techniques in Endocrine Surgery Procedures
Modern endocrine surgery uses new technologies to improve surgery and recovery. It has made big steps forward, focusing on better patient results and faster healing.
Minimally Invasive Approaches
Minimally invasive surgery is now common, thanks to its benefits. It means smaller cuts, less pain, and quicker healing. Minimally invasive techniques use small ports to reduce damage and speed up healing.
This method also means less scarring, fewer complications, and shorter hospital stays. It’s great for surgeries like thyroid, parathyroid, or adrenal.
Robotic-Assisted Endocrine Surgery
Robotic-assisted surgery is a big leap forward in endocrine surgery. It gives surgeons better control and precision. Robotic systems offer clear views and help with complex surgeries.
This method leads to better results in surgeries like thyroid and parathyroid. It’s perfect for detailed operations that need careful dissection and stitching.
Image-Guided Surgical Techniques
Image-guided surgery uses advanced imaging to guide surgeries. It makes endocrine surgery more accurate. Surgeons can see structures and tumors better.
Image-guided techniques are great for tricky cases, like reoperations or surgeries with big tumors. They lower the risk of problems and improve results.
By using modern methods like minimally invasive, robotic-assisted, and image-guided surgery, endocrine surgery centers offer top care. These advances have changed endocrine surgery, opening new ways to treat diseases.
Preoperative Evaluation and Preparation for Endocrine Surgery
Preoperative evaluation is key in treating endocrine disorders. It prepares the patient for surgery. This step checks for risks and improves care.
Hormonal Assessment and Imaging Studies
A detailed hormonal assessment is essential for diagnosing endocrine disorders. It shows how well the gland works and helps plan surgery. Imaging studies like ultrasound and CT scans help find the gland and check its size.
For thyroid nodules, ultrasound is first used. It checks the nodule’s details and may guide a biopsy.
Medical Optimization Before Surgery
Medical optimization is vital before surgery. It deals with health issues that could raise surgery risks. This includes managing high blood pressure, diabetes, or heart disease.
- Patients with hyperthyroidism may need antithyroid medications to achieve euthyroidism.
- Those with pheochromocytoma require alpha-blockade to control blood pressure.
- Individuals with Cushing’s syndrome may need medication to reduce cortisol levels.
Optimizing the patient’s health lowers surgery risks. This leads to better results.
Postoperative Care and Management Following Endocrine Surgery
The time after endocrine surgery is very important. It needs careful watching to help the patient recover well.
Immediate Postoperative Monitoring
Right after surgery, it’s key to watch for any problems. Monitoring vital signs, managing pain, and caring for the wound are musts. Patients usually stay in a recovery room until they’re ready to move to a regular room.
Studies show that how much a patient moves after surgery can tell us about their recovery. Helping patients move and follow instructions is important to avoid complications.
Long-term Follow-up and Hormone Replacement
Checking in regularly after surgery is important. It helps see if the surgery worked and if there are any lasting effects. This might include hormone replacement therapy for those who had glands removed or changed.
It’s important for patients to know the signs of hormonal issues. They should also stick to their follow-up appointments. Good communication between patients and their healthcare team is essential for long-term care.
Potential Complications and Their Management
Endocrine surgery can lead to complications. It’s important for surgeons and patients to know about these risks. This knowledge helps ensure the best results.
Common Complications of Endocrine Surgery
Like any surgery, endocrine surgery has risks. Some common issues include:
- Infection
- Bleeding or hematoma
- Nerve damage
- Hormonal imbalances
- Reaction to anesthesia
The type of surgery affects the complications. For example, thyroid, parathyroid, or adrenal surgeries have different risks.
Type of Surgery | Common Complications | Management Strategies |
Thyroidectomy | Nerve damage, hypocalcemia | Intraoperative nerve monitoring, calcium supplementation |
Parathyroidectomy | Hypocalcemia, persistent hyperparathyroidism | Calcium and vitamin D supplementation, reoperation if necessary |
Adrenalectomy | Hormonal imbalances, bleeding | Preoperative hormonal control, meticulous surgical technique |
Strategies to Minimize Surgical Risks
To lower the risks of endocrine surgery, several steps can be taken. These include:
- Preoperative evaluation: A thorough check of the patient’s hormones and health.
- Surgical expertise: Having an experienced endocrine surgeon perform the surgery.
- Minimally invasive techniques: Using less invasive methods to reduce trauma and speed recovery.
- Postoperative care: Close monitoring after surgery to catch and treat any issues quickly.
By understanding and managing the risks of endocrine surgery, patients can have better outcomes. This approach reduces the chance of complications.
Choosing a Qualified Endocrine Surgeon
Finding a skilled endocrine surgeon is key to a successful surgery. Your surgeon’s knowledge and experience greatly affect your surgery’s outcome and recovery.
Credentials and Experience to Look For
When looking for an endocrine surgeon, check their credentials and experience. Make sure they are board-certified by the American Board of Surgery or a similar group. This shows they’ve had thorough training and are experts in their field.
Experience matters too. A seasoned surgeon knows the latest methods and has done many surgeries. Ask about their experience with your specific issue or surgery.
“The quality of care you receive is directly related to the qualifications and experience of your healthcare provider.”
— American Medical Association
Questions to Ask Your Surgeon
Before deciding, ask your surgeon some important questions. These might be:
- What experience do you have with endocrine surgery?
- What are the risks and complications associated with my procedure?
- What is your approach to pain management?
- How will you ensure that my hormone levels are properly managed during and after surgery?
- What is your follow-up care plan?
By asking these questions and doing your homework, you can pick a qualified endocrine surgeon who fits your needs.
Conclusion: The Future of Endocrine Surgery
The field of endocrine surgery is changing fast. This is thanks to new research and better surgical methods. Now, surgeons can treat complex endocrine problems better, making patients’ lives better.
New technologies are changing how surgeons work. They use less invasive methods like robotic surgery and image-guided techniques. These help patients heal faster and leave less scar tissue.
The future of endocrine surgery looks bright. More research and development are on the way. This means patients will get even better care for their endocrine issues.
FAQ
What is the role of surgery in treating endocrine disorders?
Surgery is key in treating endocrine disorders. It removes tumors and corrects hormonal imbalances. This helps alleviate symptoms.
What are the different types of endocrine surgery?
There are several types of endocrine surgery. These include thyroidectomy, parathyroidectomy, adrenalectomy, and pituitary surgery. They treat various endocrine disorders.
What is the difference between minimally invasive and traditional endocrine surgery?
Minimally invasive surgery uses smaller incisions. It causes less tissue damage and has faster recovery times. Traditional surgery is more invasive.
How is a qualified endocrine surgeon chosen?
Choosing a qualified surgeon involves checking their credentials and experience. Patients should also ask about their approach to treatment.
What is the importance of preoperative evaluation and preparation for endocrine surgery?
Preoperative evaluation and preparation are vital. They ensure patients are ready for surgery and identify any risks.
What are the possible complications of endocrine surgery?
Complications can include bleeding, infection, nerve damage, and hormonal imbalances. Proper technique and care can minimize these risks.
How is postoperative care and management handled after endocrine surgery?
Postoperative care involves monitoring patients closely. It includes managing pain and complications. Long-term follow-up ensures hormone levels are balanced.
What is the role of hormone replacement therapy after endocrine surgery?
Hormone replacement therapy may be needed after surgery. It replaces hormones missing due to gland removal. This ensures normal hormone levels.
Can endocrine disorders be treated with medication alone?
Some disorders can be managed with medication. But surgery is needed for conditions like thyroid cancer or parathyroid adenomas.
What are the benefits of robotic-assisted endocrine surgery?
Robotic-assisted surgery offers precision and dexterity. It allows for complex procedures with accuracy and minimal invasiveness.
How do image-guided surgical techniques improve endocrine surgery?
Image-guided techniques, like intraoperative ultrasound, enhance surgery’s accuracy. They provide real-time imaging for precise tumor removal.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26462967/