Last Updated on December 2, 2025 by Bilal Hasdemir
Diverticulitis affects millions of people worldwide. It causes severe abdominal pain. If not treated, it can be life-threatening. When is a hospital visit for diverticulitis needed? Our critical guide reveals the shocking, 5 worst symptoms that mean go to the ER.
Diverticulitis can be scary, even more so during a flare-up. It happens when the colon wall’s diverticula get inflamed. This leads to symptoms that can be mild or severe.
It’s important to know when to go to the hospital. If your symptoms get worse or you have severe pain, you need to seek help. Understanding when a hospital visit is needed is key.
Key Takeaways
- Diverticulitis can cause severe abdominal pain and potentially life-threatening complications.
- Understanding when to seek medical care is critical to prevent further complications.
- A hospital visit may be necessary if symptoms worsen or if certain severe symptoms occur.
- Prompt medical attention can help ensure proper treatment and prevent long-term damage.
- Severe diverticulitis symptoms require immediate medical care to prevent serious complications.
Understanding Diverticulitis
It’s important to know about diverticulitis to spot its signs and get medical help fast. This condition affects the digestive system, causing pain and can lead to serious issues if not treated right.
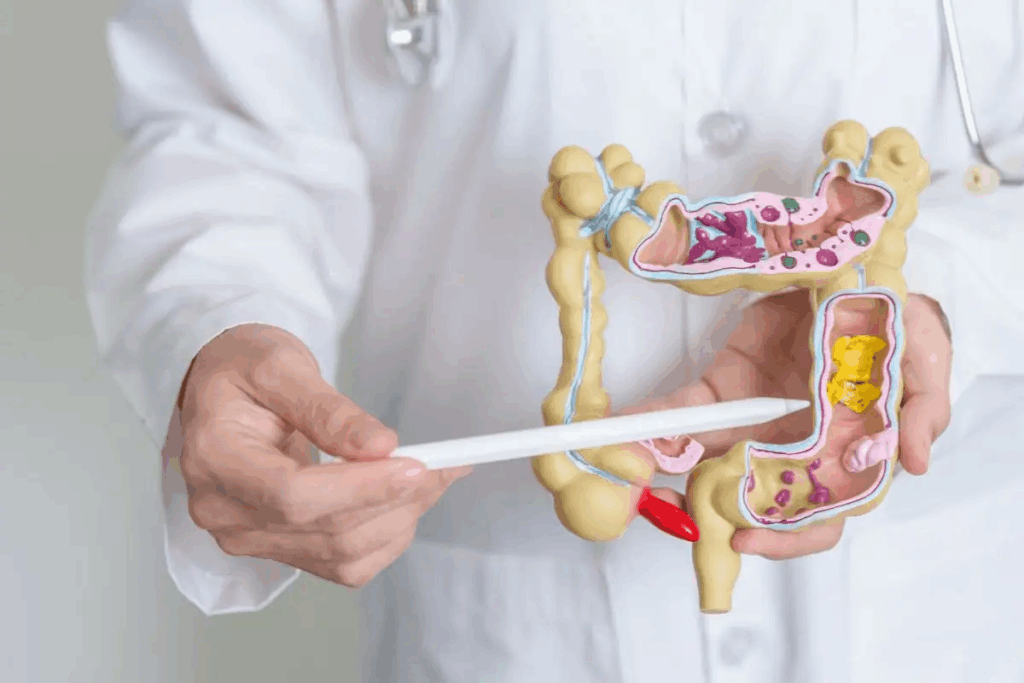
What is Diverticulitis?
Diverticulitis happens when diverticula, small pouches in the colon wall, get inflamed or infected. It’s a part of diverticular disease, which includes both the presence of these pouches and their inflammation or infection.
The exact reason for diverticulitis isn’t always known. But it’s thought to be caused by a mix of things like a low fiber diet, age, and other health conditions that can affect bowel habits or the colon’s structure.
Causes and Risk Factors
There are several things that can make you more likely to get diverticulitis. These include:
- A diet low in fiber, which can cause constipation and more pressure in the colon.
- Age, as diverticulitis is more common in older adults.
- Obesity, which can raise the risk of getting diverticulitis.
- Lack of physical activity, which can lead to constipation and more pressure inside the colon.
- Smoking, a habit that has been linked to a higher risk of diverticulitis.
Understanding these risk factors can facilitate early detection and help you seek timely medical care for diverticulitis.
Symptoms to Watch For
The symptoms of diverticulitis can differ but often include:
- Abdominal pain, usually in the lower left, which can be mild or severe.
- Changes in bowel habits, like constipation or diarrhea.
- Fever and chills, signs of an infection.
- Nausea and vomiting, which can cause dehydration if not handled right.
Spotting these symptoms early is key to getting medical help and avoiding serious problems like abscess formation or perforation of the colon.
Identifying Severe Symptoms
It’s important to know when to go to the hospital for diverticulitis. This condition can be mild or severe. Knowing the signs of a serious case can help avoid bigger problems.
Abdominal Pain and Discomfort
Severe stomach pain is a big warning sign. This pain doesn’t go away and can make your belly feel sore. Sometimes, it’s so bad it stops you from doing everyday things.
The pain’s location and how bad it is can change. Many people feel pain on the lower left side. If your pain is sudden, very bad, or gets worse, get help right away.
Changes in Bowel Habits
Changes in how you go to the bathroom can also mean trouble. You might throw up a lot, have trouble going, or go too often. Seeing blood in your stool is a big red flag that needs quick doctor attention.
These issues can make you very dehydrated or upset your body’s balance. Keep an eye on your bathroom habits and tell your doctor if anything unusual happens.
Fever and Chills
Fever and chills mean your body is fighting an infection. A fever over 100.4°F (38°C) with chills is a sign of a serious fight. This could mean your diverticulitis is getting worse.
Watch your temperature and tell your doctor if you have a fever or chills. Not treating infections can lead to serious problems like abscesses or a hole in your colon.
Symptom | Description | Action Required |
Severe Abdominal Pain | Persistent pain, tenderness, often on the lower left side | Seek immediate medical care |
Changes in Bowel Habits | Constipation, diarrhea, blood in stool, persistent vomiting | Monitor closely, report to healthcare provider |
Fever and Chills | Fever above 100.4°F (38°C), chills indicating infection | Seek medical evaluation, possible hospital stay |
Knowing these severe symptoms helps you act fast. This can prevent serious problems and improve your health.
When to Seek Medical Help
It’s important to know when to get medical help for diverticulitis. This condition can sometimes cause serious problems that need quick medical care.
Time to Go to the Hospital
If you have any of these symptoms, you need to go to the hospital right away:
- Severe abdominal pain that doesn’t get better or gets worse.
- Signs of perforation, like sudden, severe pain, fever, and nausea.
- Uncontrolled pain management, when your pain doesn’t go away with medicine.
- Vomiting blood or passing black tarry stools, which means you might be bleeding inside.
- Fever above 101°F (38.3°C) that keeps going or comes with chills.
A report from the Pennsylvania Health Care Cost Containment Council says quick medical help is key for some stomach problems. Spotting these signs early can stop bigger issues.
Symptom | Description | Action |
Severe Abdominal Pain | Persistent or worsening pain | Seek immediate medical help |
Signs of Perforation | Sudden severe pain, fever, nausea | Go to the emergency room |
Uncontrolled Pain | Pain not relieved by medication | Contact your doctor or seek emergency care |
Consulting Your Primary Care Physician
If your symptoms are not too bad, start by seeing your primary care doctor. They can check you out, give advice on how to feel better, and send you to a specialist if needed.
Your primary care doctor can help you:
- Learn about your diagnosis and treatment choices.
- Manage your symptoms and avoid serious problems.
- Plan for any follow-up care you might need.
By teaming up with your healthcare team, you can handle diverticulitis well and lower the chance of serious issues.
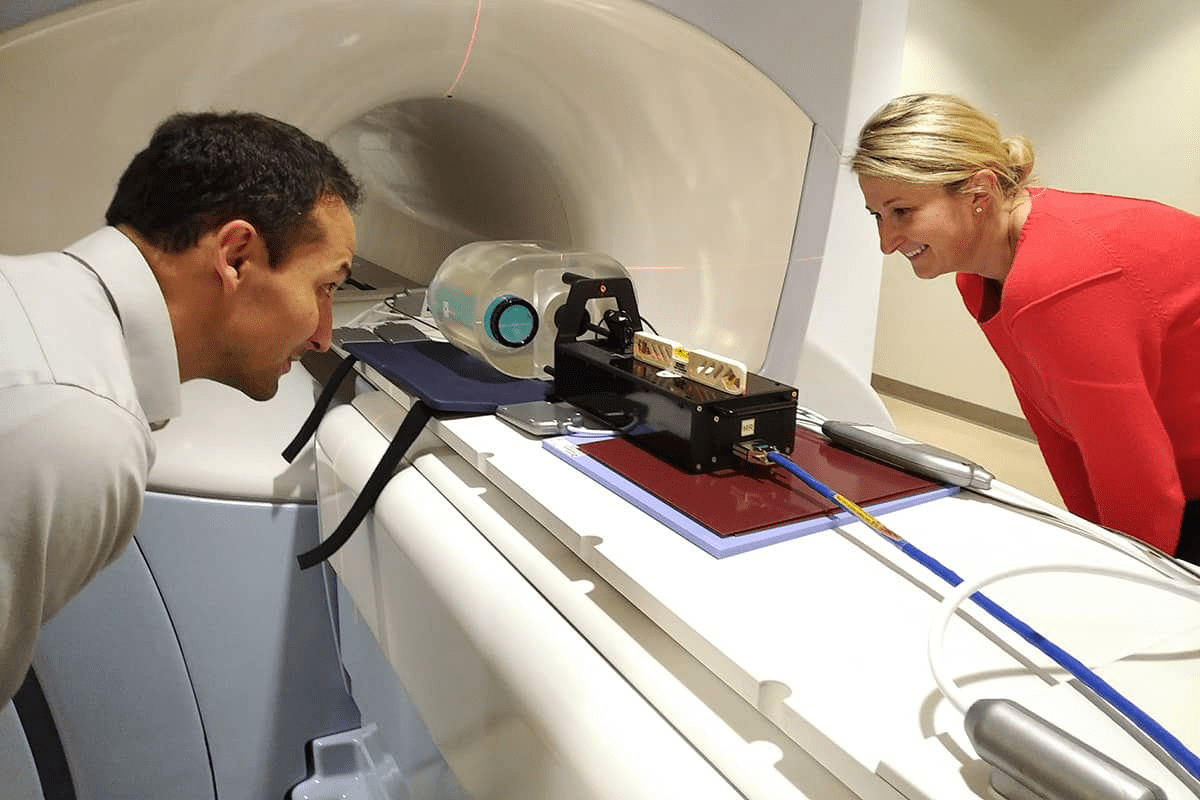
Diagnostic Tests for Diverticulitis
When symptoms suggest diverticulitis, doctors use various tests to confirm the diagnosis. These tests help figure out how severe it is. They are key to choosing the right treatment and avoiding complications.
Imaging Tests
Imaging tests are essential for diagnosing diverticulitis and seeing how far it has spread. The main imaging tests are:
- CT Scans: CT scans are the top choice for diagnosing diverticulitis. They show detailed images of the abdomen. This helps doctors spot inflammation, abscesses, or perforations in the colon.
- X-Rays: X-rays are not as detailed as CT scans but can help rule out other causes of pain. They check for things like bowel obstructions or a perforation.
Imaging Test | Purpose | Benefits |
CT Scan | Diagnose diverticulitis, assess severity | Highly sensitive, detailed images |
X-Ray | Rule out other causes of abdominal pain | Quick, widely available |
Laboratory Tests
Laboratory tests add more information to what imaging studies show. Key tests include:
- Blood Tests: Blood tests can show signs of infection or inflammation. They also check the patient’s overall health and look for complications.
- Stool Samples: Stool tests can find blood in the stool or other signs linked to diverticulitis.
Laboratory Test | Purpose | Benefits |
Blood Test | Detect infection, inflammation | Provides information on overall health |
Stool Sample | Identify blood or abnormalities | Helps in assessing gastrointestinal health |
By looking at imaging and laboratory test results together, doctors can accurately diagnose diverticulitis. They can then create a treatment plan that fits the patient’s needs.
Treatment Options in the Hospital
When someone is in the hospital for diverticulitis, doctors create a treatment plan just for them. They aim to ease symptoms, avoid serious problems, and help the patient get better.
Medications for Pain and Infection
Medicine is key in treating diverticulitis. Antibiotics fight off infections, which often happen with diverticulitis. The doctor picks the right antibiotic based on how bad the infection is and the patient’s health.
To help with pain, analgesics are given. The doctor decides what kind and how much based on the patient’s pain and medical history. Sometimes, intravenous fluids are given to keep the patient hydrated and help them recover.
Surgical Interventions: When They Are Necessary
In serious cases of diverticulitis or when complications happen, surgery might be needed. Surgery could be to take out the bad part of the colon or to drain abscesses. The decision to have surgery depends on how bad the symptoms are, if there are complications, and the patient’s health.
Treatment Option | Description | Indications |
Antibiotics | Medications to combat bacterial infection | Presence of infection or abscess |
Analgesics | Medications for pain management | Significant pain or discomfort |
Surgical Resection | Removal of the affected portion of the colon | Severe diverticulitis, perforation, or abscess |
Drainage of Abscess | Procedure to drain abscesses associated with diverticulitis | Presence of abscess |
Knowing about the treatments for diverticulitis is important for managing it well. Tailoring treatment plans to each patient helps doctors improve outcomes and lower the chance of serious problems.
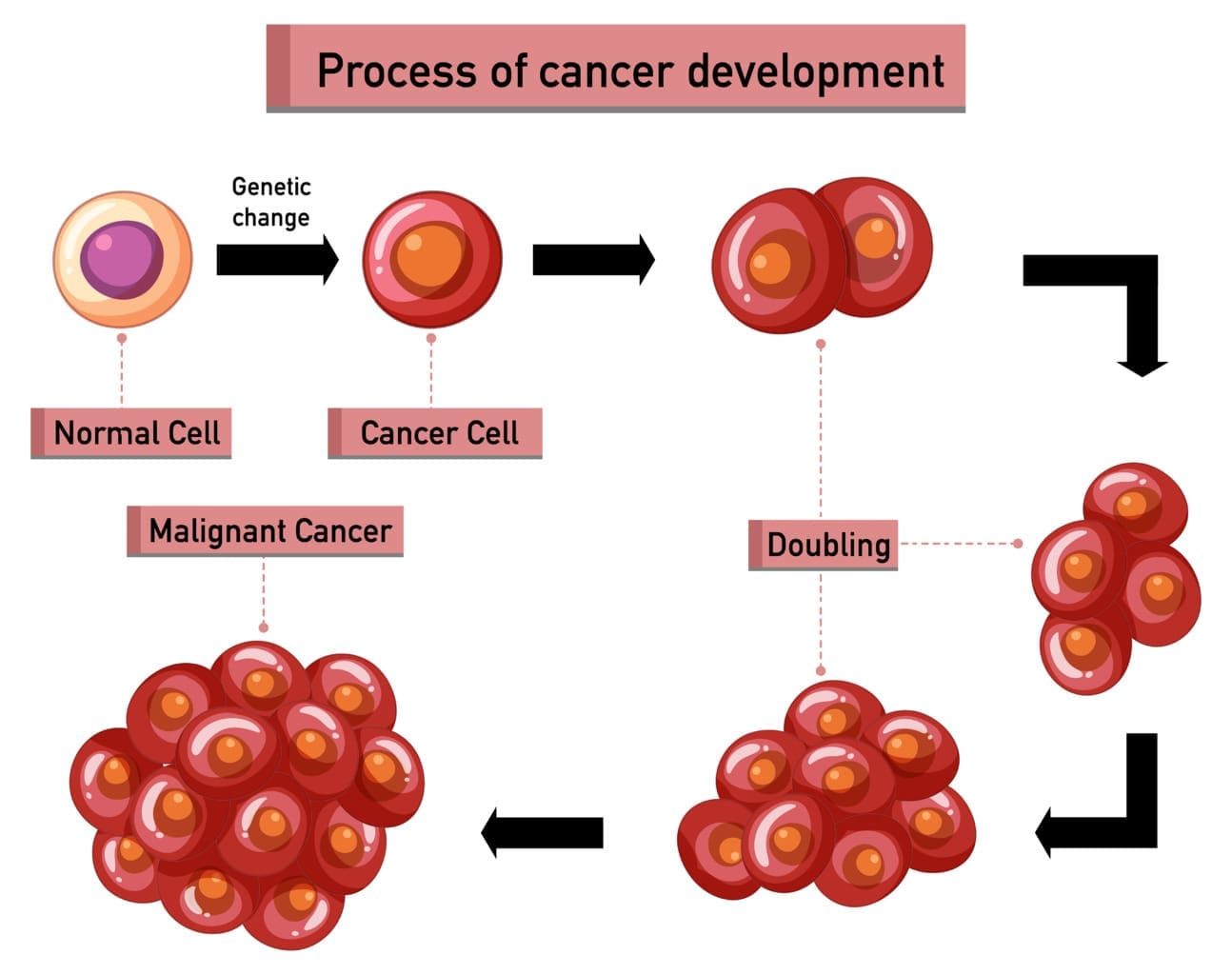
Potential Complications of Diverticulitis
It’s important to know about the possible complications of diverticulitis. If not treated right, diverticulitis can cause serious problems. We’ll look at two big issues: abscess formation and perforation of the colon.
Abscess Formation
An abscess is a pocket of pus in the colon or nearby tissues. Abscess formation is a serious complication of diverticulitis. Symptoms include severe pain, fever, and changes in bowel habits. A CT scan is often used to diagnose an abscess.
It’s key to treat abscesses quickly. This might mean antibiotics or a drainage procedure. If not treated, abscesses can cause more problems, like perforation or sepsis.
Perforation of the Colon
Perforation happens when a hole forms in the colon. This lets bacteria into the belly, causing peritonitis, a serious infection. Signs of perforation include severe pain, fever, and nausea. If you think you have perforation, get medical help right away.
Perforation is a medical emergency that needs quick surgery. It shows how important it is to manage diverticulitis well to avoid such problems.
A report from the Pennsylvania Health Care Cost Containment Council highlights the need to manage complications like abscesses and perforation. Knowing about these risks helps us take steps to prevent them and improve care.
- Watch for signs of abscess formation and perforation.
- Get medical help fast if you have severe symptoms.
- Listen to your healthcare provider’s advice on managing diverticulitis.
Preventing Hospitalization
To avoid hospital stays, it’s key to know how diet and lifestyle changes can help with diverticulitis. Making smart choices can greatly lower the risk of serious problems.
Dietary Changes to Manage Diverticulitis
Diet is very important in managing diverticulitis. Increasing fiber intake is often advised. This makes stool softer and reduces pressure on the diverticula. Foods high in fiber include fruits, veggies, and whole grains. Drinking plenty of water is also good.
- High-fiber foods: fruits, vegetables, whole grains
- Adequate hydration: water
It’s best to avoid processed meats and high-fat foods. They can make symptoms worse.
Lifestyle Modifications for Prevention
Along with diet changes, some lifestyle tweaks can prevent diverticulitis complications. Regular physical activity helps improve bowel movements and reduces pressure. Maintaining a healthy weight is also key, as extra weight can increase risk.
- Engage in regular physical activity.
- Maintain a healthy weight.
- Avoid smoking.
Dietary Component | Recommended Foods | Foods to Avoid |
Fiber Intake | Fruits, Vegetables, Whole Grains | Processed Foods, Low-Fiber Foods |
Hydration | Water | Caffeine, Alcohol (in excess) |
Fat Intake | Healthy Fats (e.g., Avocado, Nuts) | High-Fat Foods, Fried Foods |
Post-Hospital Care and Follow-Up
The journey to recovery doesn’t end when you leave the hospital. It’s just the start of a key phase in managing diverticulitis. After treatment, post-hospital care is vital for avoiding complications and ensuring a smooth recovery. This period is critical for your health and future well-being.
Importance of Timely Follow-Up
Follow-up appointments are key in post-hospital care. These visits let healthcare professionals check on your recovery and address any concerns. Timely intervention can greatly help prevent future episodes and complications. It’s important to schedule follow-up appointments as your healthcare provider advises to ensure a full recovery.
At these appointments, your healthcare team will evaluate your condition and possibly do more tests. They will also guide you on managing your recovery. It’s a chance for you to ask questions, report any symptoms, and get personalized advice on rehabilitation tips for your needs.
Rehabilitation and Recovery Tips
Recovering from diverticulitis needs a complete approach. This includes dietary changes, lifestyle adjustments, and following prescribed treatments. Here are some rehabilitation tips to help in your recovery:
- Start by adding low-fiber foods to your diet and gradually increase fiber as advised by your healthcare provider.
- Drink plenty of water all day to stay hydrated.
- Do gentle physical activity as recommended by your healthcare team to improve health and bowel function.
- Stick to your medication and tell your healthcare provider about any side effects or concerns.
By following these tips and keeping in touch with your healthcare team, you can manage the post-hospital phase well. This will help minimize complications and improve your recovery.
Long-Term Management Strategies
Managing diverticulitis well over time needs a full plan. This includes knowing the condition and having a good healthcare team. We’ll look at how to manage diverticulitis long-term. We’ll also talk about the differences between diverticulosis and diverticulitis and why a diverse healthcare team is key.
Understanding Diverticulosis vs. Diverticulitis
Diverticulosis and diverticulitis are closely related but different. Diverticulosis is when small pouches form in the colon wall. Diverticulitis happens when these pouches get inflamed or infected.
It’s important to know the difference to manage diverticulitis well. Diverticulosis might not cause symptoms, but diverticulitis can lead to severe pain, fever, and changes in bowel habits.
Building a Supportive Healthcare Team
a gastroenterologist, says, “A team approach to managing diverticulitis can greatly improve patient results. It’s important to work with healthcare providers who know the condition well.”
“A multidisciplinary approach to managing diverticulitis can significantly improve patient outcomes.”
Gastroenterologist
Conclusion: Knowing When to Act
It’s important to know when to seek medical help for diverticulitis. This knowledge helps manage the condition and avoid serious problems. By staying informed, you can take charge of your health and make better choices.
Empowering Patients with Knowledge
Being well-informed is essential in managing diverticulitis. Knowing the signs, understanding tests, and knowing treatment options boosts your confidence. Early detection of worsening symptoms can greatly improve your recovery.
Accessing Support and Resources
For those facing diverticulitis, having good resources is key. Gastroenterology clinics offer educational materials and support. Using these resources can deepen your understanding and help you manage the condition better.
FAQ
What are the signs that I should go to the hospital for diverticulitis?
If you have severe abdominal pain, keep vomiting, see blood in your stool, or have a high fever, go to the hospital right away. These signs mean you might have a serious case of diverticulitis that needs quick medical help.
How is diverticulitis diagnosed in the hospital?
Doctors use CT scans and lab tests like blood and stool samples to diagnose diverticulitis. These tests help figure out how bad the condition is and if there are any serious problems.
What treatment options are available for diverticulitis in the hospital?
In the hospital, treatments for diverticulitis might include pain and infection medicines. Sometimes, surgery is needed for severe cases or complications. We choose the best treatment for each patient based on their situation.
Can diverticulitis be managed without hospitalization?
Yes, sometimes diverticulitis can be treated without staying in the hospital. This might involve changing your diet and lifestyle. But, if your symptoms get worse or you have severe symptoms, you might need to go to the hospital to avoid serious problems.
What are the possible complications of diverticulitis?
Complications of diverticulitis can include abscesses, colon perforation, and severe infections. We watch patients closely for these signs and act quickly if they happen.
How can I prevent hospitalization for diverticulitis?
To avoid needing to go to the hospital for diverticulitis, manage your condition with diet and lifestyle changes. Keep an eye on your health and work with your healthcare team to catch any issues early.
What is the importance of follow-up care after being treated for diverticulitis in the hospital?
After being treated for diverticulitis in the hospital, follow-up care is key for recovery. We recommend regular check-ups to monitor your health, address any concerns, and prevent future problems.
How can I manage my recovery at home after being treated for diverticulitis?
To recover at home, follow a recommended diet, drink plenty of water, and rest well. We also advise on managing pain and watching for signs of complications or worsening symptoms.
What is the difference between diverticulosis and diverticulitis?
Diverticulosis is when you have diverticula in your colon. Diverticulitis is when these diverticula get inflamed or infected. Knowing the difference helps you manage your condition better.
Why is it important to have a supportive healthcare team for managing diverticulitis?
A supportive healthcare team is essential for managing diverticulitis. It ensures you get all the care and guidance you need during treatment and recovery. We work with patients to build a team that meets their unique needs.