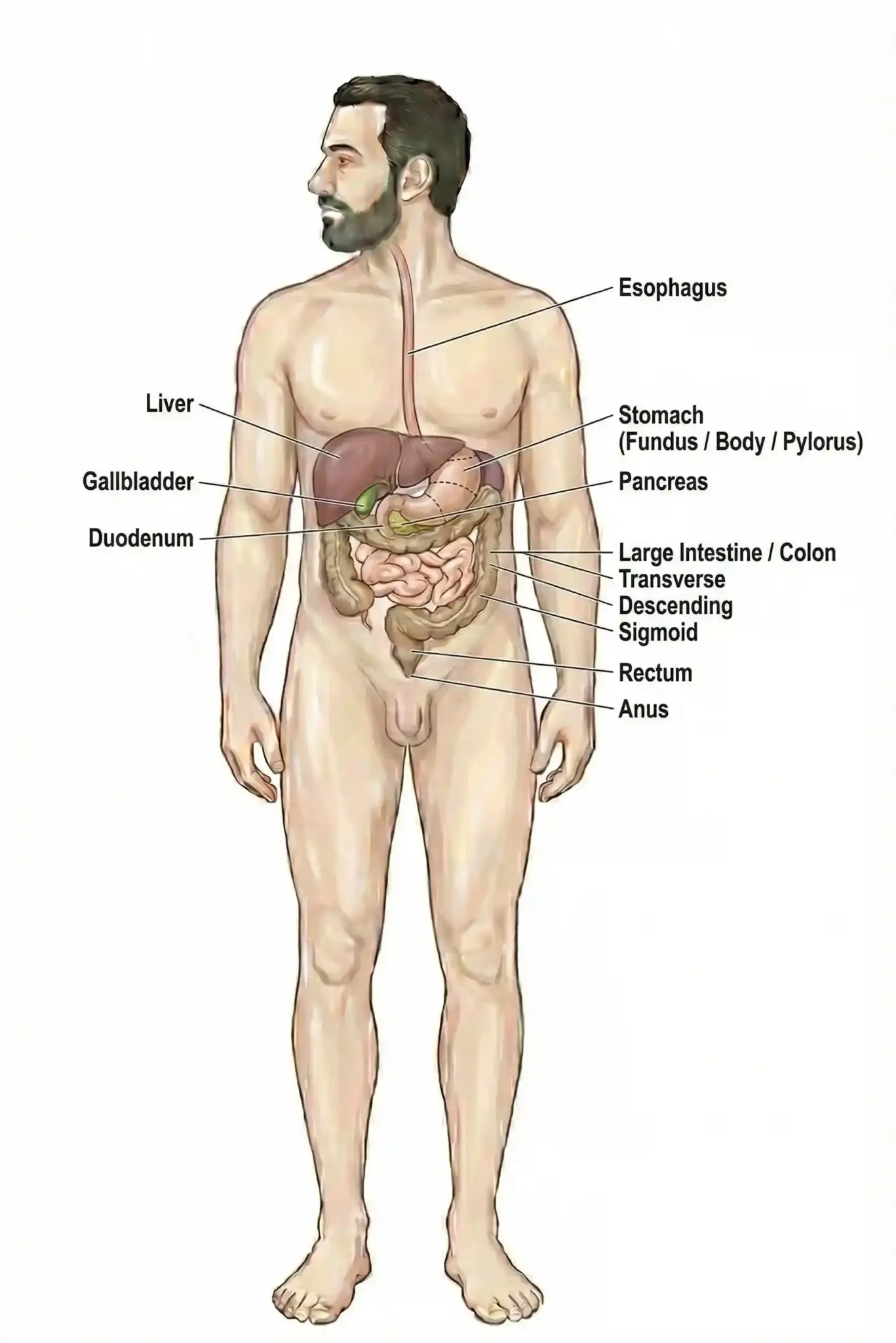
Gastroenterology covers the digestive system. It focuses on diagnosing, treating, and managing conditions of the stomach, intestines, liver, and pancreas.
Send us all your questions or requests, and our expert team will assist you.
Overview and Definition
The digestive system is the engine of the human body. It fuels every cell, regulates our immune system, and even influences our mood—scientists now call the gut our “Second Brain.” When this complex system falters, it affects not just your stomach, but your entire quality of life.
At Liv Hospital, the Department of Gastroenterology and Hepatology is more than just an endoscopy clinic. We are a comprehensive “Digestive Disease Center” dedicated to the diagnosis, treatment, and prevention of diseases affecting the gastrointestinal tract and liver. We have moved beyond the era of simply diagnosing problems; today, we fix them. Using advanced Interventional Gastroenterology techniques, we can remove early-stage tumors, clear bile duct stones, and treat swallowing disorders entirely through an endoscope—without a single incision on your skin.
Whether you are seeking a routine cancer screening or a solution for a complex liver condition, our team combines academic expertise with the latest technology (like AI-assisted colonoscopy) to provide care that is safe, precise, and surprisingly comfortable.
Gastroenterology is the branch of medicine focused on the digestive system and its disorders. It covers a massive territory, from the mouth to the anus, including the accessory organs that aid digestion.


At Liv Hospital, our specialists are often sub-specialized. You might see a Hepatologist for your liver and an Interventional Endoscopist for your polyp removal. This ensures you are treated by a master of that specific organ.
The most significant advancement in our field is the ability to perform “surgery” from the inside. By passing specialized tools through the endoscope, we can treat conditions that previously required major open surgery.

Doctors use several tools to diagnose digestive conditions. Gastroscopy (for the upper GI tract) and colonoscopy (for the lower GI tract) let doctors see inside and take tissue samples. Capsule endoscopy, where you swallow a small camera, helps view the small intestine. Breath tests can find food intolerances or bacterial overgrowth.

Send us all your questions or requests, and our expert team will assist you.

Colonoscopy is the most effective cancer prevention tool in medicine, but it relies on the human eye. At Liv Hospital, we augment human skill with AI.
Digestive diseases are often chronic. We offer dedicated clinics to manage them long-term.
For patients with Crohn’s Disease and Ulcerative Colitis.
For heartburn (GERD), constipation, and swallowing issues.
Incidental cysts are often found on MRI scans. Most are benign, but some are pre-cancerous (IPMN). We use EUS and cyst fluid analysis to determine which ones need surgery and which can be safely watched.


No. At Liv Hospital, it is performed under Deep Sedation (Propofol). You will be asleep. You will not feel the tube, the air, or the biopsy. Most patients wake up asking, “Is it over already?”
The “bowel prep” (cleaning the colon) is the hardest part for most people.
Liv Way: We use modern, low-volume prep solutions (often just 2 glasses split into two doses) combined with plenty of clear water or juice. It is much easier to tolerate.
Yes. This is called a “Double Balloon” or simply “Double Procedure.” It is very common. You receive one sedation, and we check both the stomach (upper) and colon (lower) in the same session. It takes about 30–40 minutes total.
IBD (Inflammatory Bowel Disease): A structural disease (Crohn’s/Colitis). The immune system attacks the gut, causing ulcers and bleeding. It requires strong medication to prevent damage.
No. Diagnostic endoscopy and most therapeutic procedures (like polyp removal or stone removal) are performed through natural body openings (mouth or anus). There are no external cuts and no external scars.


Medical mistakes in hospitals are a big worry. The Institute of Medicine says up to 98,000 deaths annually in the U.S. are due to these

Did you know that nearly 40% of adults worldwide are overweight or obese? Many are looking for effective ways to lose weight. While bariatric surgery
An expert guide on how hernia mesh stays in place. We explore the amazing technology of stitches, tacks, and self-gripping mesh. The choice of technique

It’s estimated that a significant number of patients worldwide are deemed ineligible for hernia surgery due to various health concerns. At our institution, we’ve encountered numerous
Our ultimate guide to hernia treatment success. Discover the amazing 100% curable facts and which repair options are best. With over 700,000 hernia repairs performed

Having a mastectomy can change your life in big ways. Many women worry about how their breasts will look after surgery. Keeping a natural look

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)