The immune system is meant to keep us safe. But sometimes, it goes wrong and attacks our own body parts. When it targets our eyes, it can lead to serious problems and even threaten our sight.Asking why does your immune system attack your eyes? We reveal the surprising reasons behind this alarming condition and what you can do.
Issues like uveitis, which is inflammation inside the eye, happen when the immune system mistakenly attacks healthy eye tissue. At Liv Hospital, we tackle the complex challenges of autoimmune eye diseases. We aim to save your vision.
Our eyes are very sensitive because of their unique tissues. These include the retina, optic nerve, uvea, and cornea. Knowing why the immune system attacks these areas is key to spotting problems early and treating them right away.
Key Takeaways
- The immune system can malfunction and target healthy eye tissue.
- Conditions like uveitis can cause inflammation inside the eye.
- Liv Hospital provides complete care for autoimmune eye conditions.
- Early detection and treatment are vital for keeping your vision safe.
- Specialized eye tissues are very vulnerable to immune system attacks.
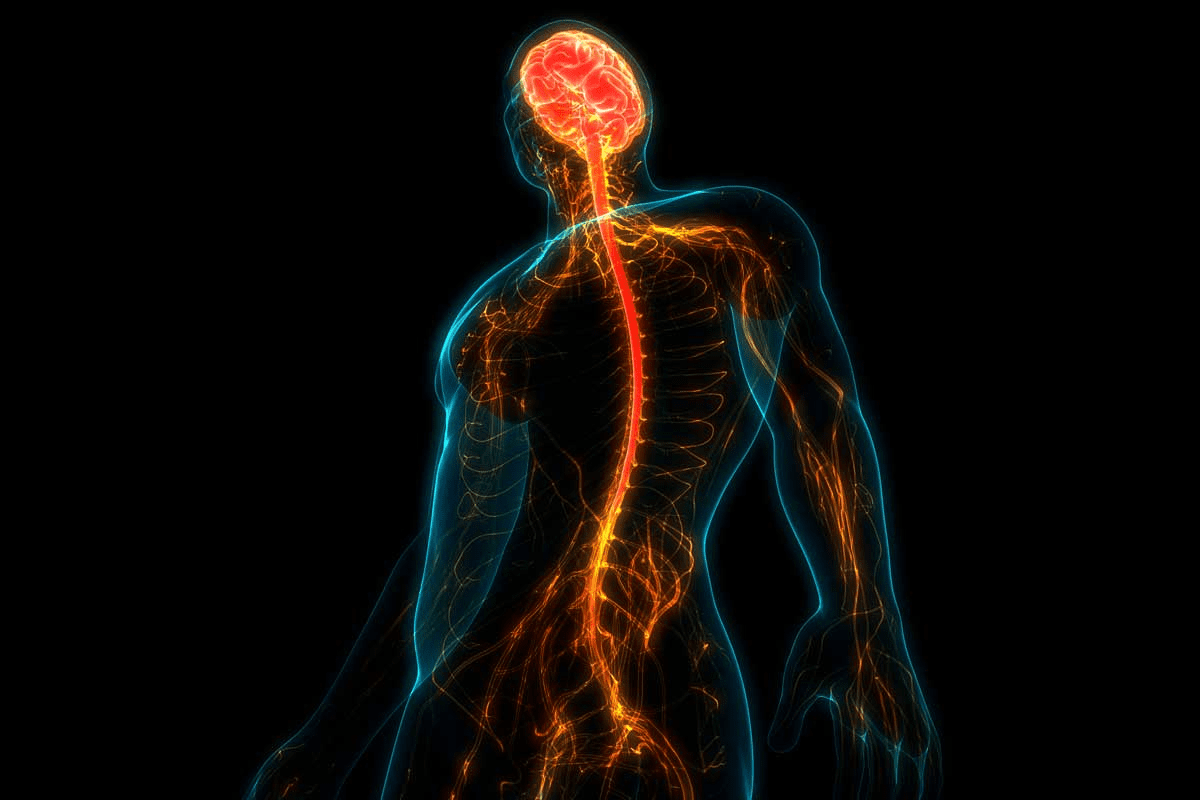
The Immune System: Your Body’s Defense Mechanism
The human immune system is a complex network that fights off infectious organisms. It’s key to keeping us healthy, including our eyes. A strong immune system helps protect us from infections by recognizing and fighting off pathogens.
The eyes have a special immune environment because of the blood-retinal barrier. This barrier is vital for keeping the eyes safe from the immune system’s attacks. We’ll look into how this barrier works and why it’s important for eye health.
How a Healthy Immune System Functions
A healthy immune system balances different cell types and signals. It knows the difference between self and non-self to fight off pathogens without harming our own tissues. This balance involves both innate and adaptive immunity.
Innate immunity is the first defense, using barriers like skin and mucous membranes. It also has cells like neutrophils and macrophages that quickly respond to infections.
Adaptive immunity is a more targeted response. It involves T cells and B cells that remember specific pathogens. This allows for a quicker and more effective response when we get infected again.
Component | Function |
Innate Immunity | First line of defense, physical barriers, and immediate response cells |
Adaptive Immunity | Specific response, T cells, and B cells, immunological memory |
The Blood-Retinal Barrier and Ocular Immune Privilege
The eyes are an immune-privileged site, protected from the immune system’s harmful responses. The blood-retinal barrier is key in keeping this privilege. It limits the exchange of molecules between the bloodstream and the retina.
This barrier is vital for stopping the immune system from attacking the retina. Such an attack could cause vision loss. The blood-retinal barrier, along with other mechanisms, helps keep the immune system and eyes in harmony.
Understanding how the immune system protects our eyes and the role of the blood-retinal barrier is essential. It shows the complex relationship between our immune system and eye health.
When Protection Turns to Attack: Understanding Autoimmunity

Our immune system is meant to protect us from harm. But sometimes, it gets confused and attacks our own cells. This is called autoimmunity, where the immune system mistakenly attacks the body’s own cells and tissues.
The Concept of Self vs. Non-Self Recognition
The immune system must know the difference between what’s us and what’s not. It uses complex systems to make this distinction. When it fails, the immune system may attack our own tissues, causing autoimmune diseases.
In the eyes, this means the immune system might see the eye’s tissues as foreign. This can lead to conditions where the immune system attacks the eyes. Understanding this is key to knowing why autoimmune conditions can harm our eyes.
Molecular Mimicry and Cross-Reactivity
Molecular mimicry happens when a foreign antigen looks like one of our proteins. This can trick the immune system into attacking our own tissues. Cross-reactivity is similar, where the immune system reacts to one antigen and also attacks another similar one.
In autoimmune eye diseases, these concepts play a big role. For example, an immune response to an infection might also target the retina or other eye tissues because of similarities.
The Role of Inflammation in Autoimmune Responses
Inflammation is a big part of autoimmune diseases, including those that affect the eyes. While some inflammation is normal, chronic inflammation is a sign of autoimmunity. This ongoing inflammation can damage tissues and make autoimmune conditions worse.
Mechanism | Description | Impact on Ocular Health |
Self vs. Non-Self Recognition Failure | Immune system fails to distinguish between body’s own cells and foreign invaders | Leads to autoimmune conditions affecting the eyes |
Molecular Mimicry | Foreign antigen shares similarities with body’s proteins, causing immune system to attack own tissues | Can trigger autoimmune eye diseases |
Chronic Inflammation | Ongoing inflammation due to autoimmune response | Results in tissue damage and disease progression |
Understanding these mechanisms is key to finding treatments for autoimmune eye conditions. By knowing how the immune system can turn against us, we can work to stop autoimmunity’s harm.
Why Does Your Immune System Attack Your Eyes?
The eye’s unique structure makes it a target for autoimmune diseases. Its complex tissues, like the retina and optic nerve, make it vulnerable. This includes the uvea and cornea too.
Unique Vulnerability of Ocular Tissues
Ocular tissues are highly specialized, making them vulnerable to autoimmune responses. For example, the retina has unique proteins. These proteins can be seen as foreign by the immune system, causing autoimmune retinopathy.
The uvea, the eye’s pigmented layer, can also be affected. This leads to uveitis, damaging the uvea and sometimes other parts of the eye. Uveitis can be chronic, causing vision problems.
Breakdown of Immune Privilege
The eye is an immune-privileged site. It has ways to avoid harmful immune responses. But, when this fails, autoimmune attacks can happen.
Genetic predispositions and environmental triggers can cause this breakdown. If the immune system doesn’t recognize the eye’s tissues, it may attack. This leads to autoimmune eye diseases.
Genetic and Environmental Triggers
Genetic and environmental factors are key in triggering autoimmune responses in the eyes. Some genetic markers increase the risk of autoimmune diseases. Environmental factors like infections or toxins can also trigger these diseases.
Trigger | Description | Potential Impact |
Genetic Predisposition | Inherited genetic markers that increase susceptibility to autoimmune diseases. | Increased risk of developing autoimmune eye conditions. |
Environmental Factors | Exposure to infections, toxins, or other external triggers. | Can initiate autoimmune responses in susceptible individuals. |
Understanding these triggers is key to treating autoimmune eye conditions. By knowing how genetics and environment interact, we can tackle these diseases better.
Common Autoimmune Conditions Affecting the Eyes
The immune system can sometimes go wrong and affect the eyes. This can lead to several eye-related autoimmune conditions. These conditions need careful management.
Uveitis: Inflammation of the Uveal Tract
Uveitis is an eye inflammation that affects the uveal tract. This includes the iris, ciliary body, and choroid. It can cause vision loss if not treated quickly.
Symptoms include eye pain, redness, sensitivity to light, and blurred vision. Uveitis is linked to diseases like rheumatoid arthritis or lupus.
Quick diagnosis and treatment are key to avoid complications. Treatment may include corticosteroids and immunosuppressive drugs to fight inflammation and protect tissues.
Autoimmune Retinopathy and Anti-Recoverin Antibodies
Autoimmune retinopathy occurs when the immune system attacks retinal proteins, like recoverin. This can cause vision loss. Symptoms include night blindness, loss of peripheral vision, and visual field defects.
Diagnosis involves finding autoantibodies against retinal proteins through tests. Treatment aims to reduce autoantibody production and save vision.
Neuromyelitis Optica and Optic Neuritis
Neuromyelitis optica (NMO) is a rare autoimmune disease that mainly affects the optic nerve and spinal cord. Optic neuritis, inflammation of the optic nerve, is a common symptom of NMO. Symptoms include severe vision loss, pain on eye movement, and visual field defects.
NMO is linked to aquaporin-4 antibodies in many patients. Treatment includes acute management of optic neuritis with corticosteroids and long-term immunosuppression to prevent relapses.
Susac Syndrome and Microangiopathy
Susac syndrome is a rare autoimmune condition. It is caused by anti-endothelial cell antibodies, leading to microangiopathy of the retina, brain, and inner ear. Symptoms include vision loss, hearing loss, and neurological deficits.
Early diagnosis is vital. Treatment usually involves immunosuppressive therapy to control the autoimmune response and prevent further damage.
The Cellular Mechanisms Behind Ocular Autoimmune Attacks
Ocular autoimmunity is complex, involving many immune parts and paths. When the immune system sees the eyes as invaders, it attacks. This can severely harm vision.
Autoantibodies Against Retinal Proteins
In autoimmune retinopathy, the immune system makes autoantibodies against retinal proteins like recoverin. These autoantibodies start a chain of events that damages the retina and causes vision loss. Finding and understanding these autoantibodies is key to treating this condition.
Some important points about autoantibodies in ocular autoimmunity are:
- Autoantibodies target specific retinal proteins.
- They activate immune cells that harm tissues.
- They disrupt normal retinal function by binding to proteins.
T-Cell Mediated Damage in Ocular Tissues
T-cells are key in ocular autoimmune diseases. They can directly harm ocular tissues or start other immune responses that damage tissues. How T-cells are activated and controlled affects how severe the disease is.
The main ways T-cells cause damage are:
- They can directly harm ocular tissue cells.
- They activate other immune cells that cause inflammation.
- They release cytokines that promote tissue damage and inflammation.
Complement System Activation and Tissue Destruction
The complement system is part of the innate immune response. In autoimmune diseases, it’s hijacked. In ocular autoimmunity, it’s activated, leading to tissue destruction. Understanding this is key to finding new treatments.
Important aspects of complement system activation in ocular autoimmunity include:
- It forms membrane attack complexes that damage tissues.
- It releases pro-inflammatory mediators that worsen inflammation.
- It offers targets for therapies to control activation.
By grasping the cellular mechanisms of ocular autoimmune attacks, we can create better treatments. This will help save vision and improve patient care.
Recognizing the Signs: Symptoms of Autoimmune Eye Conditions
Spotting the early signs of autoimmune eye conditions is key to better treatment. These conditions can cause mild discomfort or severe vision loss. We’ll look at common symptoms to help you know when to see a doctor.
Early Warning Signs: Redness, Pain, and Light Sensitivity
First signs often include redness, pain, and light sensitivity. These can make daily life hard. For example, uveitis can lead to pain, redness, and vision issues. If you notice these, see an eye doctor right away.
Progressive Symptoms: Blurry Vision and Vision Loss
As these conditions get worse, symptoms like blurry vision and vision loss can happen. Conditions like autoimmune retinopathy and neuromyelitis optica can cause serious vision problems if not treated. Regular eye exams are key to catching these early.
Dry Eyes and Surface Inflammation
Dry eyes are common in autoimmune diseases like Sjögren’s syndrome, lupus, and rheumatoid arthritis. Surface inflammation can also cause discomfort and vision issues. It’s important to manage these to avoid lasting damage.
Associated Systemic Symptoms
Eye conditions often come with symptoms from the autoimmune disease itself. This can include joint pain, skin rashes, and tiredness. Spotting these symptoms can help diagnose and treat the condition.
Symptom | Possible Autoimmune Condition | Impact on Vision |
Redness, Pain, Light Sensitivity | Uveitis | Blurry Vision, Vision Loss |
Dry Eyes | Sjögren’s Syndrome, Lupus, Rheumatoid Arthritis | Discomfort, Vision Disturbances |
Blurry Vision, Vision Loss | Autoimmune Retinopathy, Neuromyelitis Optica | Severe Vision Impairment |
Knowing the symptoms of autoimmune eye conditions is vital for early treatment. If you’re showing any of these signs, see an eye care professional for help.
Diagnosis and Testing for Ocular Autoimmune Disorders
Diagnosing autoimmune eye conditions requires a mix of clinical checks and advanced tests. Accurate diagnosis is key to start the right treatment and protect the eyes from more harm.
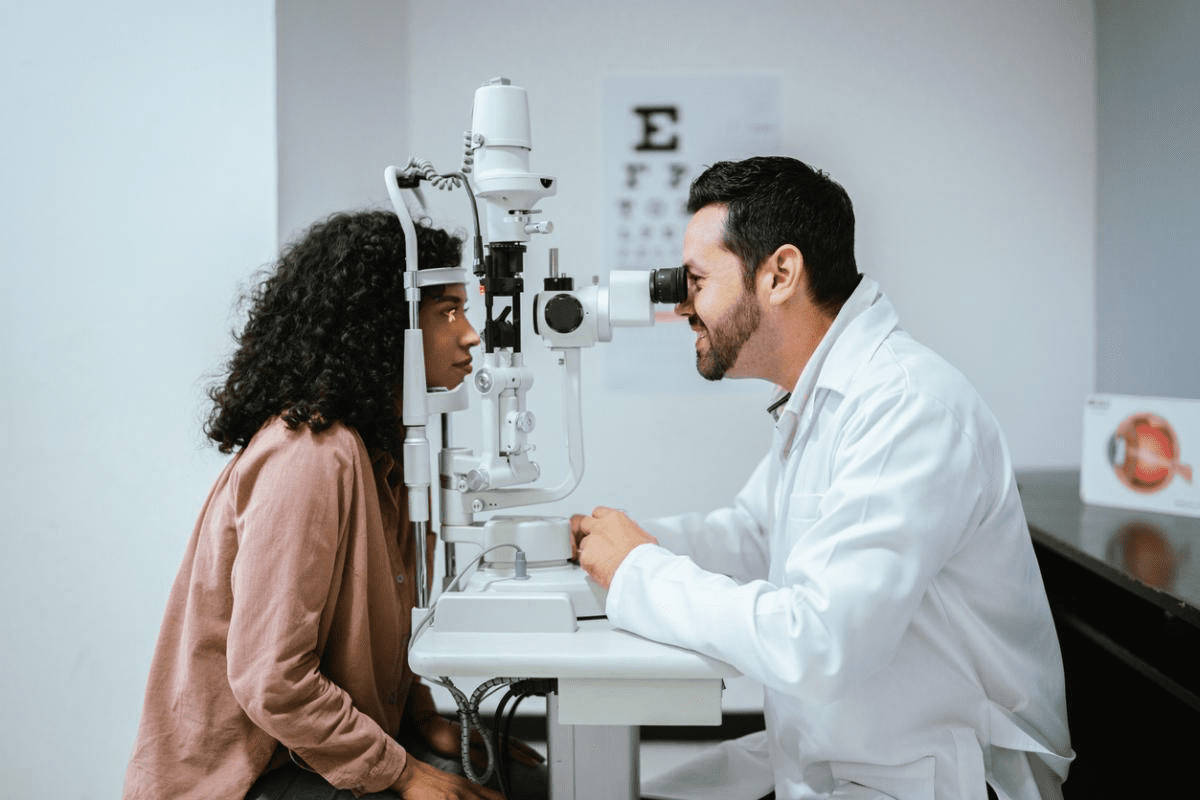
Clinical Examination Techniques
First, we do a detailed eye check to spot ocular autoimmune disorders. We use tests like visual acuity, slit-lamp exams, and fundoscopy. These help us see inflammation, damage, or other eye issues.
Visual acuity tests check how clear your vision is. Slit-lamp examinations let us closely look at the front part of the eye. Fundoscopy helps us see the back parts of the eye for any problems.
Laboratory Tests and Autoantibody Screening
Labs are key in diagnosing autoimmune eye issues. We test for specific autoantibodies linked to different autoimmune diseases. For example, tests for anti-recoverin antibodies can spot autoimmune retinopathy.
- Complete Blood Count (CBC) to check overall health and inflammation
- Erythrocyte Sedimentation Rate (ESR) or C-Reactive Protein (CRP) to measure inflammation
- Autoantibody tests to find specific autoimmune conditions
Imaging Studies and Functional Testing
Advanced imaging and functional tests give us detailed eye info. Tools like Optical Coherence Tomography (OCT), fluorescein angiography, and visual field tests help us see how much the eyes are affected and how the disease is progressing.
OCT is great for seeing the retina and spotting small changes. Fluorescein angiography shows us blood flow in the retina and finds leaks or ischemia.
Treatment Approaches for Immune-Mediated Eye Conditions
Managing immune-mediated eye conditions needs a mix of treatments. These conditions are complex, so we must tackle both symptoms and causes. We’ll look at different treatments, from common corticosteroids to new therapies.
Corticosteroids and Anti-Inflammatory Medications
Corticosteroids are often the first choice to fight inflammation. They can be applied directly to the eye, injected, or taken by mouth. But, using them for a long time can cause problems like cataracts and glaucoma.
Key considerations for corticosteroid treatment include:
- Monitoring for side effects
- Adjusting dosage as needed
- Using them with other treatments for better results
Immunosuppressive Therapies
For those who don’t get better with corticosteroids or need ongoing care, immunosuppressive therapies are an option. These treatments calm down the immune system, reducing inflammation and damage.
Examples of immunosuppressive agents used include:
- Methotrexate
- Cyclosporine
- Azathioprine
Biologics and Targeted Treatments
Biologic agents are a big step forward in treating immune-mediated eye conditions. They target specific parts of the immune system, making treatment more precise. Examples include TNF-alpha inhibitors and monoclonal antibodies.
- Less risk of side effects
- Specific action on immune pathways
- Potential for better results in tough cases
Emerging Therapies and Clinical Trials
The field of treating immune-mediated eye conditions is always changing. New therapies are being tested, and clinical trials are exploring new targets and ways to deliver treatments. This gives us hope for better and safer treatments in the future.
Some areas of research include:
- Gene therapy
- Stem cell therapy
- Novel biologic agents
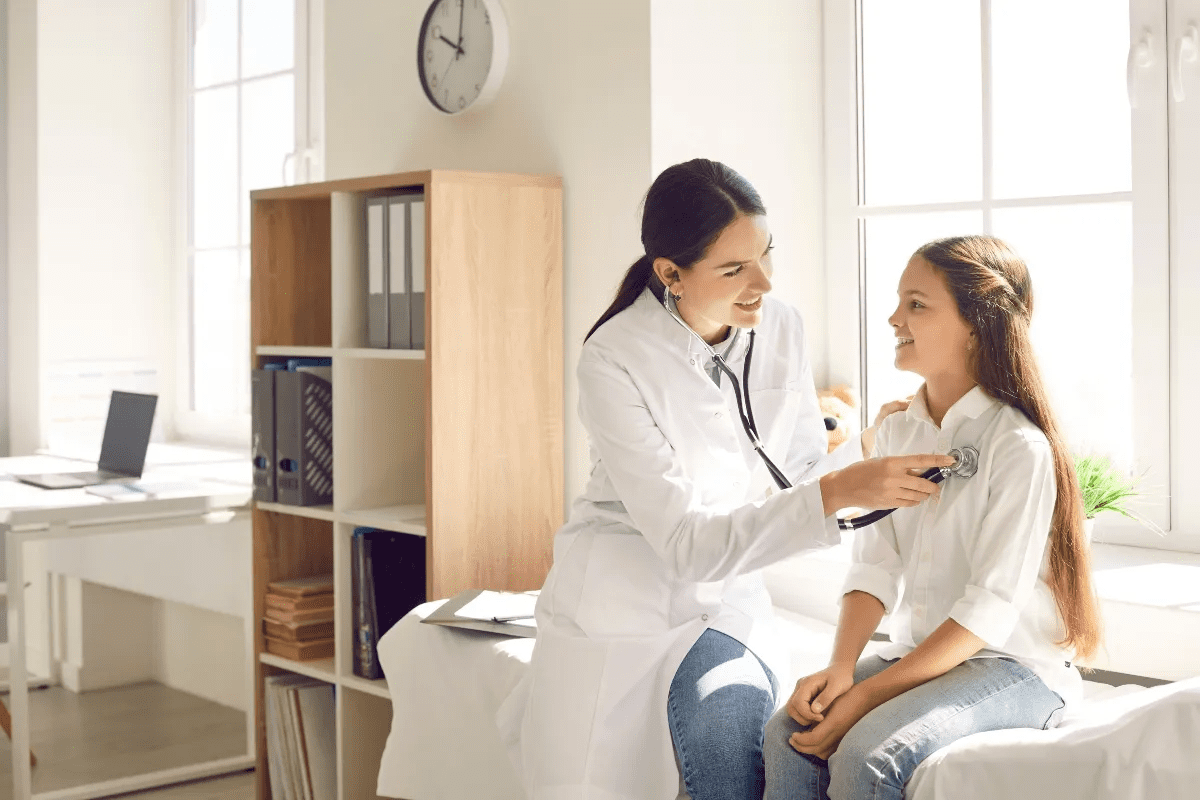
Conclusion: Living with and Managing Ocular Autoimmune Conditions
Understanding and managing ocular autoimmune conditions is key to keeping your vision and quality of life good. A complete approach is needed, including medical treatment, lifestyle changes, and regular check-ups.
Managing autoimmune eye conditions means creating a treatment plan that fits your situation. Doctors decide if treatment should target the whole body or just the eyes. Living with uveitis and other diseases requires working closely with doctors to adjust treatments.
Managing ocular autoimmune diseases is more than just treating symptoms. It’s about taking a holistic approach to health. This way, we can manage symptoms better, lower the risk of complications, and keep our vision.
FAQ
Does the immune system recognize the eyes as part of the body?
The immune system has a special relationship with the eyes. It’s because of the blood-retinal barrier, which keeps the eyes safe. But, in some cases, this barrier fails, and the immune system attacks the eyes.
Why does the immune system attack the eyes in autoimmune conditions?
The immune system goes after the eyes because of a mix of genetics and environment. Things like molecular mimicry and cross-reactivity also play a part.
What are the common autoimmune conditions that affect the eyes?
Autoimmune conditions like uveitis and autoimmune retinopathy can harm the eyes. Neuromyelitis optica and Susac syndrome are also common. Each one can cause serious vision problems.
How does the blood-retinal barrier contribute to ocular immune privilege?
The blood-retinal barrier helps keep the eyes safe from the immune system. This prevents autoimmune attacks on the eyes.
What are the symptoms of autoimmune eye conditions?
Symptoms include redness, pain, and sensitivity to light. You might also have dry eyes or blurry vision. Systemic symptoms can also occur, making a full medical check-up important.
How are ocular autoimmune disorders diagnosed?
Doctors use clinical exams, lab tests, and imaging to diagnose these conditions. They look for autoantibodies and check how much the eyes are affected.
What treatment options are available for immune-mediated eye conditions?
Treatments include corticosteroids and anti-inflammatory drugs. There are also immunosuppressives, biologics, and new therapies. The right treatment depends on the condition and its severity.
Can autoimmune eye conditions be managed effectively?
Yes, with the right treatment and care, symptoms can be managed. Regular check-ups and lifestyle changes are key to managing these conditions.
Does the immune system know about the eyes?
Normally, the immune system knows about the eyes but stays calm because of immune privilege. But, in autoimmune conditions, this calm is broken.
Can the immune system attack the eyeballs?
Yes, in autoimmune conditions, the immune system can attack the eyeballs. This leads to inflammation and damage to the eyes.
Why is immune privilege important for the eyes?
Immune privilege is key to protecting the eyes from autoimmune attacks. The eyes are very sensitive to inflammation and damage.
What happens if the immune system discovers the eyes?
If the immune system finds the eyes in autoimmunity, it may attack them. This can cause various autoimmune eye conditions.
How do autoantibodies contribute to ocular autoimmune conditions?
Autoantibodies against eye proteins are a big part of these conditions. They lead to tissue damage and vision loss.
Are there any new treatments on the horizon for autoimmune eye conditions?
Yes, new therapies and clinical trials offer hope for managing these conditions. They could be alternatives to current treatments.
References
National Center for Biotechnology Information. Ocular Autoimmunity: Mechanisms and Threats to Vision. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4186974/