Up to 20% of people who have their gallbladder removed deal with diarrhea later on. This is a big worry for those thinking about or who have had a cholecystectomy.
Handling cholecystectomy side effects can be tough, and it’s even harder when they mess with your stomach. Diarrhea after surgery can really disrupt your life.
We’ll look deeper into why this happens and how to handle it. Knowing about post surgery digestion changes is key for those who have had or are going to have this surgery.
Key Takeaways
- Diarrhea is a common issue after gallbladder removal, affecting up to 20% of patients.
- Understanding the causes can help in managing the condition.
- Changes in digestion post-surgery are significant for overall health.
- Managing diarrhea requires a complete approach.
- Post-surgery care is vital for reducing side effects.
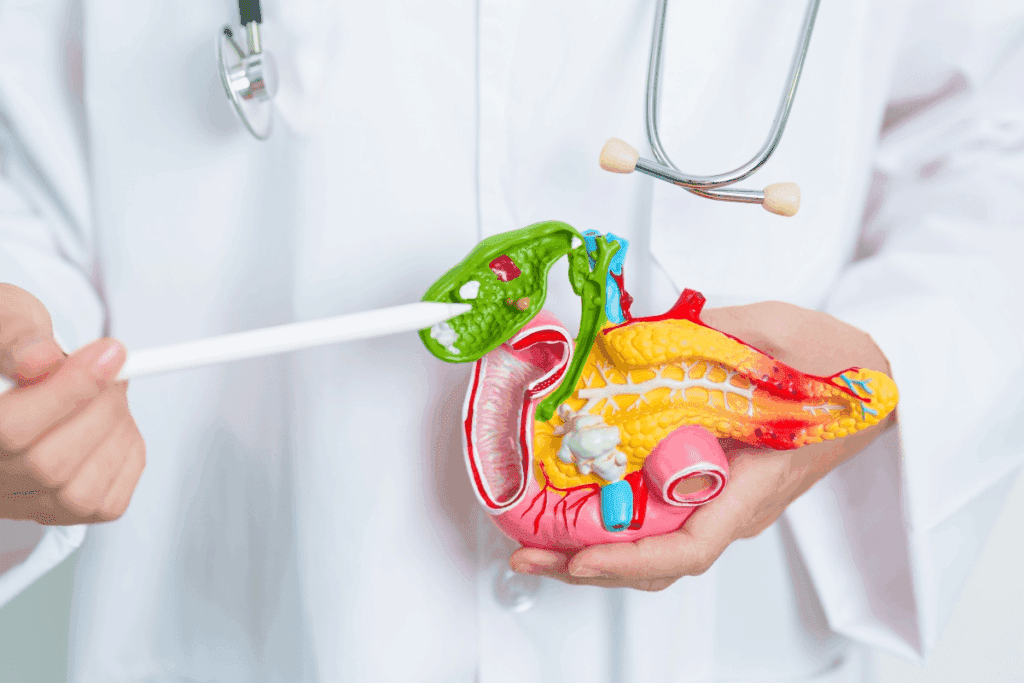
Understanding Gallbladder Function and Removal
It’s important to know how the gallbladder works and why it might need to be removed. The gallbladder plays a crucial role in digesting food, and its removal can alter digestion and bowel movements.
The Role of the Gallbladder in Digestion
The gallbladder holds bile from the liver until it’s needed in the small intestine. This bile helps break down fats. Bile salts make fats easier for enzymes to digest. Without a gallbladder, bile goes straight to the small intestine, causing digestive changes.
Common Reasons for Gallbladder Removal
People often get their gallbladder removed because of gallstones. These stones can cause pain, infection, or blockages. Other reasons include:
- Gallbladder inflammation (cholecystitis)
- Gallstones blocking the bile duct
- Pancreatitis caused by gallstones
These problems can really affect someone’s life, making surgery a good option.
Types of Cholecystectomy Procedures
There are two main ways to remove the gallbladder: laparoscopic and open. Laparoscopic cholecystectomy uses small cuts and a camera. It’s the most common because it has a shorter recovery time and less pain. Open cholecystectomy needs a bigger cut and is for more complicated cases.
Doctors choose the type of surgery based on the patient’s health and the gallbladder disease’s complexity.
Gallbladder Removal Diarrhea: How Common Is It?
Many patients wonder about diarrhea after gallbladder removal. Diarrhea after gallbladder surgery, or post-cholecystectomy diarrhea, affects a lot of people. It’s a common issue for those who have had their gallbladder taken out.
Statistical Overview of Post-Cholecystectomy Diarrhea
Research shows that up to 20% of people get diarrhea after gallbladder surgery. This fact shows why it’s important for patients to know about possible digestive changes after surgery.
Study | Prevalence of Diarrhea |
Study A | 15% |
Study B | 20% |
Study C | 18% |
Short-Term vs. Long-Term Digestive Changes
Digestive changes after gallbladder removal can be short-term or long-term. Short-term changes happen as the body gets used to the new anatomy and bile flow. Long-term changes may last longer and need ongoing care.
a gastroenterologist, says, “The body’s ability to adapt to the absence of a gallbladder varies among individuals. This affects the duration and severity of digestive symptoms.”
“The absence of a gallbladder can lead to changes in bile flow, potentially causing diarrhea in some patients.”
Risk Factors for Developing Digestive Issues
Several factors can make digestive issues, like diarrhea, more likely after gallbladder removal. These include:
- Pre-existing digestive conditions
- The method of cholecystectomy (laparoscopic vs. open surgery)
- Individual variations in bile acid production and absorption
Understanding these risk factors can help set realistic expectations and mitigate digestive changes following surgery.
Why Diarrhea Occurs After Gallbladder Surgery
Without a gallbladder, bile flow changes, which can cause diarrhea. After surgery, bile keeps flowing into the small intestine. This can lead to digestive problems.
Changes in Bile Flow and Storage
The gallbladder stores bile from the liver and releases it into the small intestine. This helps with fat digestion. Without it, bile goes straight to the intestine. This can irritate and cause diarrhea due to bile acid malabsorption.
Bile Acid Malabsorption Explained
Bile acid malabsorption happens when the body can’t reabsorb bile acids well. This leads to too many bile acids in the colon. This can cause diarrhea because bile acids make the colon release more water and electrolytes.
Causes of Bile Acid Malabsorption | Effects on the Body |
Continuous flow of bile into the intestine | Diarrhea due to excessive bile acids |
Poor reabsorption in the ileum | Increased water and electrolyte secretion |
Sphincter of Oddi Dysfunction
The Sphincter of Oddi controls bile and pancreatic juices flow into the small intestine. If it doesn’t work right, it can cause abnormal bile flow. This can lead to digestive problems, including diarrhea.
Fat Digestion Without a Gallbladder
Even without a gallbladder, the body can digest fat. But, the constant flow of bile can cause fat digestion issues for some. This is because the body has to adjust to the new way bile is released.
Understanding these changes is key to managing diarrhea after gallbladder surgery. Knowing how bile flow and storage change can help patients manage their digestive health better after surgery.
Post-Cholecystectomy Syndrome Explained
After gallbladder removal, some patients face a mix of symptoms called post-cholecystectomy syndrome (PCS). This condition includes various gastrointestinal symptoms. These symptoms can really affect a patient’s life quality.
Defining Post-Cholecystectomy Syndrome
Post-cholecystectomy syndrome is when you have stomach pain after gallbladder surgery. PCS is not one single problem. It’s a group of symptoms that can differ from person to person. The reasons for PCS can be many, like changes in bile flow or issues with the sphincter of Oddi.
Common Symptoms Beyond Diarrhea
Diarrhea is a common issue after gallbladder surgery. But PCS can cause more than just that. Symptoms can include:
- Abdominal pain or discomfort
- Bloating and gas
- Nausea and vomiting
- Fatty food intolerance
- Indigestion and dyspepsia
These symptoms can be really tough and interfere with daily life. They need a careful management plan.
Diagnostic Approaches for PCS
Diagnosing PCS starts with a detailed look at your symptoms and medical history. We begin with a thorough patient history and physical check-up. More tests might include:
- Liver function tests
- Imaging studies like ultrasound or MRI
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Hepatobiliary iminodiacetic acid (HIDA) scan
Finding the exact cause is key to creating a treatment plan that fits you.
Immediate Recovery: What to Expect
The time right after gallbladder surgery is key. Knowing what to expect can make recovery easier. Being aware of normal changes and possible issues helps manage your recovery well.
Normal Digestive Changes in the First Week
In the first week, your digestive system will change. You might have diarrhea or constipation because of bile flow changes. You could also feel some pain in your belly, which can be treated with medicine.
To manage these changes effectively, it’s important to adhere to a surgical recovery diet. This diet should be easy on your stomach. It includes low-fat foods, avoiding heavy or greasy meals, and drinking lots of water.
Distinguishing Between Normal Recovery and Complications
Some pain is normal after surgery, but severe pain, fever, or constant vomiting are not. These signs mean you need to see a doctor right away.
Managing Early Digestive Symptoms
Handling early digestive symptoms right is important for a smooth recovery. Eating small, frequent meals helps digestion. Avoid spicy or fatty foods and drink lots of water to prevent constipation.
Hospital Discharge Instructions
When you leave the hospital, you’ll get specific care instructions. These might cover wound care, pain management, and when to come back for check-ups. It’s vital to follow these instructions to avoid complications.
Understanding the immediate recovery phase and managing symptoms helps you feel confident. If you have any worries or questions, always talk to your healthcare provider for help and support.
Long-Term Digestive Changes After Surgery
After having your gallbladder removed, digestive changes can differ a lot. Some people might not notice much, while others could face ongoing digestive problems. Knowing what to expect is key to managing your recovery and improving your life after surgery.
Timeline for Digestive Adaptation
Getting used to life without a gallbladder takes time. At first, your digestive system might have trouble adjusting to the change in bile flow. This can cause various symptoms. But, as your body adapts, these symptoms usually lessen.
- Short-term adaptation (0-3 months): You might deal with diarrhea, fatty stools, or stomach pain because of the change in bile flow.
- Medium-term adaptation (3-6 months): As you get used to it, the symptoms might get less frequent and less severe.
- Long-term adaptation (6 months and beyond): Most people see a big drop in digestive symptoms. But, some might keep experiencing occasional problems.
Persistent Diarrhea Patterns
Diarrhea is a common problem after gallbladder surgery. For some, it can stick around and really affect their life. Bile acid diarrhea happens when bile acids in the colon cause diarrhea.
To handle persistent diarrhea, you might need to change your diet and possibly take medication to help with bile acid absorption.
When the “New Normal” Isn’t Normal
Some digestive changes after gallbladder surgery are expected. But, if symptoms are severe or don’t go away, it might be a sign of a problem. If you have really bad diarrhea, stomach pain, or signs of not absorbing nutrients well, you should see a doctor.
Adjusting to Life Without a Gallbladder
Living without a gallbladder means more than just dealing with immediate symptoms. It’s about making lifestyle changes too. Eating less fat and knowing when to seek medical help are important steps.
Understanding the long-term digestive changes after gallbladder removal helps you manage your recovery better. It’s vital to stay in touch with your healthcare team to handle symptoms and any concerns.
Dietary Strategies to Manage Post-Surgical Diarrhea
Changing your diet can help with digestive problems after gallbladder surgery. A good diet plan is key to managing diarrhea and a smooth recovery. We will look at different ways to help with diarrhea after surgery.
Low-Fat Diet Recommendations
A low-fat diet is often suggested for diarrhea after gallbladder removal. Without the gallbladder, fat digestion is harder. Eating less fat can reduce diarrhea and other stomach issues.
Some tips for a low-fat diet include:
- Choosing lean proteins like poultry and fish
- Opting for low-fat dairy products
- Limiting fried foods and oils
- Selecting low-fat cooking methods like grilling or baking
Foods to Avoid After Gallbladder Removal
Some foods can make digestive problems worse after gallbladder surgery. It’s important to know and avoid these foods to control diarrhea. Common foods to avoid include:
- High-fat foods like fried foods and fatty meats
- Spicy foods that can irritate the digestive tract
- Caffeine and carbonated beverages that can cause digestive discomfort
- High-fiber foods that can be difficult to digest
Beneficial Foods for Digestive Health
Adding certain foods to your diet can help with digestion and reduce diarrhea. Some beneficial foods are:
- Bananas, which are easy to digest and rich in potassium
- Rice, a low-fiber carbohydrate that can help firm up stool
- Applesauce, a easily digestible fruit that can provide essential nutrients
- Probiotic-rich foods like yogurt that support gut health
Meal Timing and Portion Control
Choosing the right foods and timing is also important. Eating smaller, more frequent meals can ease digestion and reduce diarrhea. It’s also good to eat slowly and chew well to help digestion.
By following these dietary tips, people can better manage diarrhea after surgery and improve their digestive health during recovery.
Medical Treatments for Bile Acid Diarrhea
Bile acid diarrhea is common after gallbladder removal. It happens because the body can’t store and release bile right. This leads to too much bile acid in the colon, causing diarrhea.
Bile Acid Sequestrants
Cholestyramine and colestipol are often used to treat this issue. They bind to bile acids in the intestine. This stops them from causing diarrhea. Patients start with a small dose and increase it as needed.
Medication | Initial Dose | Maximum Dose |
Cholestyramine | 4g once daily | 24g daily in divided doses |
Colestipol | 5g once daily | 30g daily in divided doses |
Over-the-Counter Anti-Diarrheal Medications
Loperamide is an over-the-counter option for bile acid diarrhea. It slows down gut movement. This helps the body absorb more water and electrolytes.
Prescription Options for Severe Cases
For severe cases, doctors might prescribe stronger medications. Alosetron is sometimes used off-label for severe diarrhea.
Digestive Enzymes and Supplements
Some people find relief with digestive enzymes and supplements. Pancreatic enzyme supplements help digest fats. This can reduce diarrhea symptoms.
Lifestyle Modifications to Improve Symptoms
Making lifestyle changes can help with digestive problems after gallbladder removal. Stress management, adjusting physical activity, staying hydrated, and getting enough sleep are key. These steps can greatly improve symptoms.
Stress Management Techniques
Stress can make digestive issues worse. That’s why managing stress is important after gallbladder removal. Meditation, yoga, and deep breathing exercises can help. Doing things you enjoy can also help relax you.
Having a regular stress management plan can make you feel better and reduce digestive problems.
Physical Activity Considerations
After surgery, gentle physical activity is good. Walking or swimming can help digestion and health. But, start slow and avoid hard exercises at first.
- Start with short walks and gradually increase the duration.
- Avoid heavy lifting or bending.
- Listen to your body and rest when needed.
Hydration and Electrolyte Balance
Drinking enough water is key for digestion. It helps prevent constipation and dehydration from diarrhea. Also, keeping electrolyte balance right is important, mainly if you have diarrhea a lot. Drinking electrolyte-rich drinks or taking supplements can help.
Drink at least 8-10 glasses of water a day. If a doctor says so, take electrolyte supplements too.
Sleep and Recovery Connection
Getting enough sleep is vital for recovery. Aim for 7-8 hours of sleep each night. It helps with digestion and overall health. A regular sleep schedule and a calm sleep space can improve sleep quality.
By making these lifestyle changes, people can manage their symptoms better and live a better life after gallbladder removal.
When to Consult Your Doctor About Post-Surgical Diarrhea
Knowing when to see a doctor after gallbladder surgery is key to a smooth recovery. Some digestive changes are normal after surgery. But, some symptoms need quick attention from your doctor.
Warning Signs of Complications
After gallbladder removal, watch out for complications. Look out for:
- Severe abdominal pain that doesn’t subside
- High fever or chills
- Vomiting blood or persistent vomiting
- Signs of dehydration, such as excessive thirst, dark urine, or dizziness
Any of these symptoms might mean you need to see a doctor right away.
Symptoms Requiring Immediate Medical Attention
Some symptoms after gallbladder surgery need quick doctor visits. These include:
- Persistent diarrhea that lasts more than a few days
- Bloody stools or black, tarry stools
- Severe diarrhea with abdominal pain or cramping
If you’re experiencing these, seeing a doctor is important to avoid more problems.
Preparing for Your Doctor’s Appointment
Before your doctor visit, get ready. Here’s what to do:
- Keep a symptom diary to track your symptoms and what triggers or helps them
- List all your medications, including over-the-counter drugs and supplements
- Write down any questions or concerns you have about your symptoms or recovery
Being prepared will help you have a better conversation with your doctor.
Follow-up Care Schedule
Follow-up care is important for your recovery. Your doctor will schedule a follow-up visit a few weeks after surgery. The exact time depends on your needs and the surgery details.
It’s important to stick to your follow-up care schedule. This helps your doctor monitor your recovery and address any issues quickly.
Other Digestive Complications After Gallbladder Surgery
After gallbladder surgery, other digestive problems can occur. These issues can greatly affect a person’s life. It’s important to know what causes them and how to manage them.
Constipation and Irregular Bowel Movements
Constipation or irregular bowel movements can happen after gallbladder removal. These changes in bowel habits are part of the body’s adjustment. Eating a high-fiber diet and drinking plenty of water can help.
Acid Reflux and GERD
Acid reflux and GERD can also occur after gallbladder surgery. The surgery can put more pressure on the lower esophageal sphincter. This can cause heartburn and regurgitation. Changing your diet and eating smaller meals can help manage these symptoms.
Bloating and Gas
Bloating and gas are common after gallbladder surgery. The body may struggle to digest certain foods. Changing your diet and avoiding foods that cause gas can help. Over-the-counter medications can also offer relief.
Abdominal Pain Patterns
Abdominal pain can persist or start after gallbladder surgery. It’s important to figure out the cause of the pain. This could be related to sphincter of Oddi dysfunction or other factors. Talking to a healthcare provider is key to finding the right treatment.
Knowing about these digestive problems can help patients deal with their recovery better. Working with healthcare providers and making smart lifestyle choices can help manage these issues. This way, people can live well without a gallbladder.
Special Considerations for Different Patient Groups
Some patient groups face special challenges after gallbladder surgery. The recovery and symptoms can vary based on age, health, and other factors.
Elderly Patients and Recovery Challenges
Elderly patients have unique recovery challenges after gallbladder surgery. Age-related decline in physical function and health issues can make healing harder. We need to tailor care for older adults carefully.
It’s important to watch them closely and create personalized care plans. This helps avoid complications and aids in a smoother recovery.
Patients with Pre-existing Digestive Disorders
Those with digestive disorders like IBS or IBD may see exacerbated symptoms after surgery. It’s key to manage these conditions well before and after surgery to avoid digestive problems.
A comprehensive treatment plan that covers both the gallbladder issue and the digestive disorder is vital. This approach can lead to better results.
Diabetic Patients After Cholecystectomy
Diabetic patients need careful management of their blood sugar after gallbladder surgery. Surgery stress and changes in digestion can affect blood sugar levels.
Diabetic patients should work closely with their doctors. They should adjust their treatment plans and keep a close eye on their blood sugar.
Gender Differences in Post-Surgical Symptoms
Research shows gender differences in post-surgical symptoms after gallbladder surgery. Knowing these differences helps tailor care for men and women.
More studies are needed to understand these differences. This will help develop gender-sensitive treatment approaches.
Patient Experiences and Coping Strategies
Patients who have had their gallbladder removed share many experiences. They talk about the changes in their digestion and how to deal with them. This is key to keeping their quality of life good.
Common Patient Concerns
Managing digestive symptoms, like diarrhea, is a big worry for many. Learning about the causes and finding ways to manage them helps a lot.
Patients worry about the unpredictable nature of their symptoms. They also worry about how these symptoms affect their daily life. To help, they need to make dietary changes, adjust their lifestyle, and sometimes get medical help.
Quality of Life Considerations
The quality of life after gallbladder removal depends on managing symptoms well. Eating right and drinking plenty of water helps reduce discomfort and aids in recovery.
- Eating smaller, more frequent meals to ease digestion
- Avoiding foods that trigger or worsen symptoms
- Staying hydrated to prevent dehydration, which is common with diarrhea
Support Resources and Communities
Having support from others can greatly help. Support groups, online forums, and healthcare providers offer valuable advice and reassurance.
Connecting with others who have gone through the same thing is very helpful. They can share strategies and learn new ways to manage symptoms.
Communicating with Family About Your Condition
Talking openly with family and friends about your condition is important. It helps them understand and support you better. Patients should be able to talk about their needs, symptoms, and any worries they have.
“It’s been helpful for me to explain to my family what I’m going through and how they can support me. It’s made a big difference in my recovery.” – Patient testimonial
By sharing their experiences and helpful strategies, patients can create a supportive environment. This environment helps them recover and adjust to life after gallbladder removal.
Conclusion
Managing diarrhea after gallbladder removal is key for those who have had cholecystectomy. We’ve talked about how not having a gallbladder can change bile flow, leading to diarrhea. Post cholecystectomy syndrome, which includes digestive problems like diarrhea, is a big worry for many.
To handle diarrhea, making dietary changes is important. Eating less fat and avoiding foods that can make symptoms worse helps. Medical treatments like bile acid sequestrants and anti-diarrheal meds can also help. Plus, managing stress and staying hydrated are important for feeling better.
By understanding the causes of diarrhea after gallbladder removal and applying these strategies, patients can improve their well-being. It’s vital to talk to healthcare providers for advice on managing digestive issues after surgery.
FAQ
What is post-cholecystectomy syndrome, and how is it related to diarrhea after gallbladder removal?
Post-cholecystectomy syndrome (PCS) is a set of symptoms that happen after the gallbladder is removed. Diarrhea is one of these symptoms. PCS is diagnosed when these symptoms are present and affect daily life.
How common is diarrhea after gallbladder surgery, and what are the risk factors?
Diarrhea is common after gallbladder surgery, affecting many patients. Factors like differences in bile acid production and pre-existing digestive issues can increase the risk.
What dietary changes can help manage diarrhea after gallbladder removal?
Eating a low-fat diet and avoiding certain foods can help. Also, adding foods that are good for digestion is beneficial. Paying attention to meal timing and portion sizes is important too.
Are there any medical treatments available for managing bile acid diarrhea?
Yes, treatments include bile acid sequestrants and anti-diarrheal medications. For severe cases, prescription options are available. Digestive enzymes and supplements may also be suggested.
How can lifestyle modifications improve symptoms of diarrhea after gallbladder surgery?
Managing stress, staying active, drinking enough water, and keeping electrolytes balanced can help. Getting enough sleep and following a recovery plan are also key.
When should I consult my doctor about post-surgical diarrhea?
See your doctor if diarrhea is persistent or severe. Also, if you notice warning signs of complications or need immediate medical help. Regular follow-up appointments are important for monitoring your health.
Can other digestive complications occur after gallbladder surgery, and how are they managed?
Yes, issues like constipation, acid reflux, bloating, and abdominal pain can happen. Management depends on the complication and may include dietary changes, medications, or lifestyle adjustments.
Are there special considerations for different patient groups after gallbladder surgery?
Yes, elderly patients, those with digestive disorders, diabetic patients, and different genders face unique challenges. Tailored approaches are needed to manage symptoms effectively.
How can I cope with diarrhea and other symptoms after gallbladder removal?
Coping strategies vary, but seeking support and talking to family about your condition are common. Making adjustments to improve your quality of life is also important.
What are the signs of bile acid malabsorption after gallbladder surgery?
Signs include persistent diarrhea and other digestive symptoms. Diagnosis involves tests to confirm bile acid malabsorption.
References
BMJ (British Medical Journal). Evidence-Based Medical Insight. Retrieved from https://bmjopen.bmj.com/content/12/2/e046172[4