When our immune system attacks the delicate tissues of our eyes, it can cause serious problems. Autoimmune eye inflammation, also known as uveitis, is a type of eye disease. It happens when the immune system mistakenly attacks the inside of the eye, causing inflammation.Discover the link between eye inflammation and autoimmune disease. We uncover the hidden causes and reveal the best treatment strategies.
Uveitis affects thousands of people every year. It’s a major cause of preventable blindness in adults who are working. We will look into what causes it and how it can be treated. This condition happens when the immune system attacks healthy tissue in the eye.
Key Takeaways
- Autoimmune eye inflammation, or uveitis, is a significant category of eye disease.
- The condition occurs when the immune system mistakenly attacks healthy eye tissue.
- Uveitis is a leading cause of preventable blindness in working-age adults.
- Understanding the causes and treatment options is key to managing the condition well.
- Approximately 30,000 new cases of uveitis are diagnosed annually.
Understanding Autoimmune Eye Inflammation
When the immune system attacks the eye by mistake, it can cause serious inflammation. This is called autoimmune eye inflammation or uveitis. It happens when the body sees the eye’s parts as foreign threats.
Definition and Basic Mechanisms
Autoimmune eye inflammation affects the uvea, which includes the iris, ciliary body, and choroid. This inflammation is caused by the immune system’s wrong response. It leads to autoimmune eye swelling and autoimmune disease eye inflammation.
The uvea is key to the eye’s structure. Its inflammation can cause serious problems, like vision loss if not treated.
Uveitis involves a complex mix of immune cells and cytokines. Normally, the body fights off pathogens. But in autoimmune diseases, it attacks the body’s own tissues, including the eye.
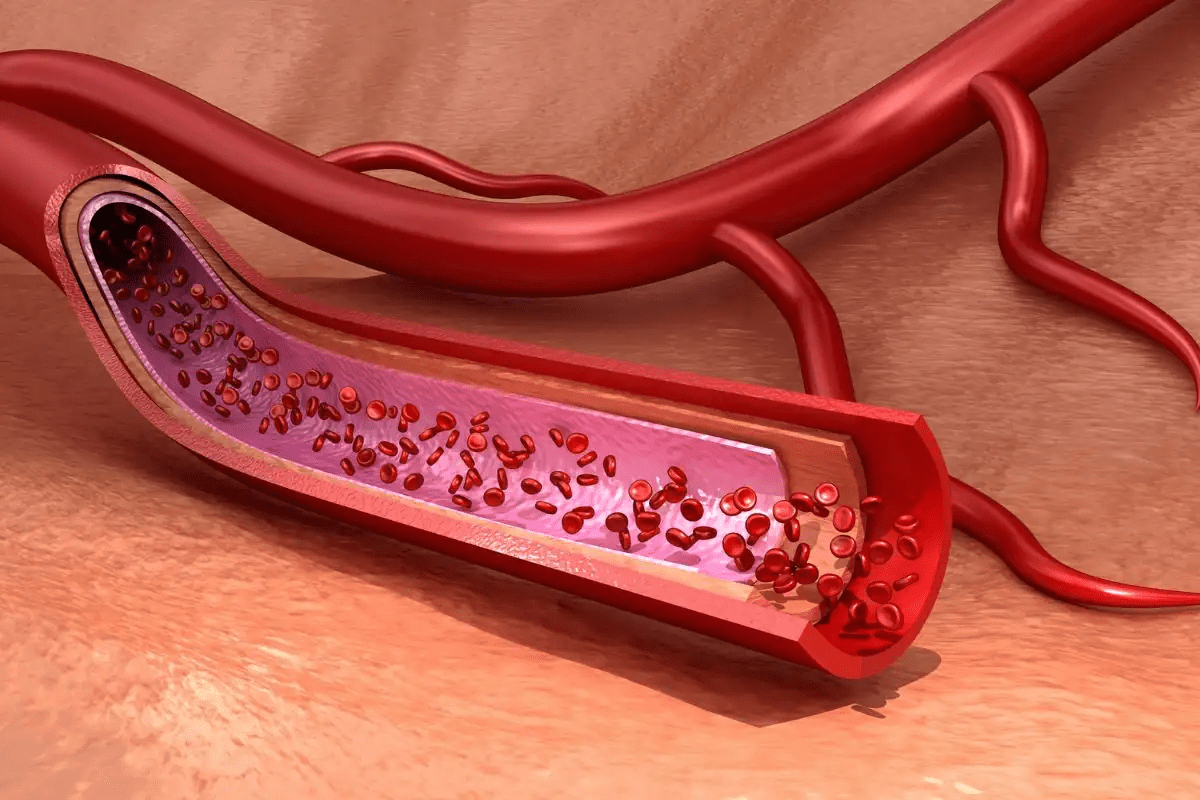
The Uvea: Primary Target of Inflammation
The uvea is the main target of inflammation in autoimmune eye inflammation. It has three main parts: the iris, ciliary body, and choroid. The iris is the colored part of the eye, the ciliary body makes fluid for the lens and cornea, and the choroid is a layer of blood vessels.
Inflammation of the uvea, or uveitis, can be caused by autoimmune disorders. Uveitis is a form of uveitis autoimmune disease. It happens when the immune system attacks the uvea, causing inflammation and serious eye damage.
Part of the Uvea | Function | Effect of Inflammation |
Iris | Controls the amount of light entering the eye | Inflammation can cause eye pain and sensitivity to light |
Ciliary Body | Produces fluid that nourishes the lens and cornea | Inflammation can lead to vision problems and eye discomfort |
Choroid | Layer of blood vessels between the sclera and retina | Inflammation can cause damage to the retina and affect vision |
Understanding the uvea’s structure and function is key to diagnosing and treating autoimmune eye inflammation. Recognizing uveitis signs and symptoms helps healthcare providers create effective treatment plans. This prevents long-term damage.
The Prevalence and Impact of Autoimmune Uveitis

Understanding autoimmune uveitis is key to better treatments. This condition, which causes inflammation in the uvea, is rare but serious. It affects public health a lot.
Statistical Overview and Epidemiology
Autoimmune uveitis is behind 70-90 percent of serious uveitis cases in rich countries. It’s caused by the body’s immune system attacking itself. About 38 cases of uveitis happen for every 100,000 people, making it rare.
Every year, around 30,000 new cases are found. This shows we need to spread the word and catch it early.
The disease often hits people under 40. This means we must find and treat it early to save their sight.
Demographics and Risk Factors
Studies have found who’s most at risk for autoimmune uveitis. It affects people of all ages but hits working-age folks hard. This can hurt their work and life quality.
Knowing who’s at risk helps doctors target their care. This way, we can help people with autoimmune uveitis more.
Key demographic factors include:
- Age: Typically diagnosed before the age of 40
- Geographic variations in prevalence
- Association with other autoimmune diseases
By understanding these, doctors can give better care. This improves life for those with autoimmune uveitis.
Types of Autoimmune Eye Inflammation
Autoimmune eye inflammation can show up in different ways. Each type has its own signs and needs special care. Doctors sort these conditions based on where in the eye they happen.
Anterior Uveitis
Anterior uveitis affects the front part of the uvea. This includes the iris and the ciliary body. It’s often linked to diseases like ankylosing spondylitis and rheumatoid arthritis. Symptoms include eye pain, redness, and light sensitivity.
Key features of anterior uveitis include:
- Inflammation of the iris and ciliary body
- Association with systemic autoimmune diseases
- Symptoms like pain, redness, and photophobia
Intermediate Uveitis
Intermediate uveitis causes inflammation in the vitreous humor and the peripheral retina. It’s sometimes linked to multiple sclerosis. People with this condition might see floaters and have blurry vision.
Notable aspects of intermediate uveitis:
- Inflammation mainly in the vitreous humor
- Possible link to multiple sclerosis
- Symptoms include floaters and vision problems
Posterior Uveitis and Panuveitis
Posterior uveitis affects the back of the eye, including the choroid and retina. Panuveitis, on the other hand, causes inflammation across all layers of the uvea. Both can lead to serious vision loss if not treated right.
Characteristics of posterior uveitis and panuveitis:
- Posterior uveitis involves the choroid and retina
- Panuveitis is a widespread inflammation across the uvea
- Risk of significant visual loss if untreated
Knowing about these different types of autoimmune eye inflammation is key. It helps doctors make the right diagnosis and treatment plan. Each type needs a specific approach to manage symptoms and avoid complications.
The Connection Between Eye Inflammation and Autoimmune Disease
It’s key to understand how autoimmune diseases and eye inflammation are connected. Many autoimmune conditions affect more than just their primary symptoms. They can also impact eye health significantly.
Rheumatoid Arthritis and Ocular Manifestations
Rheumatoid arthritis (RA) mainly affects joints but can also harm the eyes. Uveitis and scleritis are common eye problems linked to RA. We’ll look at how managing RA affects eye health and vice versa.
RA patients often need care from both rheumatologists and ophthalmologists. This team approach is vital for managing the disease well.
Systemic Lupus Erythematosus
Systemic Lupus Erythematosus (SLE) can affect many parts of the body, including the eyes. Ocular manifestations in SLE can vary from mild to severe. These include retinal vasculitis and optic neuritis. It’s important to catch these early for proper treatment.
Regular eye check-ups are essential for SLE patients. This helps catch any eye problems early on.
Multiple Sclerosis and Optic Neuritis
Multiple sclerosis (MS) is a disease that affects the central nervous system. It’s linked to optic neuritis, an inflammation of the optic nerve. This shows how closely neurological and eye health are connected.
Optic neuritis is a common first symptom of MS. Both neurologists and ophthalmologists need to be aware of this.
Ankylosing Spondylitis and Uveitis
Ankylosing spondylitis (AS) mainly affects the spine but can also lead to uveitis. The connection between AS and uveitis is clear, with HLA-B27 being a common risk factor for both.
Monitoring for uveitis in AS patients is critical. It affects their overall treatment plan.
The Immune System’s Role in Ocular Inflammation
Understanding how the immune system causes eye inflammation is key. The immune system protects us from harm. But, in autoimmune diseases, it fails.
Normally, it knows the difference between self and non-self. It fights off invaders but not our own cells. In autoimmunity, it attacks our own cells, including eye tissues.
Normal Immune Function vs. Autoimmunity
In a healthy person, the immune system is well-controlled. It doesn’t harm our own tissues. This control involves many immune cells and signaling molecules.
Autoimmune diseases happen when this control fails. The immune system then attacks our own cells. This is true for eye diseases too.
Specific Immune Mechanisms in Eye Inflammation
The immune system’s role in eye inflammation is complex. Autoreactive T cells mistakenly see eye tissues as foreign. Cytokines, like TNF-alpha, play a big role in inflammation.
- CD4+ T cells are important in the immune response, including in eye diseases.
- Cytokines like TNF-alpha are key in inflammation and are targets for treatments.
- The balance between pro-inflammatory and anti-inflammatory cytokines affects how much inflammation and damage there is.
Knowing these mechanisms helps us create better treatments. These treatments aim to control the immune response without weakening it too much.
By understanding the immune system’s role in eye inflammation, we can tackle autoimmune eye diseases better. We need precise treatments to help.
Symptoms and Warning Signs
It’s important to know the signs of autoimmune eye inflammation to get help quickly. This condition, known as uveitis, can cause serious problems if not treated fast.
Common Symptoms of Autoimmune Eye Inflammation
Symptoms of autoimmune eye inflammation can differ. But, they often include eye pain, redness, and light sensitivity. You might also see blurred vision, floaters, or have trouble seeing clearly.
Uveitis, a type of this condition, can make your eyes hurt and feel uncomfortable. How bad these symptoms are can depend on the type of uveitis and the person affected.
When to Seek Medical Attention
If you have sudden eye pain, vision changes, light sensitivity, or eye redness, see a doctor right away. Getting help early can stop serious issues like vision loss.
It’s key to know the warning signs and see an eye doctor if you notice anything odd. Getting help quickly can make a big difference in treating autoimmune eye inflammation.
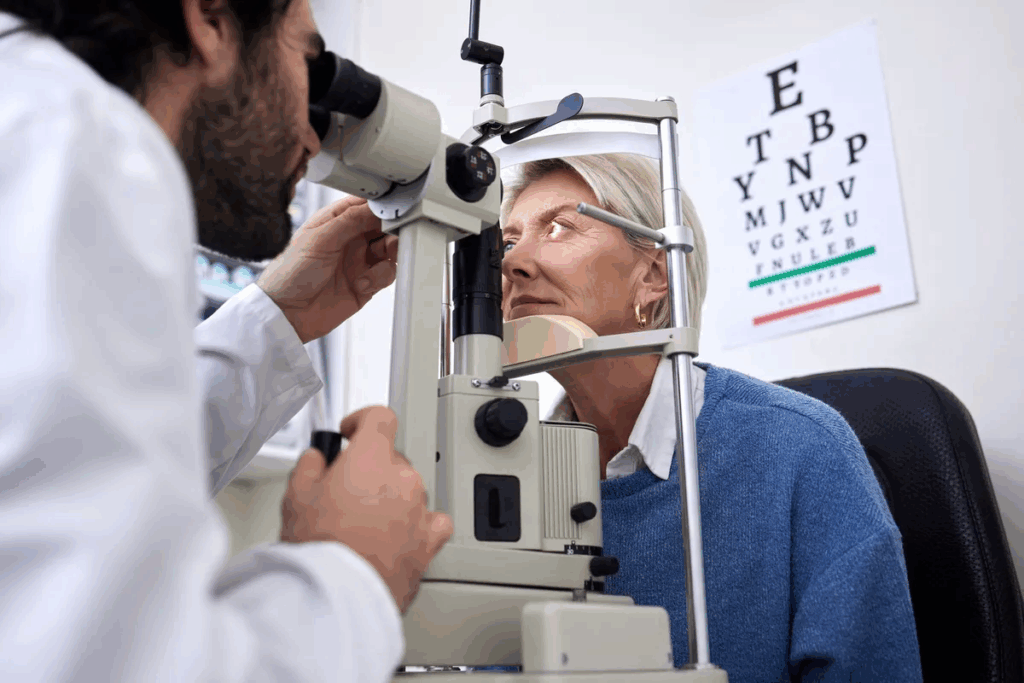
Diagnosis of Autoimmune Eye Disorders
Healthcare providers use many tools to diagnose autoimmune eye disorders. They do clinical exams and use advanced imaging. Accurate diagnosis is key for good treatment.
Clinical Examination Techniques
A detailed eye exam is the first step. It checks how well you see and the pressure in your eyes. It also looks at the front and back of your eyes.
Experts say a good exam is vital. It helps spot signs of uveitis and other eye problems.
The exam might show inflammation or other signs of disease. These clues help us decide what tests to do next.
Laboratory Tests and Imaging
Blood tests are important to confirm a diagnosis. They look for signs of inflammation or infections. Imaging like OCT and fluorescein angiography show detailed pictures of your eyes.
OCT can spot changes in the retina. Fluorescein angiography shows where there might be leaks or problems with blood flow. “New imaging has changed how we diagnose and treat eye diseases,” experts say.
Differential Diagnosis
It’s important to rule out other possible causes. Symptoms can look like other diseases. A detailed check helps find the right cause.
By looking at all the information, we can make a correct diagnosis. “Knowing the exact cause is the first step to treating eye diseases,” experts agree. This helps patients get the right care and see better.
Treatment Approaches for Autoimmune Eye Inflammation
There are many ways to treat autoimmune eye inflammation. We will look at these methods. They aim to reduce inflammation and prevent damage.
Corticosteroid Therapy
Corticosteroids are often the first choice for treating autoimmune eye inflammation. They help reduce inflammation and ease symptoms. Corticosteroid therapy can be applied topically, injected, or taken orally, depending on the inflammation’s severity and location.
Topical corticosteroids are used for anterior uveitis. Systemic corticosteroids are used for more severe cases or when the posterior segment is involved. But, long-term use can cause side effects like cataracts and increased eye pressure.
Immunosuppressive Medications
For long-term treatment or severe disease, immunosuppressive medications are used. These drugs reduce the immune system’s abnormal response, decreasing inflammation. Common drugs include methotrexate, azathioprine, and cyclosporine.
These medications are often used with corticosteroids. This allows for a lower steroid dose and reduces side effects. Regular monitoring is needed to check their effectiveness and safety.
Biologic Agents and Targeted Therapies
Biologic agents are a newer treatment for autoimmune eye inflammation. They target specific parts of the immune response, providing a more precise therapy. Examples include TNF-alpha inhibitors like adalimumab and infliximab.
Biologic agents are helpful for patients who don’t respond well to other treatments or have systemic autoimmune diseases. They have been shown to reduce inflammation and improve outcomes in uveitis patients.
Surgical Interventions
In some cases, surgical interventions are needed to manage complications or treat conditions caused by the disease or its treatment. Surgical options include cataract, glaucoma, and vitreoretinal surgeries.
The decision to have surgery depends on the condition’s severity, the patient’s health, and the surgery’s benefits and risks.
Complications and Prognosis
Untreated autoimmune uveitis can severely affect vision and quality of life. It’s important for patients and doctors to know the risks and outcomes. This helps in managing the condition better.
Potential Complications of Untreated Disease
Autoimmune uveitis can cause serious problems if not treated. These include:
- Vision loss, which can be permanent
- Cataract formation, potentially requiring surgical intervention
- Glaucoma, a condition that can cause optic nerve damage
- Retinal detachment, a medical emergency that can lead to blindness
- Cystoid macular edema, causing swelling in the macula
These issues highlight the need for early and effective treatment to avoid long-term damage.
Long-term Outlook and Quality of Life
The outlook for autoimmune uveitis patients depends on the disease’s type and severity. It also depends on how well they respond to treatment. With the right care, many patients can manage their symptoms well and live a good life.
Factor | Impact on Prognosis | Quality of Life Considerations |
Disease Severity | More severe disease often correlates with a poorer prognosis. | Frequent monitoring and aggressive treatment may be necessary. |
Response to Treatment | A good initial response to corticosteroids or immunosuppressives is a positive prognostic sign. | Effective treatment can significantly improve quality of life. |
Presence of Complications | Complications such as cataracts or glaucoma can complicate management and affect prognosis. | Early detection and treatment of complications are critical. |
Understanding the risks and factors that affect prognosis helps doctors create better treatment plans. This improves outcomes and enhances the quality of life for patients with autoimmune uveitis.
Living with Autoimmune Eye Disease
Living with autoimmune eye inflammation can be tough, but there are ways to manage it. We know it takes a full approach, including medicine, lifestyle changes, and learning about the disease.
Monitoring Disease Progression
Keeping an eye on the disease is key. Regular visits to the ophthalmologist help track the disease and adjust treatments. Spotting flare-ups early can make a big difference.
At these visits, patients might get tests like visual acuity tests and imaging studies. These help doctors see how the eyes are doing. Keeping a symptom journal can also help spot patterns and triggers.
Test Type | Purpose | Frequency |
Visual Acuity Test | Assess vision clarity | Every visit |
Imaging Studies (e.g., OCT) | Evaluate retinal health | As needed |
Ophthalmoscopy | Examine the retina and vitreous | Every visit |
Preventing Flare-Ups
Stopping flare-ups is a big part of managing the disease. This means sticking to your medicine and making lifestyle changes. Knowing and avoiding triggers can also help.
Some foods or environmental factors might set off flare-ups. Eating well and exercising regularly can help avoid these risks.
Lifestyle Modifications and Support Resources
Making lifestyle changes can really help manage the disease. This includes quitting smoking, staying at a healthy weight, and wearing sunglasses to protect your eyes.
Also, using support resources like patient groups and counseling can offer emotional support and advice. It helps with living with a chronic condition.
By using medicine, making lifestyle changes, and getting support, patients can live better with autoimmune eye disease.
Conclusion
Managing autoimmune eye inflammation, like uveitis, needs a full approach. This includes getting the right diagnosis, treatment, and ongoing care. We’ve looked into uveitis’s complexities, its link to autoimmune diseases, and why knowing its symptoms is key.
Patients and doctors can work together to create a treatment plan. This plan aims to improve life quality. It might include using corticosteroids, immunosuppressants, biologic agents, or surgery, based on the uveitis type and severity.
In short, autoimmune eye inflammation is a serious issue that needs quick action and proper care. Understanding and managing uveitis can lead to better outcomes for those affected.
FAQ
What is autoimmune eye inflammation?
Autoimmune eye inflammation, also known as uveitis, is when the immune system attacks healthy eye tissues. This leads to inflammation.
What are the symptoms of autoimmune eye inflammation?
Symptoms include eye pain, redness, sensitivity to light, and vision problems.
How is autoimmune eye inflammation diagnosed?
Doctors use eye exams, lab tests, and imaging to diagnose uveitis. They check for other conditions too.
What are the different types of autoimmune eye inflammation?
There are several types. Anterior, intermediate, posterior, and panuveitis affect different eye parts.
How is autoimmune eye inflammation treated?
Treatment includes corticosteroids, immunosuppressants, biologic agents, and surgery. It depends on the uveitis type and severity.
What are the possible complications of untreated autoimmune eye inflammation?
Untreated uveitis can cause vision loss, cataracts, and glaucoma.
Can autoimmune eye inflammation be associated with other autoimmune diseases?
Yes, it can be linked to diseases like rheumatoid arthritis, lupus, multiple sclerosis, and ankylosing spondylitis.
How can patients manage autoimmune eye disease effectively?
Effective management includes monitoring, preventing flare-ups, making lifestyle changes, and using support resources.
What is the long-term outlook for patients with autoimmune eye inflammation?
The outlook depends on disease severity and treatment success. Proper management can improve quality of life.
Are there any specific lifestyle changes that can help manage autoimmune eye inflammation?
Yes, lifestyle changes and support are key to managing the condition effectively.
What is uveitis autoimmune disease?
Uveitis autoimmune disease is when the immune system attacks the uvea. This leads to inflammation and complications.
How does the immune system contribute to autoimmune eye inflammation?
In autoimmune eye disease, the immune system sees healthy eye tissues as foreign. This causes inflammation and damage.
References
National Center for Biotechnology Information. Ocular Autoimmunity: Mechanisms and Threats to Vision. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4186974/