Prevent digestive problems with a healthy gut diet and lifestyle changes. Learn how fiber, exercise, and stress management protect your stomach and liver.
Send us all your questions or requests, and our expert team will assist you.
The digestive system is remarkably resilient. The lining of your stomach regenerates every few days, and the liver is the only organ capable of regrowing itself after injury. However, after a procedure like a colonoscopy, ERCP, or tumor removal (ESD), your body needs specific support to heal correctly without complications.
At Liv Hospital, we view Recovery and Prevention not as a passive waiting period, but as an active phase of treatment. This is where the long-term success of your procedure is determined. Will the polyp come back? Will the ulcer heal? Will the fatty liver reverse?
Our holistic approach combines Medical Surveillance (knowing exactly when to check again) with Nutritional Science (feeding the microbiome). We empower you to become the guardian of your own gut health, turning a medical intervention into a permanent lifestyle upgrade.
Most gastroenterology procedures are performed under deep sedation. While you may wake up feeling alert, your reflexes and judgment are impaired for the rest of the day.


Your digestive lining may be raw or healing. Treating it gently prevents bleeding and pain.
If we removed a large polyp or treated an infection, we want to reduce the volume and frequency of stools to let the bowel rest.
If we stretched your esophagus or placed a stent for cancer.
Without a gallbladder to store bile, your body cannot digest large amounts of fat at once. Eating a greasy burger can cause immediate diarrhea (“dumping syndrome”).

Preventing cancer is not a one-time event; it is a schedule. We follow strict international guidelines (ESGE/ASGE) to determine your next visit based on what we found.

Send us all your questions or requests, and our expert team will assist you.

Your gut contains trillions of bacteria (microbiota) that regulate your immune system. Antibiotics and bowel prep can disrupt this ecosystem.
The laxatives used for prep wash away some good bacteria.
If you have chronic bloating and gas despite normal test results, you may have Irritable Bowel Syndrome (IBS).
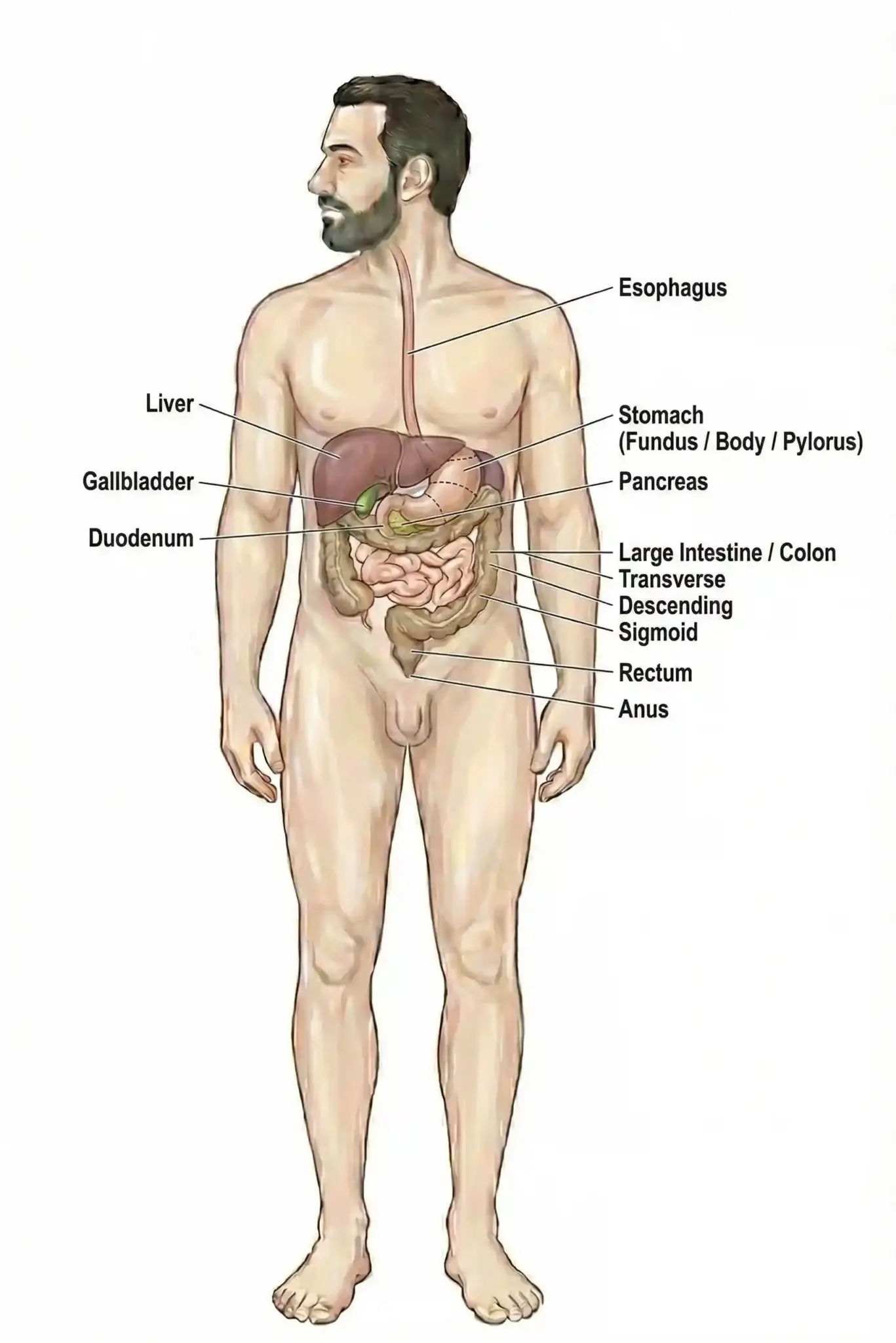
The liver is the body’s filter. If it gets clogged with fat (Steatosis) or scar tissue (Fibrosis), it fails.
There is no pill for fatty liver. The cure is lifestyle.
If you have liver disease (Hepatitis or Cirrhosis), there is no safe amount of alcohol. You must abstain completely. For healthy adults, limit intake to prevent damage.
Stress causes gut symptoms (butterflies in the stomach, diarrhea before a meeting).

Most recoveries are smooth, but complications can happen up to 2 weeks later. Contact your Liv Patient Coordinator immediately if you experience:
If we removed a large polyp (>1cm), we recommend waiting 3–5 days before flying. This is because changes in cabin pressure can expand gas in the bowel, increasing the risk of delayed bleeding or perforation. For simple diagnostic scopes, you can fly the next day.
No. Probiotics are like seeds; they need soil to grow. Once you have re-established a healthy microbiome (usually 1–2 months), a high-fiber diet is enough to maintain it. Long-term probiotic supplements are usually unnecessary unless you have a specific condition like Ulcerative Colitis.
You must wait 24 hours. Alcohol enhances the sedative effect of the anesthesia still in your system, which can slow your breathing or heart rate dangerously.
This is “Bile Acid Diarrhea.” Without a gallbladder, bile drips continuously into the intestines, acting like a laxative. It usually improves within a few weeks as the body adjusts. If it persists, we can prescribe a powder (Cholestyramine) to bind the bile.
Yes. The sedative Propofol causes “anterograde amnesia.” You may have a conversation with the doctor right after waking up but not remember it an hour later. That is why we always give you a written report and explain the results to your companion.


Medical mistakes in hospitals are a big worry. The Institute of Medicine says up to 98,000 deaths annually in the U.S. are due to these

Did you know that nearly 40% of adults worldwide are overweight or obese? Many are looking for effective ways to lose weight. While bariatric surgery
An expert guide on how hernia mesh stays in place. We explore the amazing technology of stitches, tacks, and self-gripping mesh. The choice of technique

It’s estimated that a significant number of patients worldwide are deemed ineligible for hernia surgery due to various health concerns. At our institution, we’ve encountered numerous
Our ultimate guide to hernia treatment success. Discover the amazing 100% curable facts and which repair options are best. With over 700,000 hernia repairs performed

Having a mastectomy can change your life in big ways. Many women worry about how their breasts will look after surgery. Keeping a natural look

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)