What causes thin blood in children? Find out does ibuprofen thin your blood. Understand this dangerous anti-platelet effect and crucial advice for pediatric use.
Thrombocytopenia, or low platelet count, is a condition that can lead to excessive bleeding and bruising in children. We will explore the various causes of this condition, which can significantly impact a child’s health and well-being.
Several factors contribute to the development of thrombocytopenia in children. Genetic predispositions play a significant role, as do viral infections such as Epstein-Barr virus and hepatitis C. Also, autoimmune diseases like lupus can cause this condition.
Understanding these causes is key for proper care and treatment. We aim to give a detailed overview to help parents and caregivers make informed decisions about their child’s health.
Key Takeaways
- Thrombocytopenia is characterized by low platelet counts in children.
- Genetic conditions, viral infections, and autoimmune diseases are major causes.
- Understanding the causes is vital for timely diagnosis and treatment.
- Viral infections like Epstein-Barr virus and hepatitis C can cause thrombocytopenia.
- Autoimmune diseases such as lupus are also a contributing factor.
Understanding Thin Blood in Children
Thrombocytopenia, or thin blood, is a condition where children have too few platelets. Platelets help blood clot, so a low count can cause problems. These include easy bruising and bleeding gums.
Medical Definition of Thrombocytopenia
Thrombocytopenia means having fewer than 150,000 platelets per microliter of blood. Normal counts are between 150,000 and 450,000. A count below this range shows thrombocytopenia.
It can be caused by many things, like bone marrow problems or infections. It can also happen because of certain medicines.
There are two types: acute and chronic. Acute is more common in kids and often gets better by itself. Chronic may need ongoing care.
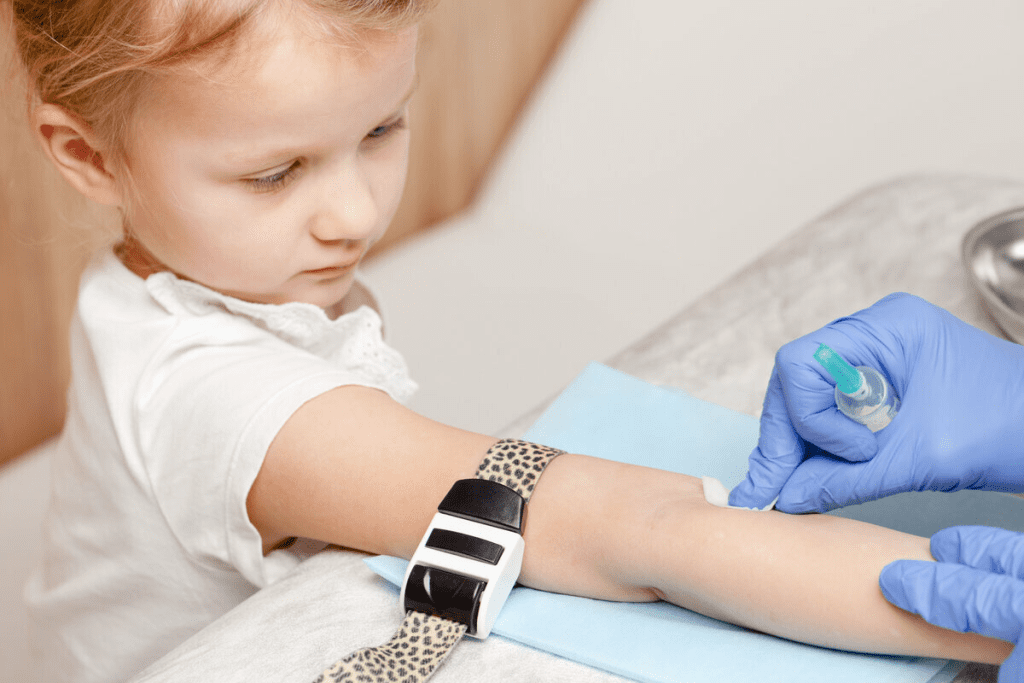
How Blood Thickness is Measured
Blood thickness is checked with a Complete Blood Count (CBC) test. This test looks at many parts of the blood. It checks red and white blood cells, hemoglobin, hematocrit, and platelets.
- A CBC test takes a blood sample from a vein in the child’s arm.
- The sample goes to a lab for analysis.
- The results show how healthy the child’s blood is, including platelet count.
Prevalence in Different Age Groups
Thrombocytopenia can happen in kids of all ages. The reasons and how common it is can change with age.
- Newborns might get it from their mom or because of something in the womb.
- Older kids might get it from infections, autoimmune diseases, or bone marrow problems.
- Teenagers can get it for the same reasons as adults, like chronic diseases or side effects from medicines.
Knowing how common it is in different ages helps doctors treat it better.
Common Symptoms of Thin Blood in Children
It’s important to know the signs of thin blood in kids to get them help early. Thin blood, or thrombocytopenia, can cause health problems if not treated quickly. We’ll look at common symptoms to help parents and caregivers know when to seek medical help.
Physical Signs to Watch For
Children with thin blood may show several physical signs. These include:
- Easy Bruising: Bruises can show up with little or no injury.
- Nosebleeds: Frequent or long-lasting nosebleeds are a sign.
- Petechiae: Small spots on the skin, often on legs, arms, or torso.
- Prolonged Bleeding: Bleeding that lasts longer than usual after an injury.
Behavioral Changes
Children with thin blood may also act differently. These changes can include:
- Fatigue: They might seem more tired or sluggish than usual.
- Irritability: They could get more irritable or have mood swings.
- Lack of Energy: They might not want to do things they used to enjoy.
These changes can be small, so watching your child’s behavior is key.
When to Seek Medical Attention
If you see any of these signs, get medical help right away:
- Severe Bleeding: Heavy bleeding that doesn’t stop with pressure.
- Frequent Bruising: Bruising that happens often without reason.
- Other Concerning Symptoms: Any other symptoms that worry you or seem odd.
Getting help early can make a big difference for kids with thin blood. If you’re worried about your child’s symptoms, talk to a doctor.
Genetic Causes of Thin Blood in Children
Thin blood in children often comes from inherited conditions. These conditions make it hard for blood to clot. We’ll look at the genetic factors that lead to this issue in kids.
Inherited Bleeding Disorders
Inherited bleeding disorders are a big reason for thin blood in kids. Hemophilia and von Willebrand disease are examples. They affect how blood clots.
Hemophilia happens when there’s not enough clotting factor VIII or IX. This leads to long bleeding episodes. Von Willebrand disease is caused by a lack or problem with von Willebrand factor. This protein is key for platelets to stick together and form clots.
Other Genetic Factors
Other genetic factors can also cause thin blood in kids. For example, some genetic conditions affect platelet production or function. This can lead to thrombocytopenia, or low platelet count.
Genetic syndromes like Wiskott-Aldrich syndrome can affect both platelet count and function. This increases the risk of bleeding. Knowing these genetic factors helps doctors diagnose and treat thin blood in kids better.
By finding the genetic causes of thin blood, doctors can create better treatment plans. This helps improve the lives of kids with this condition.
Viral Infections That Cause Thin Blood
Viral infections are a big reason for thin blood in kids. It’s important to know how they work to help kids get better. Some viruses mess with platelet production or destroy them, causing low platelet counts.

Epstein-Barr Virus
The Epstein-Barr virus (EBV) causes “mono” or the “kissing disease.” It’s not common for EBV to make kids’ platelets low. But, it’s key to watch platelet counts in kids with EBV to spot problems early.
Hepatitis C
Hepatitis C can also make blood thinner. It can cause low platelet counts over time. This happens because the virus attacks platelets or messes with the bone marrow.
Other Viral Infections
Other viruses can also make blood thinner in kids. These include:
- Cytomegalovirus (CMV), which can cause low platelets in newborns.
- HIV, where low platelets are a common problem.
- Dengue fever, a mosquito-borne virus that can severely lower platelet counts.
It’s vital to understand how these viruses affect blood thickness. Doctors need to watch for signs of low platelets in kids with these infections.
By knowing how viral infections can cause thin blood, we can help kids better. We can make sure they get the right care to get better and stay healthy.
Autoimmune Conditions and Thin Blood
Autoimmune conditions are a big reason for thin blood in kids. It’s key to know how they affect us. These diseases happen when our immune system attacks our own body parts. This can lower platelet counts, causing thrombocytopenia.
Lupus and Its Effects on Blood
Lupus is a chronic autoimmune disease that can harm many parts of the body, including the blood. It makes the immune system attack platelets, leading to thrombocytopenia. Kids with lupus might feel tired, have joint pain, and get skin rashes, along with bleeding problems.
Managing lupus requires a team effort, including medicines to control the immune system. We help families create a care plan that meets their child’s physical and emotional needs.
Immune Thrombocytopenia (ITP)
ITP is an autoimmune condition that lowers platelet counts because of immune system attacks. In kids, it can start suddenly after a viral infection. Symptoms can be mild bruising or serious bleeding. Some kids might get better on their own, but others need treatment to increase platelet counts.
It’s important to know why ITP happens to find the best treatment. We use tests and medical checks to make a treatment plan that fits each child.
Age-Related Differences in Autoimmune Responses
Autoimmune responses change as kids get older. Young kids might get acute conditions, while older kids and teens often get chronic diseases like lupus. Knowing these differences helps us give the right care and support.
We adjust our treatments based on each child’s age, health, and specific condition. This way, we aim to lessen the disease’s impact on their life and future health.
Does Ibuprofen Thin Your Blood? Medication Effects in Children
It’s important to know how medicines like ibuprofen change blood thickness in kids. Many parents wonder, does ibuprofen thin your blood, especially when giving it to children for pain or fever.

Common Medications That Affect Blood Thickness
Some medicines can change how blood clots and gets thicker in kids. Ibuprofen and aspirin are two common ones. They can make blood thinner, which is good for pain but might be a concern for clotting.
Other drugs, like antibiotics and anticoagulants, can also change blood thickness. It’s vital to tell your doctor about all medicines your child takes to avoid bad reactions.
Safe Medication Practices for Children
To keep kids safe with medicines, always follow the dosage your doctor or the label says. Watch for signs of bleeding or bruising, too, if the medicine can thin blood.
- Always talk to a healthcare provider before giving your child any medicine.
- Stick to the recommended dosage.
- Know the possible side effects, like bleeding signs.
Monitoring Blood Thickness During Medication Use
Keeping an eye on blood thickness is important when kids take medicines that can change it. We suggest working with your doctor to check your child’s blood counts and adjust the medicine if needed.
By staying informed and careful, parents can keep their kids safe while using medicines to help their health.
Bone Marrow Disorders and Thin Blood
It’s key to know about bone marrow disorders to treat thin blood in kids well. The bone marrow makes blood cells, like platelets, which help blood clot. When the bone marrow is sick, it can make fewer platelets, causing thin blood or thrombocytopenia.
Leukemia: The Most Common Childhood Cancer
Leukemia is a cancer that messes with the bone marrow, making too many white blood cells. This can push out other blood cells, like platelets, causing thin blood. Acute lymphoblastic leukemia (ALL) is the top leukemia in kids, and it can cause thin blood.
Symptoms of leukemia in kids include:
- Pale skin
- Fatigue
- Recurring infections
- Easy bruising or bleeding
Other Bone Marrow Conditions
Other than leukemia, other bone marrow issues can mess with blood making. These include:
- Aplastic anemia, where the bone marrow can’t make blood cells.
- Myelodysplastic syndromes, where blood cells aren’t made right.
- Bone marrow failure from infections or toxins.
Early Detection and Intervention
Finding bone marrow disorders early is key for good treatment. Regular check-ups and tests can spot these issues early. Complete Blood Count (CBC) is a test used to find blood disorders, like thin blood.
There are ways to help, like:
- Medicine to get the bone marrow to make more blood cells.
- Blood transfusions to raise platelet counts quickly.
- In some cases, a bone marrow transplant might be needed.
We know how important quick and right diagnosis is for treating bone marrow issues. Spotting signs early lets parents get their kids the right care.
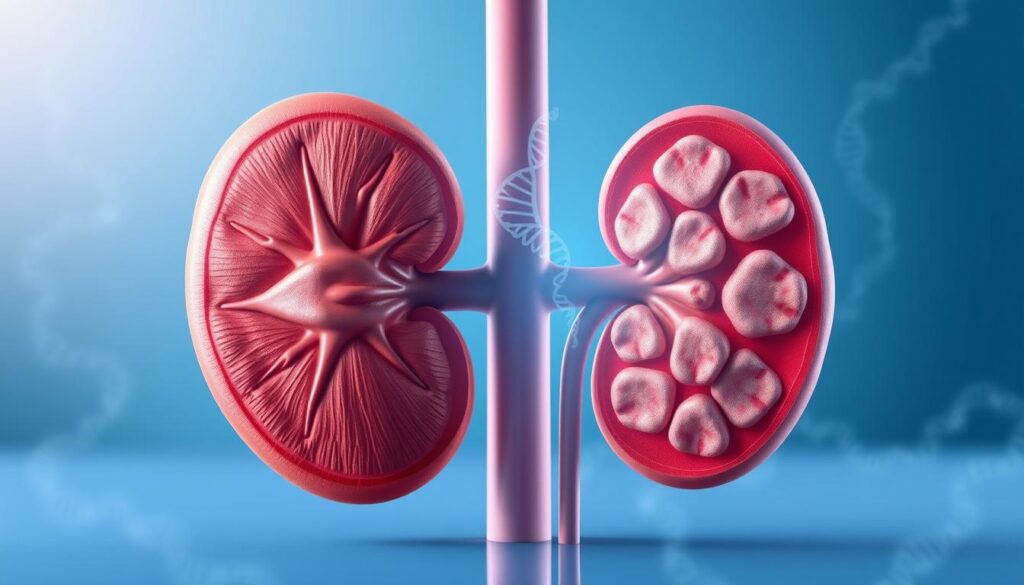
Thick Blood vs. Thin Blood: Understanding Both Conditions
It’s important to know the difference between thick and thin blood in kids. Both can affect how well blood works, but they have different reasons, signs, and ways to treat them.
Causes of Thick Blood in Children
Thick blood, or hypercoagulability, in kids can come from many things. Genetic conditions are a big part, as some kids are born with a higher risk of blood clots. Dehydration also plays a role, making blood thicker and more viscous. Other causes include some medicines and health issues that affect blood clotting.
Thick Blood Symptoms
The signs of thick blood can be hard to spot. Common symptoms include frequent headaches, dizziness, and fatigue. In serious cases, it can lead to blood clots, which can cause strokes or heart attacks. Spotting these signs early is key to acting fast.
Comparing Treatment Approaches
Treating thick and thin blood needs different methods. For thick blood, fixing the cause is often the first step, like rehydration for dehydration or changing medicines. For genetic cases, anticoagulant therapy might be needed to stop blood clots. Thin blood, on the other hand, might need treatments to help it clot better or fix underlying issues like autoimmune disorders or side effects from medicines.
Getting a precise diagnosis is vital for the right treatment. Knowing if a child has thick or thin blood is the first step to managing and treating their condition effectively.
Anemia and Its Relationship to Thin Blood
Anemia is a big health issue in kids all over the world. It happens when there aren’t enough red blood cells or hemoglobin. This makes the blood thin and less able to carry oxygen.
Global Statistics on Childhood Anemia
Anemia is a big problem for kids everywhere. Anemia is more common in places where food and healthcare are hard to get. It’s bad for kids’ health now and can hurt their growth later.
The World Health Organization (WHO) says anemia is a big issue worldwide. It affects kids in rich and poor countries. It’s often caused by not enough iron, which is very important for health.
Iron Deficiency and Its Impact
Iron deficiency is the main reason for anemia in kids. It happens when the body can’t make enough hemoglobin. Hemoglobin is what lets red blood cells carry oxygen.
Iron deficiency anemia can make kids tired, weak, and less able to think clearly. It’s not just about not eating enough iron. It can also happen when kids grow fast or lose blood too much.
Nutritional Interventions
Good nutrition is key to fighting anemia in kids. Eating foods rich in iron is very important. Iron-rich foods include red meat, fish, beans, and fortified cereals. Vitamin C helps the body absorb iron better, so eating foods high in vitamin C is good too.
We suggest that parents and caregivers give kids a diet full of iron. Sometimes, iron supplements are needed, but only with a doctor’s advice.
Diagnosing Blood Thickness Issues in Children
Figuring out blood thickness problems in kids takes a few steps. We look at their medical history, do a physical check, and run tests. It might seem scary, but it’s key to find out what’s wrong and how to fix it.
Common Blood Tests
Blood tests are key in finding blood thickness issues in kids. The main test is the Complete Blood Count (CBC). It checks different parts of the blood, like:
- Red blood cell count
- White blood cell count
- Platelet count
- Hemoglobin levels
A CBC can spot problems in blood cell counts. A top pediatric hematologist says, “A CBC is often the first step in diagnosing blood disorders. It gives us a quick look at the child’s blood cell counts and can show possible issues.”
“A CBC is a key tool for figuring out a child’s blood disorder.”
Additional Diagnostic Procedures
Other tests might be needed to find blood thickness issues in kids. These include:
- Bone marrow aspiration or biopsy to check how well the bone marrow makes blood cells
- Imaging tests like ultrasound or CT scans to find any underlying conditions
- Coagulation studies to see if the blood clots right
These tests help doctors understand the child’s condition better. They help make a good treatment plan.
Interpreting Test Results
Understanding test results needs skill and careful thought. We work with parents to explain the results and what they mean for their child’s health. For example, if a CBC shows low platelets, we might do more tests to find the cause.
Getting the diagnosis right is vital. It helps make a good treatment plan. This ensures the best care for kids with blood thickness disorders.
Modern Treatment Approaches for Thin Blood in Children
Managing thin blood in kids has changed a lot. Now, we use both old and new treatments. This way, kids get care that really fits their needs.
Medical Interventions
Medical treatments are key for kids with thin blood. Doctors use medicines to help platelets grow or find the cause. For example, corticosteroids help platelets grow.
In some cases, IVIG is used to help the immune system. This can also help platelets.
Medicines like corticosteroids and IVIG are big help. They make kids feel better and live better lives. The right medicine depends on the cause, the child’s health, and how they react.
Innovative Therapies
New treatments are changing how we treat thin blood in kids. Gene therapy is one of them. It fixes genes that cause thin blood, which might cure it.
Other new treatments target specific disease paths. They work better and have fewer side effects. Scientists are always finding new ways to help.
Liv Hospital’s Approach to Pediatric Blood Disorders
At Liv Hospital, we treat kids with thin blood in a special way. Our team works with families to make plans that fit each child.
We use many tools and treatments to care for kids. We always try to use the newest treatments. This way, kids get the best care.
We mix medical knowledge with caring to help kids. We want to make their lives better and their outcomes better too.
Conclusion
It’s important to understand thin blood in kids to help them get the right care. We’ve looked at why it happens, its symptoms, and how doctors diagnose it. This includes genetic, viral, and autoimmune causes.
We’ve also talked about how to treat it. This includes both traditional and new treatments. Knowing this helps parents and caregivers support their kids better.
Places like Liv Hospital use a team approach to help kids with blood disorders. This ensures kids get the best care. In short, knowing about thin blood in kids is key to helping them stay healthy.
FAQ
What is thrombocytopenia, and how is it related to thin blood in children?
Thrombocytopenia is when a child has too few platelets in their blood. This is often called thin blood. It can happen for many reasons, like genes, viruses, or autoimmune diseases.
How is blood thickness measured in children?
Doctors use a complete blood count (CBC) test to check blood thickness. This test looks at platelets, red blood cells, and white blood cells.
What are the common symptoms of thin blood in children?
Kids with thin blood might bruise easily, get nosebleeds, or bleed a lot after injuries. They might also feel tired, irritable, and have small spots on their skin.
Can certain medications like ibuprofen thin the blood in children?
Ibuprofen and other NSAIDs can slow down platelet function. But they’re not true blood thinners. It’s important to use medications safely and watch blood thickness closely.
What are the genetic causes of thin blood in children?
Some genetic conditions, like hemophilia or von Willebrand disease, can cause thin blood in kids.
How do viral infections like Epstein-Barr virus and hepatitis C contribute to thin blood?
Viruses like Epstein-Barr and hepatitis C can cause thrombocytopenia. They affect platelet production or increase their destruction.
What is the difference between thick blood and thin blood?
Thick blood has more red blood cells or platelets, making it thicker. Thin blood has fewer platelets or they don’t work right.
How is anemia related to thin blood in children?
Anemia, or low red blood cells, can be linked to thin blood. Some conditions cause both problems.
What diagnostic tests are used to assess blood thickness issues in children?
Doctors use CBC tests, bone marrow biopsies, and other tests to check platelet count and blood health.
What are the modern treatment approaches for thin blood in children?
Treatments include medicines to boost platelet count, new therapies, and care from experts like Liv Hospital.
What causes thick blood in children?
Thick blood can be due to genes, dehydration, or medical conditions that raise red blood cell or platelet counts.
How do autoimmune conditions like lupus affect blood thickness in children?
Lupus and other autoimmune diseases can destroy platelets. This leads to thin blood in kids.
References
- Kumar, G., et al. (2024). Clinical profile of thrombocytopenia in pediatric patients. International Journal of Contemporary Pediatrics, 11(4), 1500-1506. https://www.ijpediatrics.com/index.php/ijcp/article/view/6093
- Jan, M. A. (2004). Thrombocytopenia in children. Journal of Postgraduate Medical Institute, 18(3). https://jpmi.org.pk/index.php/jpmi/article/view/900