Last Updated on December 2, 2025 by Bilal Hasdemir
Many people facing breast cancer or high risk worry about mastectomy. They fear losing their nipple. A mastectomy removes the whole breast and sometimes chest muscle to fight cancer. But, you don’t always lose your nipple.
We know how important nipple preservation is. We aim to clear up the confusion about mastectomies and nipple care. We also want to talk about reconstructive surgery options.
Does nipple removal mastectomy happen? Get the shocking facts about nipple-sparing vs. traditional procedures in our ultimate guide.
Key Takeaways
- Understanding the different types of mastectomies and their impact on nipple preservation.
- Factors influencing the decision to remove or preserve the nipple.
- Available reconstructive surgery options after a mastectomy.
- The importance of discussing personal preferences with your healthcare provider.
- Considering prophylactic caution for those at high risk.
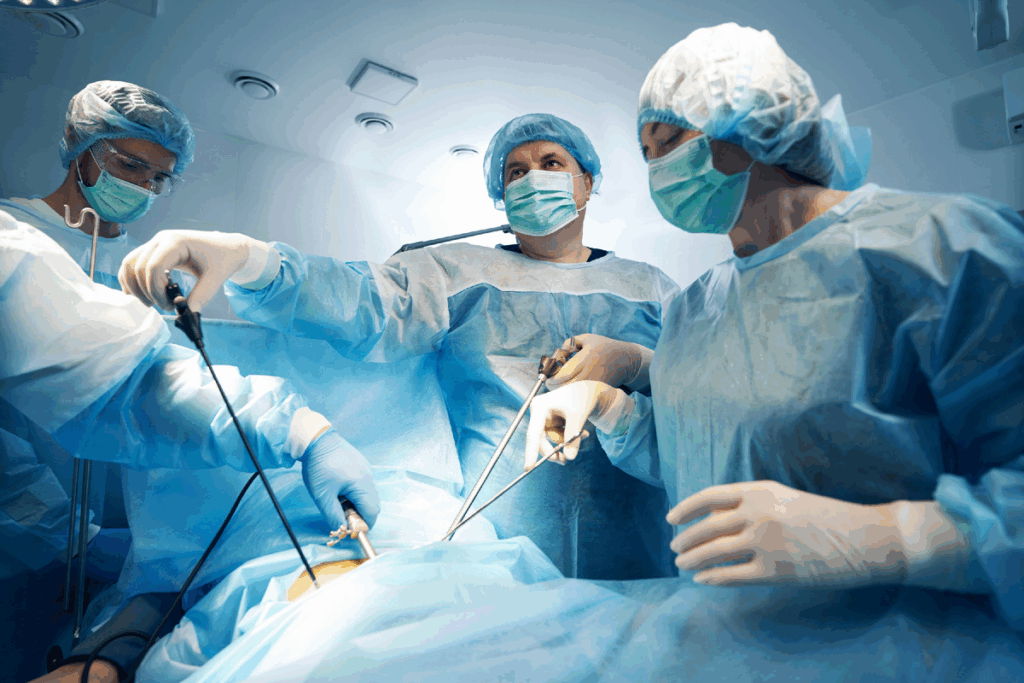
Understanding Mastectomy Procedures
It’s key for patients to grasp the details of mastectomy procedures. A mastectomy removes breast tissue and sometimes nearby tissue. The choice to have a mastectomy depends on the cancer’s stage and type, the patient’s health, and personal wishes.
Types of Mastectomies
There are many types of mastectomies, each for different reasons and outcomes. A simple or total mastectomy removes all breast tissue, skin, and the nipple and areola. It also includes removing lymph nodes under the arm to check for cancer spread.
Other types include:
- Nipple-sparing mastectomy: This keeps the nipple and areola while removing the breast tissue. It’s a detailed procedure not for everyone.
- Skin-sparing mastectomy: This removes the breast tissue and nipple-areola but keeps the skin. It’s good for immediate reconstruction.
- Modified radical mastectomy: This removes the breast tissue, nipple-areola, and some lymph nodes under the arm.
Reasons for Performing Mastectomies
Mastectomies are mainly for treating breast cancer. The decision to have a mastectomy depends on the cancer’s stage, type, and size. It also considers the patient’s genetic risk for breast cancer. Sometimes, a mastectomy is suggested as a preventive measure for those at high risk.
It is essential to understand the risks associated with mastectomy, including the potential for contralateral removal and the implications of unnecessary bilateral surgery. Understanding these risks and the lack of survival benefit in some cases helps in making informed choices.
Nipple-Sparing vs. Nipple-Removing Mastectomy
Knowing the difference between nipple-sparing and nipple-removing mastectomies is key. The choice depends on cancer stage, tumor location, and health. It’s a personal decision that should be well thought out.
What Is Nipple-Sparing Mastectomy?
Nipple-sparing mastectomy removes breast tissue but keeps the nipple, areola, and skin. It’s for patients with certain cancer stages and tumor locations. NCCN guidance says it’s a good option for some, highlighting the need for individualized care.
This surgery keeps the nipple-areola complex, aiming for a natural look after reconstruction. But, it’s important to check if the cancer is near the nipple. This could make the surgery not possible.
Benefits of Nipple-Sparing Procedures
Nipple-sparing mastectomy has many benefits. It looks more natural and can make patients feel better about their body. It’s a big plus for those worried about how they’ll look after surgery.
- Looks more natural
- Can make patients feel better mentally
- Looks better after reconstruction
When Nipple-Removing is Necessary
In some cases, removing the nipple is needed. This is when cancer is near or in the nipple. The decision is based on careful evaluation and individualized care plans.
| Procedure | Indications | Benefits |
| Nipple-Sparing Mastectomy | Cancer not involving the nipple, early-stage cancer | Preserves natural appearance, potentially less psychological impact |
| Nipple-Removing Mastectomy | Cancer involving or close to the nipple, advanced cancer | Ensures removal of all cancerous tissue, necessary for cancer treatment |
Talking to a healthcare provider about risks and benefits is vital. It helps avoid overtreatment concern and ensures the best treatment plan. Understanding each procedure helps patients make choices that fit their health and preferences.
Factors Influencing Nipple Removal Decisions
Choosing to remove or keep the nipple during a mastectomy is a big decision. It’s influenced by many factors. We know this choice is very important for patients going through mastectomy.
Several key factors are considered when deciding about the nipple. These include the cancer’s stage and type, the patient’s health, and the surgeon’s advice.
Breast Cancer Stage and Type
The stage and type of breast cancer are key in deciding about the nipple. For example, women with small, not aggressive tumors might choose nipple-sparing mastectomy. But, more aggressive cancers might need the nipple to be removed.
Genetic mutations also play a role. Some patients with certain genetic mutations might prefer nipple-sparing mastectomy, based on their risk and health.
Patient’s Individual Health Concerns
A patient’s health and concerns are also important. We look at their medical history, current health, and surgery risks.
In some cases, active surveillance might be suggested. This allows for a more personalized care plan.
Surgeon’s Recommendations
The surgeon’s advice is very important. We work with patients to understand their needs and make personalized recommendations.
Our approach is all about shared decision-making. We discuss the pros and cons of each option. This way, patients can make an informed choice that fits their situation.
| Factor | Description | Impact on Nipple Removal Decision |
| Breast Cancer Stage and Type | The stage and aggressiveness of the cancer | More advanced cancers may require nipple removal |
| Patient’s Health Concerns | The patient’s overall health and medical history | Certain health concerns may influence the decision to remove or preserve the nipple |
| Surgeon’s Recommendations | The surgeon’s professional judgment and expertise | Personalized recommendations based on the patient’s unique situation |
Psychological Impact of Nipple Removal
Having a mastectomy and losing a nipple can change a person’s life. The emotional side of losing a nipple is a big part of the treatment. It’s something we need to think about carefully.
Emotional Responses to Mastectomy
People react differently to losing a nipple. Some feel relieved, while others struggle with how it changes their body image. It’s important to understand and help with these feelings.
Patients might feel sad, anxious, or depressed. The change in how they see themselves can hurt their self-esteem and relationships. We offer emotional support to help them through this tough time.
Coping Strategies Post-Surgery
Dealing with the loss of a nipple needs a variety of strategies. Counseling, support groups, and relaxation techniques can help. We suggest trying different things to find what works best.
- Counseling: It’s a safe place to talk about feelings and worries.
- Support Groups: They connect people with others who understand what they’re going through.
- Relaxation Techniques: Like meditation and yoga, they can help manage stress and improve mood.
Importance of Support Systems
Having a strong support system is key for those going through mastectomy and nipple removal. Family, friends, and healthcare professionals are all important. They offer emotional support and help with recovery.
We believe in a team approach to handle the emotional side of losing a nipple. Working with a team of healthcare professionals ensures patients get the care they need. This care addresses both their physical and emotional health.
| Support System | Description | Benefits |
| Family and Friends | Emotional support and practical help | Reduced feelings of isolation, improved mental health |
| Support Groups | Community of individuals with similar experiences | Shared understanding, coping strategies |
| Multidisciplinary Healthcare Team | Comprehensive care addressing physical and emotional needs | Improved quality of life, better risk–benefit balance |
By understanding the emotional impact of nipple removal and providing strong support, we can help patients. It’s important to work with a team to ensure patients get the care they need. This way, they can have the best possible outcome in terms of quality of life.
Reconstructive Surgery Options
For those facing mastectomy, reconstructive surgery offers many choices to keep the breast’s look when it’s safe. This surgery is key in the healing process for many. We give full care, talking about the good and bad of each reconstructive method.
Immediate vs. Delayed Reconstruction
Reconstruction can happen right after mastectomy or later. Immediate reconstruction does both surgeries at once, cutting down on the number of surgeries and recovery time. Delayed reconstruction lets patients focus on cancer treatment first before more surgery.
| Reconstruction Timing | Benefits | Considerations |
| Immediate Reconstruction | Reduced overall surgeries, potentially less emotional distress | Requires coordination between surgical teams, may not be suitable for all patients |
| Delayed Reconstruction | Allows focus on cancer treatment, potentially fewer complications | May involve more total surgeries, longer overall recovery time |
Techniques for Nipple Reconstruction
Nipple reconstruction helps make the breast look natural again. There are different methods, like local flap and nipple-areola complex reconstruction. Nipple nerve reconstruction is a more advanced method that tries to bring back feeling in the nipple-areola area, making the reconstruction better.
“Reconstruction can be a powerful tool in a patient’s recovery, giving not just physical but also emotional healing.”
Alternatives to Traditional Mastectomy
Breast cancer treatment has changed, giving patients new options. While mastectomy is needed for many, others might have less invasive choices. Every patient’s situation is different, so it’s key to look at all treatment options.
Lumpectomy as a Possible Option
A lumpectomy removes the tumor and some tissue but keeps most of the breast. It’s often followed by radiation to kill any cancer cells left. Lumpectomy instead of mastectomy is good for early-stage cancer or those wanting to keep more of their breast.
Talking to your doctor about lumpectomy instead is important. It might keep your breast looking more natural and reduce surgery’s emotional impact. But, there are risks like cancer coming back and needing more treatments like radiation.
If Nipple-Sparing Isn’t Suitable
Not everyone can have a nipple-sparing mastectomy. The choice to remove the nipple depends on the cancer’s stage and type. If not suitable, there are other ways to make your breast look like it did before.
It’s right to worry about overtreatment. Knowing the risks of bigger surgeries is important. By understanding your situation and talking to a doctor, you can choose what’s best for you.
Post-Surgical Care and Recovery
After a mastectomy, the recovery starts with post-surgical care. We focus on individualized care to meet each patient’s needs. This ensures they get the best treatment plan for them.
Good post-surgical care includes managing pain and watching for complications. These steps help improve patient outcomes and their quality of life.
Managing Post-Operative Pain
Controlling pain after a mastectomy is key for a smooth recovery. We use many strategies to reduce discomfort. These include medication, physical therapy, and other pain management methods.
- Medication: We choose pain relief meds based on each patient’s needs.
- Physical Therapy: Gentle exercises help with stiffness and mobility.
- Alternative Techniques: Acupuncture or relaxation therapy can also help.
Monitoring for Complications
Watching for complications is vital in post-surgical care. We look for signs of infection, reactions to anesthesia, and other issues. Catching these early helps us deal with them effectively.
| Potential Complications | Signs and Symptoms | Actions to Take |
| Infection | Redness, swelling, increased pain, fever | Contact your healthcare provider immediately |
| Reaction to Anesthesia | Nausea, vomiting, difficulty breathing | Seek immediate medical attention |
| Seroma or Hematoma | Swelling, pain, or fluid accumulation at the surgical site | Notify your healthcare provider for evaluation |
By watching for complications and acting fast, we can reduce risks. This supports a healthier recovery for our patients.
Long-term Effects of Nipple Removal
It’s important to know the long-term effects of nipple removal for those thinking about mastectomy. Losing a nipple can greatly affect a person’s life, changing how they feel physically and emotionally.
Changes in Sensation
Nipple removal can cause changes in how the chest feels. You might feel numb, more sensitive, or lose all feeling. These changes can last forever and affect your quality-of-life impact.
Talking to your doctor about these possible changes is key. They can help you understand the risk–benefit balance of your treatment. A multidisciplinary approach to care can also help. This includes using rehabilitation and counseling to manage these changes.
It’s important to consult multidisciplinary teams. They can help with both physical and emotional needs.
Impact on Body Image
Removing a nipple can deeply affect how you see your body. You might feel sad, anxious, or depressed. This change can lower your self-esteem and confidence, impacting your life quality.
Having a support system is key. Counseling and support groups can help you deal with these feelings. Healthcare providers can offer a care plan that helps with both physical and emotional healing.
Resources for Patients
Dealing with mastectomy is more than just medical treatment. It needs a full support system. We know how important it is to give patients the tools to handle the emotional and informational parts of their journey.
Support Groups and Counseling
Support groups and counseling are key for emotional support after mastectomy. They offer a place to share, get advice, and meet others facing similar issues.
A study in the Journal of Clinical Oncology shows support groups improve life quality and coping skills.1 Our team helps find the best support services for each patient, ensuring they get the care they need.
“The emotional support I received from my support group was invaluable. It helped me navigate the complex feelings associated with mastectomy and reconstruction.”
A breast cancer survivor
Educational Materials on Mastectomy
Having the right information is key for patient care. We provide various resources like brochures, online content, and consultations with experts.
| Resource Type | Description | Benefits |
| Support Groups | Regular meetings with others who have experienced mastectomy | Emotional support, shared experiences |
| Counseling Services | One-on-one or group counseling sessions with licensed therapists | Personalized guidance, coping strategies |
| Educational Materials | Brochures, online resources, and consultations on mastectomy and reconstruction | Informed decision-making, reduced anxiety |
We aim to improve our patients’ experience by providing these resources. Our goal is to support them fully, not just during surgery. We want to help them recover and heal fully.
Conclusion: Making Informed Decisions
Understanding mastectomy procedures and the factors that influence nipple removal is key for patients. We stress the need for shared decision-making between patients and their healthcare providers. This ensures the best outcomes for everyone.
Personalized Approach to Care
Creating a personalized care plan is essential. It should meet your unique needs and concerns. Talking with your doctor helps you make informed choices that improve your quality‑of‑life.
We urge patients to have open talks with their healthcare providers. Discussing options and outcomes together helps patients make informed decisions. This leads to better health and well-being for all.
FAQ
What is a mastectomy, and when is it necessary?
A mastectomy is a surgery that removes the breast tissue. It’s needed for breast cancer patients, based on the cancer’s stage and type. The patient’s health and personal wishes also play a role.
What are the different types of mastectomies, and how do they differ?
There are several mastectomy types, like nipple-sparing and nipple-removing. The choice depends on the cancer’s stage, location, and the patient’s health.
What is nipple-sparing mastectomy, and who is eligible for it?
Nipple-sparing mastectomy keeps the nipple. It’s for early-stage breast cancer patients or those at high risk. Eligibility varies, based on cancer stage, location, and health.
What are the benefits of nipple-sparing mastectomy?
It offers better looks and less emotional impact. It helps keep the patient’s body image and intimacy, improving their life quality.
When is nipple-removing mastectomy necessary?
It’s needed when cancer is near or in the nipple, or when a bigger surgery is required. The decision is based on the patient’s situation.
What are the alternatives to traditional mastectomy?
Options include lumpectomy, which removes the tumor and some tissue. It’s good for early-stage cancer or when mastectomy isn’t suitable.
What are the long-term effects of nipple removal?
Nipple removal can change sensation, body image, and life quality. Patients might feel numbness, pain, or emotional distress.
How can patients cope with the psychological impact of nipple removal?
Support from loved ones, groups, and counseling helps. A team can offer the needed resources and guidance through mastectomy challenges.
What are the reconstructive surgery options available after mastectomy?
Options include immediate and delayed reconstruction. Nipple reconstruction is also available, aiming to restore body image and intimacy.
How can patients make informed decisions about their mastectomy care?
Discussing options with the doctor and understanding treatments helps. A personalized care plan ensures the best outcomes and quality of life.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6952567/